Many of the current guidelines for the management of carotid atherosclerosis are based on clinical trial findings published more than 2 decades ago. The lack of plaque information in clinical decision making represents a major shortcoming and highlights the need for contemporary trials based on characteristics of the atherosclerotic lesion itself, rather than luminal stenosis alone. This article summarizes the major dilemmas clinicians face in current practice, and discusses the rationale and evidence that plaque imaging may help to address these challenges and optimize the clinical management of carotid artery disease in the future.
Key points
- •
Advancements in optimal medical therapy, comprising antiplatelet agents, statin therapy, and aggressive risk factor control, have substantially reduced the risk of stroke in individuals with carotid artery disease.
- •
Compared with the current clinical standard of attributing risk based on carotid stenosis, plaque imaging may be better able to stratify the risk for stroke, and identify those most likely to benefit from carotid endarterectomy (CEA) and carotid artery stenting (CAS).
- •
Although CAS is considered as an alternative to CEA, it currently has higher rates of periprocedural stroke and clinically silent hemispheric infarction. Preliminary results suggest that vessel wall imaging of plaque morphology, composition, and activity may be beneficial in planning CAS procedures, and thereby reduce periprocedural stroke.
- •
While evidence is increasing, larger outcome studies and randomized clinical trials are needed to confirm the value of carotid plaque imaging in deciding between optimal medical therapy, carotid endarterectomy, and CAS.
Current clinical challenges
Prevalence of Carotid Artery Disease
Carotid artery disease, a local manifestation of systemic atherosclerosis, is not an uncommon finding in clinical practice. Indeed, a recent study pooling individual participant data from 4 large population-based studies estimated that the prevalence of asymptomatic moderate carotid stenosis, defined as 50% or more based on duplex ultrasonography, was as high as 7.5% in the general population depending on subjects’ age and sex. Specifically, 2.3% of men and 2.0% women in their 60s had carotid stenosis on ultrasonographic examination, which increased to 7.5% and 5.0% for individuals aged 80 years or older. In subgroups with cardiovascular risk factors or those with established coronary or peripheral artery disease, the prevalence of carotid stenosis is increased by severalfold compared with the general population.
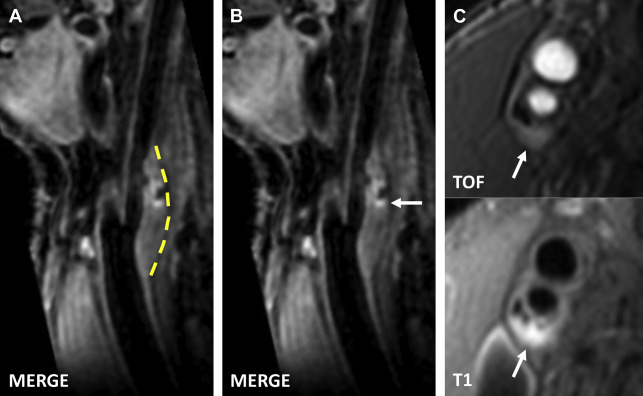
In addition, the prevalence of carotid artery disease that is significant, from a histopathologic point of view, may be underestimated. Nonstenotic or minimally stenotic carotid plaques can harbor substantial amounts of lipid and necrotic debris as a result of outward remodeling and the geometry of the carotid bulb. Furthermore, high-risk plaque features such as intraplaque hemorrhage (IPH), thin or ruptured fibrous cap, and plaque inflammation have been found in carotid plaques that are otherwise morphologically indistinct ( Fig. 1 ). In a 2008 study, 192 subjects underwent ultrasonography to quantify the degree of carotid stenosis, and MR imaging to identify the presence of complex plaques. Complex plaques were defined as having IPH or luminal surface defect on multicontrast MR images and were more frequently found in plaques with higher grades of stenosis. Of note, however, complex plaques were detected in 21.7% of arteries with only 16% to 49% luminal stenosis. Increasingly, the advent of improved techniques for vessel wall imaging demonstrates that diagnostic imaging methods that only measure stenosis underestimate plaque burden, plaque complexity, and, hence, the true prevalence of histologically significant carotid artery disease.
Clinical Outcomes with Medical Therapy Alone
Most carotid plaques have a relatively benign clinical course. However, once carotid artery disease becomes symptomatic, it often leads to disabling or devastating stroke without preceding signs. In the Asymptomatic Carotid Surgery Trial (ACST), half of the ipsilateral ischemic strokes in patients with asymptomatic carotid stenosis greater than 60% were disabling or fatal. Carotid artery disease is a major source of ischemic stroke, accounting for approximately 15% of the 795,000 incident strokes that occur annually in the United States. Less known is the role of nonstenotic but high-risk carotid plaques in cryptogenic strokes, of which a significant portion may be attributable to large-artery atherosclerosis, as discussed elsewhere in this issue.
Medical therapy plays a pivotal role in the primary and secondary prevention of ischemic strokes ascribed to carotid artery disease. The benefit of aspirin has long been recognized, and it is currently listed as a class I recommendation in guidelines for the management of asymptomatic and symptomatic carotid artery disease. Multiple clinical trials have established the efficacy of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) in reducing the incidence of major cardiovascular events and stroke, which is proportional to individuals’ baseline risk and absolute reduction in low-density lipoprotein cholesterol. Annual event rates for recurrent strokes from all sources have decreased from 8.7% in the 1960s to 4.98% in the 2000s, in part attributed to more prevalent use of statins along with improved profiles in blood pressure, smoking, and antithrombotic agents. In current guidelines, optimal medical therapy including aspirin and statin use, synergistic control of vascular risk factors, and lifestyle intervention forms the foundation of clinical management.
Carotid Endarterectomy
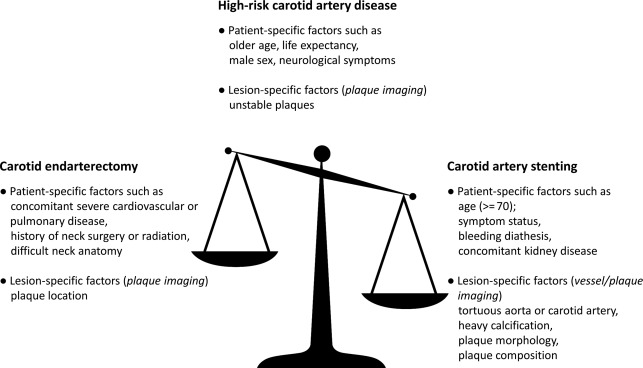
Excision of the culprit carotid plaque can offer long-term benefits in selected patients. To ensure net benefit on an individual basis, the evaluation of operative risk and future stroke risk must be carefully compared ( Fig. 2 ).
Symptomatic carotid artery disease
The North American Symptomatic Carotid Endarterectomy Trial compared carotid endarterectomy with medical therapy alone in patients with carotid artery disease and transient ischemic attack (TIA) or nondisabling stroke in the previous 180 days. Carotid stenosis, as assessed on digital subtraction angiography, ranged from mild (<50%) to severe (≥70%). Net benefit was seen most robustly in the group with severe stenosis, whereas patients with mild stenosis did not have a significant reduction in 5-year rate of ipsilateral stroke.
Asymptomatic carotid artery disease
Earlier randomized trials demonstrated smaller but statistically significant benefit from CEA in asymptomatic patients with high-grade carotid stenosis, as shown in the Asymptomatic Carotid Atherosclerosis Study and the ACST study.
However, the major clinical trials comparing CEA with medical therapy alone were conducted decades ago. Substantial advancements in medical therapy have been associated with progressive reduction in the risk for stroke. Most recent studies have reported an annual stroke rate of less than 1%. In 2009, Abbott performed a systematic review and analysis of published data on stroke risk associated with asymptomatic severe carotid stenosis. She found a progressive decrease in reported stroke rate with an average annual stroke risk estimated to be as low as those of the CEA arms in randomized trials performed before 2003. As the decision to proceed with surgical intervention must balance periprocedural risk and long-term event-free benefit, the net gain from surgical intervention for asymptomatic carotid stenosis is unclear in comparison with current optimal medical therapy.
Stroke risk, even in symptomatic cerebrovascular disease, can be substantially reduced with aggressive medical therapy. Recent guidelines have introduced alternative antiplatelet therapies and have taken into account the potential benefit of dual-antiplatelet therapy in the early phase following onset of symptoms. Furthermore, high-intensity statins are now recommended in patients with symptomatic carotid artery disease irrespective of patients’ lipid level. In a 2013 observational study, which pooled individual patient data from multiple centers internationally, Merwick and colleagues found that statin pretreatment was associated with lower 90-day stroke risk in patients with TIA and carotid stenosis, thereby highlighting the importance of acute statin treatment in preventing early strokes.
Is Carotid Artery Stenting a Viable Substitute for Carotid Endarterectomy?
In patients with high surgical risk, such as those with concomitant severe cardiovascular or pulmonary disease, previous history of neck surgery, or cervical radiation therapy, carotid artery stenting (CAS) offers a viable alternative to CEA (see Fig. 2 ). The SAPPHIRE (Stenting and Angioplasty with Protection in Patients with High Risk for Endarterectomy) trial showed that CAS was noninferior to CEA for the primary composite end point of death, stroke, and myocardial infarction within 30 days, and death and ipsilateral stroke within 1 year (16.3% vs 20.0%). Controversy remains for patients with average surgical risk despite several randomized trials that compared the 2 approaches. In a meta-analysis of individual patient data from 3 European trials on symptomatic carotid stenosis, Bonati and colleagues noted that CAS in patients 70 years or older had a higher perioperative risk of stroke or death when compared with carotid endarterectomy (8.9% vs 5.8% within 120 days). The CREST (Carotid Revascularization Endarterectomy versus Stenting Trial) is the largest trial used to compare CAS with CEA in both symptomatic and asymptomatic carotid stenosis. No significant difference was found in the estimated 4-year rates of the composite end point including stroke, myocardial infarction, and death during the periprocedural period and ipsilateral stroke within 4 years (7.2% vs 6.8%). However, during the periprocedural period stroke occurred more frequently in the CAS arm, whereas myocardial infarction occurred more frequently in the CEA arm.
Based on these data, CAS is indicated in guidelines as an alternative to CEA for patients with an average or low risk of complications associated with endovascular intervention. However, older age (≥70 years) is considered as a factor that may drive the equilibrium toward CEA. Furthermore, several lesion-specific conditions that increase the probability of embolization from CAS have been associated with increased periprocedural events, such as a tortuous aorta, angulation of carotid bifurcation, and heavily calcified carotid plaques. Identification of these factors before CAS would contribute to improved outcomes.
Current clinical challenges
Prevalence of Carotid Artery Disease
Carotid artery disease, a local manifestation of systemic atherosclerosis, is not an uncommon finding in clinical practice. Indeed, a recent study pooling individual participant data from 4 large population-based studies estimated that the prevalence of asymptomatic moderate carotid stenosis, defined as 50% or more based on duplex ultrasonography, was as high as 7.5% in the general population depending on subjects’ age and sex. Specifically, 2.3% of men and 2.0% women in their 60s had carotid stenosis on ultrasonographic examination, which increased to 7.5% and 5.0% for individuals aged 80 years or older. In subgroups with cardiovascular risk factors or those with established coronary or peripheral artery disease, the prevalence of carotid stenosis is increased by severalfold compared with the general population.
In addition, the prevalence of carotid artery disease that is significant, from a histopathologic point of view, may be underestimated. Nonstenotic or minimally stenotic carotid plaques can harbor substantial amounts of lipid and necrotic debris as a result of outward remodeling and the geometry of the carotid bulb. Furthermore, high-risk plaque features such as intraplaque hemorrhage (IPH), thin or ruptured fibrous cap, and plaque inflammation have been found in carotid plaques that are otherwise morphologically indistinct ( Fig. 1 ). In a 2008 study, 192 subjects underwent ultrasonography to quantify the degree of carotid stenosis, and MR imaging to identify the presence of complex plaques. Complex plaques were defined as having IPH or luminal surface defect on multicontrast MR images and were more frequently found in plaques with higher grades of stenosis. Of note, however, complex plaques were detected in 21.7% of arteries with only 16% to 49% luminal stenosis. Increasingly, the advent of improved techniques for vessel wall imaging demonstrates that diagnostic imaging methods that only measure stenosis underestimate plaque burden, plaque complexity, and, hence, the true prevalence of histologically significant carotid artery disease.
Clinical Outcomes with Medical Therapy Alone
Most carotid plaques have a relatively benign clinical course. However, once carotid artery disease becomes symptomatic, it often leads to disabling or devastating stroke without preceding signs. In the Asymptomatic Carotid Surgery Trial (ACST), half of the ipsilateral ischemic strokes in patients with asymptomatic carotid stenosis greater than 60% were disabling or fatal. Carotid artery disease is a major source of ischemic stroke, accounting for approximately 15% of the 795,000 incident strokes that occur annually in the United States. Less known is the role of nonstenotic but high-risk carotid plaques in cryptogenic strokes, of which a significant portion may be attributable to large-artery atherosclerosis, as discussed elsewhere in this issue.
Medical therapy plays a pivotal role in the primary and secondary prevention of ischemic strokes ascribed to carotid artery disease. The benefit of aspirin has long been recognized, and it is currently listed as a class I recommendation in guidelines for the management of asymptomatic and symptomatic carotid artery disease. Multiple clinical trials have established the efficacy of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) in reducing the incidence of major cardiovascular events and stroke, which is proportional to individuals’ baseline risk and absolute reduction in low-density lipoprotein cholesterol. Annual event rates for recurrent strokes from all sources have decreased from 8.7% in the 1960s to 4.98% in the 2000s, in part attributed to more prevalent use of statins along with improved profiles in blood pressure, smoking, and antithrombotic agents. In current guidelines, optimal medical therapy including aspirin and statin use, synergistic control of vascular risk factors, and lifestyle intervention forms the foundation of clinical management.
Carotid Endarterectomy
Excision of the culprit carotid plaque can offer long-term benefits in selected patients. To ensure net benefit on an individual basis, the evaluation of operative risk and future stroke risk must be carefully compared ( Fig. 2 ).