Fig. 8.1
51-year-old lady with suspected gall bladder cancer. 18F–FDG PET/CT shows hypermetabolic mass with maxSUV 13.4 involving the fundus and body of the gall bladder (arrow in a–c). Histopathology post-radical cholecystectomy was adenocarcinoma of the GB

Fig. 8.2
18F–FDG PET/CT study of a 62-year-old lady showing hypermetabolic GB mass with loss of fat planes with the hepatic flexure of the colon (arrow in a–c) suggesting colonic infiltration

Fig. 8.3
55-year-old male, a case of GB carcinoma post-cholecystectomy. 18F–FDG PET/CT shows hypermetabolic metastatic supraclavicular, mediastinal nodes (block arrows in a), anterior abdominal wall deposits (arrow in a, b), and peritoneal deposits (curved arrow in a, c)

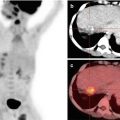
Fig. 8.4
18F–FDG PET/CT study of a 52-year-old lady with GB cancer. The study shows a hypermetabolic soft tissue mass (maxSUV 9.4) in the neck of the gall bladder (arrow in a–c) with bilateral intrahepatic biliary radical dilatation (curved arrow in b). The block arrow in d, e shows a focal hypermetabolic area in segment IVB, which was along the biliary radicals suggesting focal cholangitis (block arrow)
8.4 Role of FDG PET/CT in Prognostication
18F–FDG PET/CT has a potential role in prognostication of patients with GBC. It has the ability to gauge the aggressiveness of a tumor based on increased glucose uptake in cancer cells. Hwang et al. demonstrated that maximum SUV (maxSUV) values were prognostic and were an independent predictor of overall survival (OS). They showed that patients with maxSUV <6 had longer survival as compared to patients with maxSUV >6. Also in multivariate analysis, patients with lower maxSUV in the pretreatment study and nonmetastatic disease survived longer [9]. Volume-based metabolic parameters like metabolic tumor volume (MTV) and total lesion glycolysis (TLG) are also prognostic in GBC. In a study by Yoo et al., TLG of the primary GB mass was an independent prognosticator for OS [10]. Also patients with positive FDG PET/CT have a shorter median survival as compared to those with a negative PET/CT study [11].
8.5 Cholangiocarcinoma
Cholangiocarcinomas (CCA) are rare adenocarcinomas (>90%) arising from intrahepatic bile ducts, at the bifurcation of the hepatic ducts or from the distal common bile duct. The commonest form is that which arises from the bifurcation of the hepatic ducts (70%) and is called the Klatskin tumor. They are usually classified as intrahepatic or extrahepatic tumors. Intrahepatic can be further divided into mass forming, periductal, or intraductal based on the pattern of growth [12]. The patient usually is symptomless till an advanced stage is reached, and thus these are often diagnosed in late stage of the disease.
8.6 Role of Conventional Imaging Modalities
USG, CT, and MRI are the imaging modalities of choice for diagnosis and staging. These imaging modalities help in determining the size and extent of the tumor, biliary ductal dilatation, and involvement of regional lymph nodes [13–15]. Endoscopic retrograde cholangiopancreatography (ERCP) helps in obtaining brush cytology and biopsy.
8.7 Role of 18F–FDG PET in Diagnosis of the Primary Lesion
18F–FDG PET/CT has no advantage over these conventional imaging modalities in the diagnosis of CCA [16, 17]. The ability of PET/CT to detect a lesion depends on the location of the lesion. Studies have shown the highest sensitivity in the range of 91–95% and specificity ranging from 80 to 100% for intrahepatic bile duct lesions [18, 19]. This could be due to large tumor size of intrahepatic cholangiocarcinoma as compared to extrahepatic lesions. Another possibility is more accumulation of FDG in the malignant lesion as compared to the surrounding normal hepatocytes, where the turnover of 18F–FDG is faster [20].
The ability of FDG PET to detect cholangiocarcinoma also depends upon the pattern of growth of the lesion—whether mass forming or infiltrative. The sensitivity for detection of a lesion is highest for mass-forming/nodular lesion as compared to periductal or infiltrating lesions [21, 23, 24]. In a study by Anderson et al., they found a sensitivity of 85% for nodular lesions and only 18% for infiltrative lesions [21]. Hilar CCA are well demonstrated on FDG PET/CT and also help in demonstrating intrahepatic biliary dilatation (Figs. 8.5 and 8.6).



Fig. 8.5
18F–FDG PET/CT study of a 61-year-old male, diagnosed case of hilar cholangiocarcinoma. The study shows hypermetabolic mass at the confluence of right and left hepatic ducts (arrow in a–e) (maxSUV 13.51) with bilateral IHBR dilatation

Fig. 8.6




18F–FDG PET/CT study of a male patient, 57 years, a case of cholangiocarcinoma. Hypermetabolic mass is seen at the hilar confluence (arrow a–c) (maxSUV 10.38) with multiple enlarged periportal lymph nodes (block arrow) (maxSUV 8.1)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree