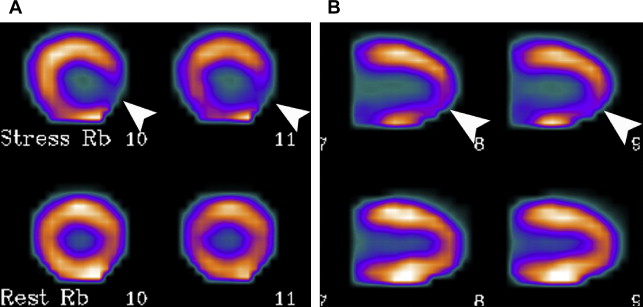
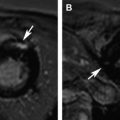
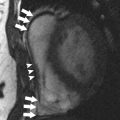
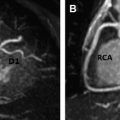
PET and magnetic resonance (MR) imaging have each become essential tools in the workup and management of cardiac patients. Combined PET/MR systems have recently been developed, allowing for single-session imaging using both modalities. This new technology holds great promise for cardiac applications given the different, yet complementary, information each modality provides. Research in this area is still nascent, although early studies have been promising. Combined PET/magnetic resonance (MR) systems are being developed and refined, with many commercially available systems now entering the market. Cardiac indications are potentially a fruitful area for this new technology, given how important PET and MR imaging each are in the workup and management of various cardiac diseases. Research to define the most effective use of this new hybrid technology is at a very early stage, although many preliminary studies have been promising. Several different imaging modalities have been used to study the heart, each with strengths and weaknesses. Two advanced imaging modalities, magnetic resonance (MR) imaging and PET, have enjoyed decades of clinical use, each evolving to become integral to the management of certain cardiac patients. MR imaging offers the ability to evaluate cardiac anatomy with high resolution and detailed tissue characterization. High temporal resolution cine image sequences have been developed, which capture high-resolution images of the heart throughout the cardiac cycle. Blood flow can be visualized and measured via velocity-encoded cine sequences. Postcontrast imaging adds an additional dimension, allowing for angiographic evaluation and assessment of early and late myocardial enhancement. Advanced MR techniques continue to be developed, including MR spectroscopy and sequences capable of measuring myocardial strain, T1 mapping, and so forth. The full range of cardiac MR sequences, all providing targeted information, is available without the use of ionizing radiation. Independently, PET has also become a modality ubiquitously used in cardiac imaging. Myocardial perfusion, historically evaluated via single-photon emission computed tomography (SPECT) tracers, can be assessed using PET agents. Rubidium-82 (Rb-82) and nitrogen-13 (N-13) ammonia allow for high-resolution imaging in a short acquisition time, and the possibility of quantitative measurements of coronary artery blood flow. These agents require an on-site generator or cyclotron, respectively, owing to the short half-life of these agents. Fluorine-18 [ 18 F]-based perfusion agents, which have a longer half-life and can be transported over greater distances, are in late-stage clinical trials. An approved 18 F perfusion agent could potentially result in PET replacing SPECT as the first-line modality for imaging myocardial perfusion. 18 F tagged to glucose ([ 18 F]–fluorodeoxyglucose [FDG]) has been used to evaluate the myocardium in several settings, including conditions involving inflammation of the myocardium. PET/computed tomography (CT) and SPECT/CT hybrid technologies have demonstrated the power of hybrid nuclear medicine imaging, with PET/CT in particular revolutionizing oncologic imaging. MR has several advantages over CT, making it potentially an excellent complement to the molecular information provided by PET, including excellent soft-tissue contrast, advanced functional techniques, and lack of ionization radiation. Combined PET/MR hybrid systems, however, have been an elusive technological goal until recently. MR imaging requires a bulky electromagnet and a plethora of electronics while PET cameras require a large array of sensitive detectors. The immense technological limitations of merging these technologies have finally been overcome in commercially viable scanners. The clinical value of PET/MR as a hybrid technology has only limitedly been evaluated thus far. The published literature regarding this technology for cardiac indications, in particular, is somewhat limited. Cardiac indications would prima facie seem like a fruitful area, given the unique and complementary strengths of each modality individually. In its simplest form, PET/MR could offer “one-stop shop” imaging modality for patients in whom PET and MR studies are separately indicated. For indications whereby acquiring both sets of images could theoretically be complementary, though not currently the standard of care, the new-found ease of acquiring both sets of images via hybrid scanners may result in a hybrid evaluation becoming the new standard. Finally, future research may determine ways to more deeply integrate the information obtained from each modality, resulting in new levels of diagnostic information. This article reviews of the current state of PET/MR technology, followed by a brief overview of cardiac indications for which PET/MR may hold great promise. Several technical challenges had to be overcome in designing commercially viable PET/MR imaging systems. A variety of solutions have been developed. The most straightforward solution, a sequential system, involves the installation of a PET/CT scanner and an MR scanner adjacent to each other, in line, connected by a single patient table. Sequential systems can also be installed with the 2 scanners in separate rooms, joined by a table system that spans the 2 rooms. Both of these designs require relatively minimal changes to the underlying scanners, although they require large installation footprints. In addition, a truly simultaneous acquisition of PET and MR data is not possible. The most integrated of the PET/MR designs is a concurrent system, in which the PET and MR components are physically combined in one scanner with a single gantry ( Fig. 1 ). This design involves a significant redesign of both the MR and PET hardware, most notably redesigning the MR hardware to make room for the PET and altering the PET detectors to become less sensitive to the MR scanner’s magnetic fields. Fully integrated systems have smaller footprints, and allow for the simultaneous acquisition of PET and MR data. Simultaneous image acquisition allows for the most flexibility in designing optimal imaging studies. PET/MR systems must have a mechanism to address attenuation correction, another major obstacle faced when developing these systems for clinical use. PET-only scanners and PET/CT systems use built-in radionuclide sources and CT, respectively, to create attenuation maps; neither technology is available in PET/MR systems. Several methods to address attenuation correction have been studied including template-based methods, atlas-based methods, and approaches based on MR image segmentation, and PET emission. Future studies will likely determine which approach is the most optimal. Hybrid PET studies are limited by patient motion. First, patient motion can result in misregistration between the anatomic and PET images. With potentially longer acquisition times, PET/MR may suffer from more misregistration issues in comparison with PET/CT. Second, patient motion can degrade the PET images themselves, given that PET images are acquired over multiple minutes per imaging bed. This limitation is particularly problematic when imaging the heart because of cardiac and respiratory motion, which can result in 4.9 to 9 mm of movement. PET/MR systems, however, unlike PET/CT systems, have the potential to correct PET data for patient motion. Cine MR imaging can demonstrate the full range of cardiac and respiratory motion, thereby allowing for a map to be created that can be applied to the raw PET data to correct for motion. The evaluation of cardiac tumors may be the most straightforward potential application of combined PET/MR scanners. CT is fairly limited in the evaluation of cardiac tumors, whereas MR imaging provides far more detail with regard to tissue characterization and the evaluation of tissue planes. In the case of malignant cardiac tumors, PET is often indicated for staging purposes, owing to the improved sensitivity of PET for metastatic disease in comparison with anatomic imaging alone. PET is also often used for the evaluation of treatment effectiveness and for surveillance. When both anatomic and metabolic imaging is indicated in the evaluation of a cardiac tumor, PET/MR may be superior to PET/CT. The primary tumor almost certainly would be more clearly demonstrated by MR imaging, and even in the evaluation for nodal and metastatic disease, PET/MR would likely be similar or superior to PET/CT. Although this supposition has not specifically assessed for cardiac malignancies, several studies have reported on the value of PET/MR in comparison with PET/CT for a variety of other tumors, including lung cancer. One notable weakness of PET/MR is in the evaluation of the lungs. The extent of patients’ coronary artery disease (CAD) can be evaluated by cardiac MR imaging, although the modality is not considered first line for this indication. First-pass perfusion with gadolinium can demonstrate perfusion defects at stress and rest, analogous to nuclear perfusion studies. Direct coronary artery imaging is also possible by MR imaging, although coronary CT angiography is currently the noninvasive gold standard owing to its high resolution and fast acquisition times. Cardiac MR imaging is more commonly used in the evaluation of myocardial infarctions. Late gadolinium enhancement (LGE) is demonstrated in acute and chronic infarctions, with the contrast being retained in the expanded extracellular in necrotic myocardium early and in regions of fibrosis later. Myocardial perfusion with PET tracers such as N-13 ammonia and Rb-82 is used more commonly than MR imaging to evaluate for CAD ( Fig. 2 ). PET perfusion studies have high sensitivity and specificity for the evaluation of obstructive CAD, and the PET data can also be processed to quantify coronary artery blood flow. This assessment is of particular value in patients with balanced ischemia, which can be underappreciated on visual evaluation.
Key points
Introduction
Instrumentation

Cardiac tumors
Myocardial ischemia and infarction