Anatomic variants
- ◼
Accessory spleen: very common. Typically near spleen. Can be intrapancreatic. Can be mistaken for a mass. Should look like spleen on all imaging sequences.
- ◼
Duplicated renal collecting system: prone to obstruct/reflux. Has surgical implications.
- ◼
Prominent column of Bertin: mimics focal renal mass. Has similar echogenicity, density, and magnetic resonance imaging (MRI) signal intensity to normal renal cortex.
- ◼
Pancreas divisum: no ventral/dorsal pancreatic fusion. Predisposes to pancreatitis.
- ◼
Pancreatic cleft: fat between normal pancreatic lobulations mimics a mass.
- ◼
Chilaiditi sign: colonic hepatic flexure interposed between the liver and the ventral abdominal wall can mimic intraperitoneal free air on radiograph.
- ◼
Inferior vena cava (IVC) pseudolipoma: retroperitoneal fat protrudes into the IVC near the cavoatrial junction mimicking a lipoma or thrombus ( Fig. 39.1 ).

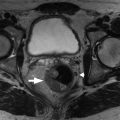
Fig. 39.1
Inferior vena cava pseudolipoma. A, Axial contrast enhanced abdominopelvic computed tomography image shows a fat attenuation filling defect ( arrow ) in the inferior vena cava at the diaphragm. This finding should not be mistaken for nonocclusive thrombus or a fat containing mass, such as lipoma. B, The coronal reformatted image shows that the lesion ( arrow ) is retroperitoneal fat protruding into the vessel, a benign finding.
- ◼
Variant hepatic arterial anatomy: includes accessory (extra) and replaced (arising from the wrong place) arterial anatomy. Crucial for liver and pancreas surgical planning.
- ◼
Duplicated IVC: common iliac veins do not join. Left common iliac vein commonly drains to the left renal vein. Affects optimal IVC filter placement.
- ◼
Prominent diaphragmatic slip: mimics a focal mass along the liver surface.
- ◼
Pseudolipoma of Glisson’s capsule: a piece of colonic epiploic fat located ectopically along the liver capsule.
- ◼
Diaphragmatic crus versus retroperitoneal lymphadenopathy: view multiple contiguous axial slices or orthogonal planes (coronal/sagittal) to distinguish.
- ◼
Limbus vertebra: well corticated triangular osseous fragment at the anterosuperior corner of a lumbar vertebra resulting from intravertebral herniation of the nucleus pulposus. Mimics a fracture fragment, which would not be well corticated.
- ◼
Cisterna chyli: normal fluid-filled tubular lymphatic structure in the right retrocrural space. No arterial or portal venous phase enhancement. Mimics a mass or lymph node.
Techniques and modality-specific pitfalls
Radiography
- ◼
Misplaced nasogastric tube: beware of the misplaced tube that is at the margin or beyond the field of view. If one tube is in place, consider that a second tube may be misplaced.
- ◼
Intraperitoneal free air can be challenging to detect on supine radiograph. Rigler sign, air on both sides of the bowel wall, can be helpful; however, dilated air-filled loops of bowel closely opposed to each other can mimic this appearance.
Ultrasonography
- ◼
Ultrasound settings: adjustment of numerous settings (gain, focal zone, depth, time gain compensation…) can have dramatic effects on image quality, which can mask lesions or create pseudolesions ( Fig. 39.2 ).

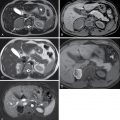
Fig. 39.2
Transjugular intrahepatic portosystemic shunt ( TIPS ) thrombosis. A, B-mode and color Doppler ultrasound image showing TIPS stent ( arrow ) with apparent internal color flow. Diffuse background color signal should raise concern that this flow is artifactual. B, Contrast enhanced computed tomography shows absent enhancement within the TIPS stent ( arrow ) and extension of thrombus into the inferior vena cava ( small arrowhead ). C, Digital subtraction angiogram confirms TIPS occlusion ( arrow ) and collateral vessel ( arrowheads ) formation.
- ◼
Mirror artifact: a strong reflector (i.e., the diaphragm) creates a false duplicate image of an abdominal structure in the lung. An echogenic liver lesion may be seen in the liver and the lung. Correctly identify the artifact to avoid misdiagnosing a lung mass.
Computed tomography
- ◼
Enhancement versus intrinsically hyperdense: cannot distinguish hyperdense renal cyst from enhancing renal mass or hyperdense ingested enteric material from contrast extravasation. If available, a precontrast series is helpful (similar problem affects MRI).
- ◼
Liver metastases with background steatosis: low intrinsic background liver attenuation reduces conspicuity or totally obscures liver metastases. In severe hepatic steatosis, metastases appear hyperenhancing to background low attenuation liver.
- ◼
Osseous metastasis pseudoprogression: enlarging sclerotic lesions are common after chemotherapy. Reflects treated metastases or progression. Imaging cannot distinguish.
- ◼
Vascular mixing artifacts mimicking thrombosis.
- ◼
Portal vein: on early postcontrast images, contrast opacified splenic venous blood can mix with nonopacified blood from the superior mesenteric vein.
- ◼
IVC: on early postcontrast images, contrast opacified renal vein blood can mix with nonopacified infrarenal IVC blood.
- ◼
- ◼
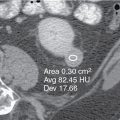
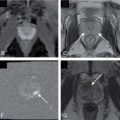
Bladder is filled with contrast on a noncontrast computed tomography (CT): consider excreted iodinated contrast from prior CT (perhaps at a different institution), excreted iodinated contrast from nonradiology procedure (coronary angiography), or excreted gadolinium from prior MRI. The excreted contrast can mimic renal stones ( Fig. 39.3 ).

Fig. 39.3
Excreted contrast mimicking renal stones. A 48-year-old woman with left flank pain underwent noncontrast computed tomography (CT) to assess for nephrolithiasis. Coronal reformation shows scattered hyperdensities in the bilateral upper renal poles ( arrows ), which should be recognized as excreted contrast material as the ureters ( long arrows ) are completely opacified. Search of the medical record confirmed that the patient underwent gadolinium enhanced breast magnetic resonance imaging 30 minutes before the CT. Excreted gadolinium, like iodine, is hyperdense. Epiploic appendagitis ( arrowheads ) was identified as the likely source of pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree