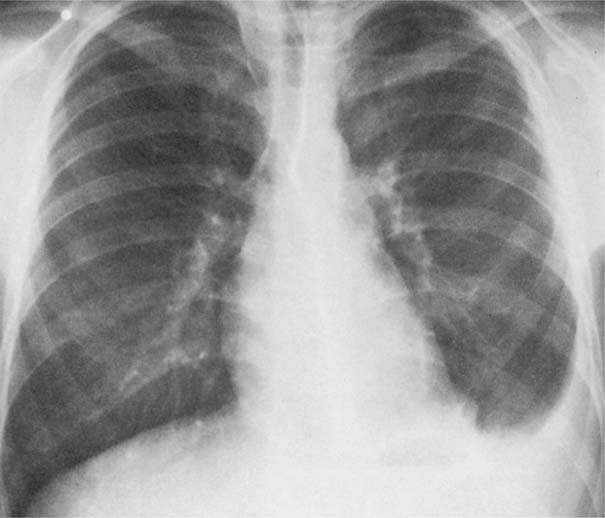
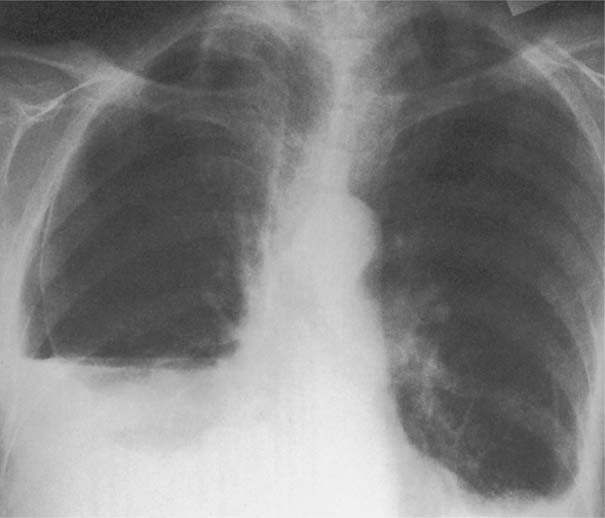
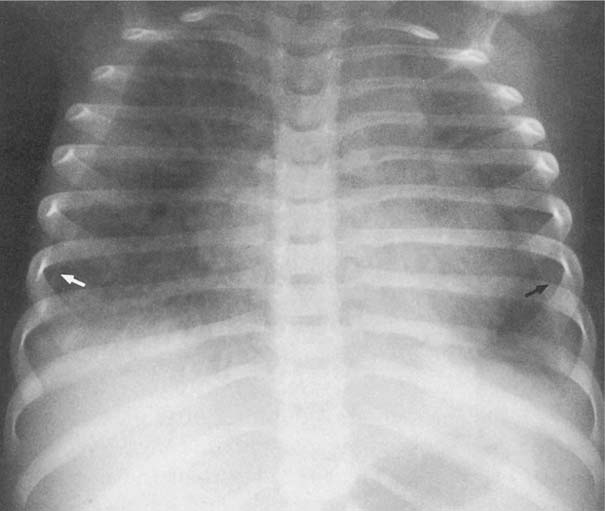
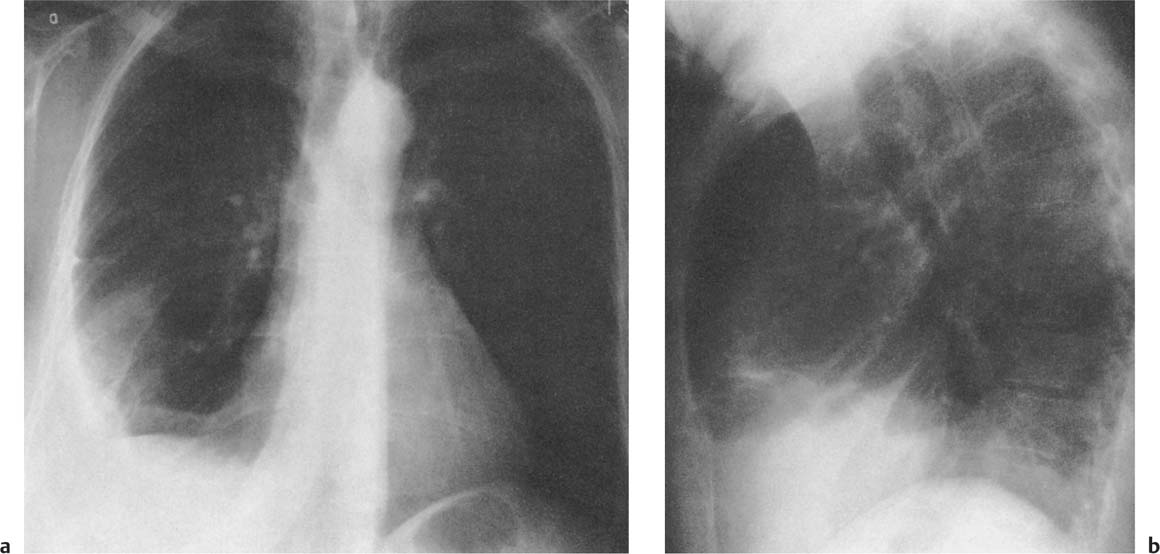
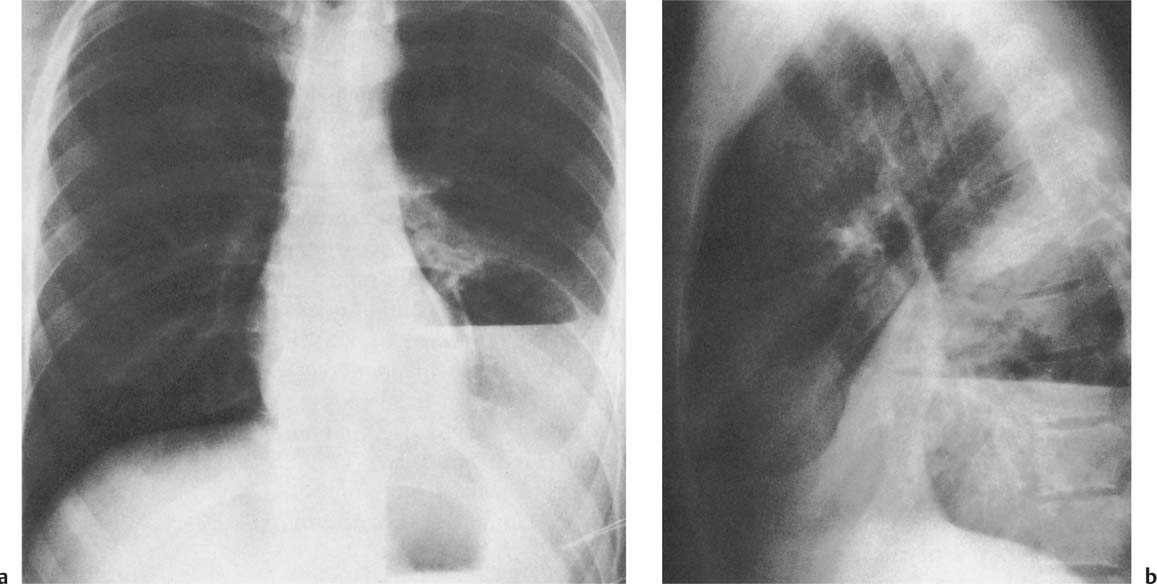
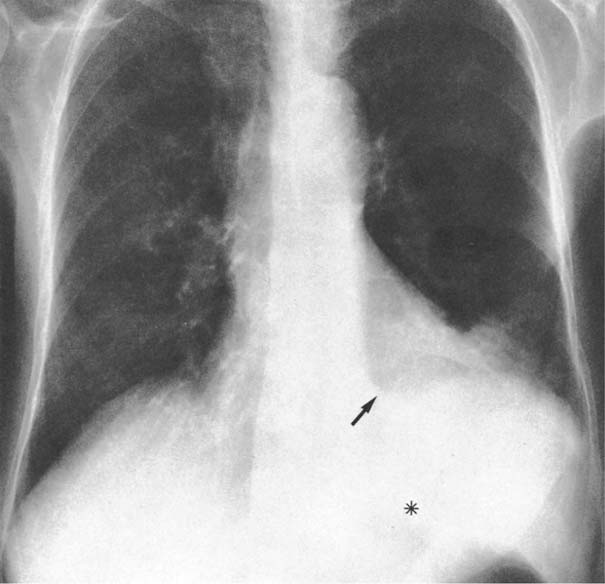
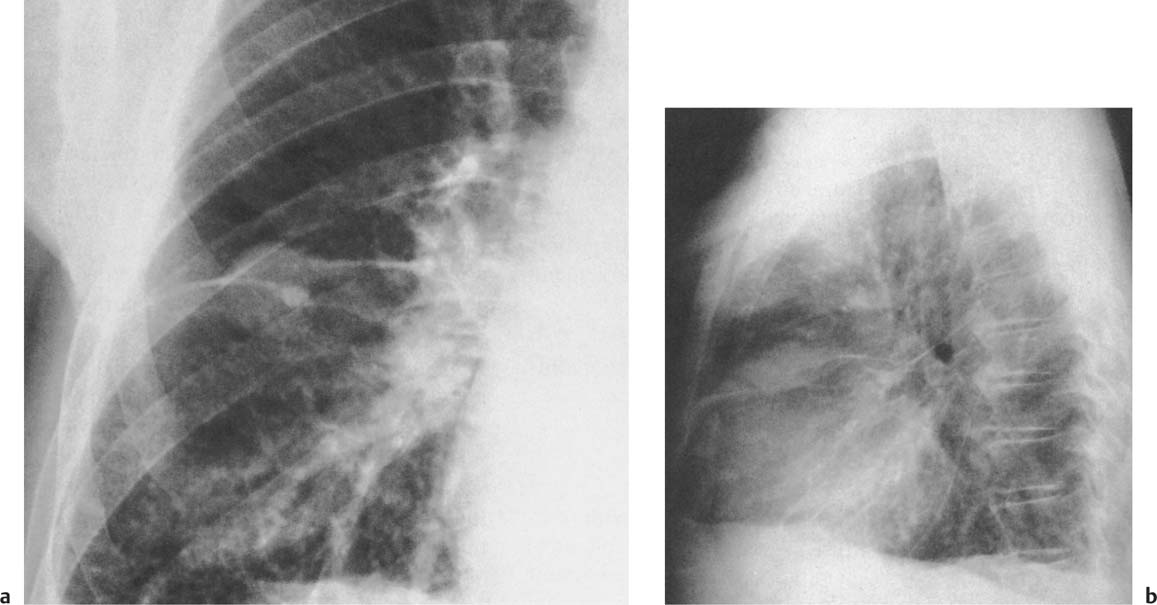
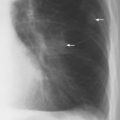
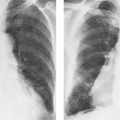
3 Pleura and Diaphragm Up to 15 ml of pleural fluid is present in normal healthy humans. This amount is not visualized in normal chest roentgenograms, but it can be demonstrated using a horizontal roentgen beam and lateral decubitus projection, which is the most sensitive plain film technique for such a purpose. As much as 250–600 ml of pleural fluid is required for roentgenographic demonstration in the erect subject. Lowering or flattening of diaphragm may be caused by inreased air pressure, emphysema of any origin and air trapping for any reason. Elevation is caused by a number of conditions which are discussed on Table 3.2. Diaphragm may show one or several humps. They may be congenital or caused by disease which usually is extrapulmonary. Gravity and elastic recoil of lung tissue cause collection of fluid between the inferior surface of the lung and the hemidiaphragm, particularly in the deepest posterior sinus. The layer of fluid that spreads upward in a mantle-like fashion around the lung becomes thinner until the parietal and visceral layers of the pleura meet again. This is influenced by capillary attraction. Since there is less elastic recoil in the mediastinal surface of the lung, less fluid accumulates along this surface than around the convexity. Thus in post-eroanterior projection, the density of the fluid will be high laterally and will curve gently downward and medially, with a smooth meniscus-shaped upper border (Fig. 3.1). The height of fluid accumulation is identical posteriorly, laterally, and anteriorly, but the thin layer of fluid viewed en face will not cast a discernible shadow. Frequently, small amounts of fluid may accumulate between the inferior surface of the lower lobe and the diaphragm without “spilling over” into the costophrenic sinuses. Such infrapulmonary fluid collections may be confirmed by using the lateral decubitus position with a horizontal beam. In this position, the fluid accumulates into the lowermost lateral pleural space. The typical radiographic findings caused by free pleural effusion are: (1) obliteration of the normally sharp costophrenic angles (first posterior, then lateral and finally anterior); (2) extension of the fluid up the chest wall resulting in a meniscus-shaped density. In the presence of pneumothorax, the fluid layer laterally is strictly horizontal in the absence of capillary attraction (Fig. 3.2); (3) thickening of the interlobar pleural septa (wet pleura), commonly present in congestive heart failure. (4) Replacement atelectasis of the ipsilateral lung, enlargement of the ipsilateral hemithorax, displacement of the mediastinum to the contralateral side, and concave depression of the ipsilateral hemidiaphragm are changes typical of massive pleural fluid accumulation. If one hemithorax is totally opacified, but the mediastinum shows no shifting and the hemidiaphragm is not markedly depressed, the findings are not caused primarily by a space-occupying process of pleural effusion but are due to primary reduction of the volume of the ipsilateral lung, e.g., pulmonary disease. The most likely cause of such a finding is an endobronchial obstruction, such as bronchogenic carcinoma. Films taken in the supine position are insensitive in detecting pleural effusion, which layers behind the lung. Increased density of the hemithorax and a layer of fluid in the surrounding pleural space may be seen (Fig. 3.3). Fig. 3.1 Left pleural effusion (tuberculous pleuritis) with characteristic meniscus shape. No other abnormality. Fig. 3.2 Bilateral, freely mobile pleural effusions with and without pneumothorax. On the left side, the pleural fluid has a meniscus shape, while on the right side it is strictly horizontal due to pneumothorax. Fig. 3.3 Bilateral pleural effusion in a newborn (due to heart failure) as seen in supine position. There is a slight increase in the density of the right hemithorax, where the amount of fluid is greater and there is more replacement collapse of the lung, The layer of fluid in the pleural space is widest near the pulmonary apices. Major fissures are demonstrated because fluid enters into the lateral aspect of the fissures (arrows). Atypical distribution of pleural fluid may indicate localized parenchymal disease as well as pleural disease. In the region of parenchymal disease, the elastic recoil is decreased and fluid is attracted to those areas of the thorax where retraction force is greatest, e.g., where lung tissue is normal. Pleural fluid may simulate atelectasis or consolidation (Figs. 3.4 and 1.5). Lateral decubitus view may help in visualizing the underlying parenchymal changes by redistributing the fluid. Infrapulmonary (subpulmonary) pleural effusion (Fig. 3.6) without blunted costophrenic angles may represent a phenomenon of altered pulmonary recoil, but it is also seen with apparently normal lung. Although the lateral decubitus view is the best way of demonstrating an infrapulmonary fluid collection, it is important to know the following signs commonly present in erect films to raise suspicion of infrapulmonary effusion: 1. Infrapulmonary fluid is more common on the right; it can be bilateral. 2. In posteroanterior projection, the peak of the pseudodiaphragmatic configuration is lateral to that of the normal hemidiaphragm. 3. On the left side, there is an increased distance between the lung base and the gastric air bubble (this also occurs with gastric tumors and interposition of the liver or spleen) (Fig. 3.6). An indentation on the gastric air bubble represents the depressed diaphragm. 4. The posterior costophrenic gutter is usually blunted, although other signs of fluid in costophrenic angles are lacking. 5. In the lateral projection, the contour of the fluid is usually flattened anterior to the major fissure. This segment descends abruptly to the anterior costophrenic angle. 6. There may be a triangular mediastinal collection of fluid seen in the anteroposterior view. Loculated or encysted pleural fluid may occur anywhere in the pleural space secondary to pleural adhesions. Samples of loculated pleural fluid are presented in Figures 3.7 and 3.8. Encapsulated fluid in the lower half of the major fissure may mimic atelectasis and consolidation of the right middle lobe. However, encapsulated fluid does not obscure the minor fissure or right heart border as do atelectasis or consolidation of the middle lobe. Furthermore, encapsulated fluid has a spindle-shaped form, whereas the shadow of the diseased middle lobe has straight or slightly concave borders. Encapsulated fluid does not move in response to postural changes. Thus, encapsulated fluid and pleural thickening may have identical appearance. Fig. 3.4a, b Right pleural effusion (metastatic breast carcinoma, post left mastectomy) may mimic consolidation or atelectasis in anteroposterior projection. The densities are created by fluid in the fissures surrounding the middle lobe. Fig. 3.5a, b Atypical accumulation of pleural effusion around a left lower lobe abscess containing an air–fluid level. Fig. 3.5c Post thoracentesis. There is inadvertent pneumothorax and pneumoperitoneum. The fluid within the abscess remains, while the pleural collection has disappeared. Fig. 3.6 Infrapulmonary pleural effusion on the left (chronic leukemia). The peak of the pseudodiaphragmatic configuration is more lateral than normal and there is increased distance between the lung base and the gastric air bubble (asterisk). A triangular rnediastinal collection of fluid is seen (arrow). Positive diagnosis is often, but not always, obtained from laboratory studies of the pleural fluid. In Table 3.1, emphasis has been put on associated radiologic findings as criteria for differential diagnosis. Pleural effusion unassociated with other roentgeno-graphic evidence of disease in the thorax is a nonspecific finding and the differential diagnosis depends on additional clinical information or roentgenographic findings elsewhere in the body. Common causes of pleural fluid with the otherwise normal-looking chest are: 1 infection of the pleura (tuberculosis, viral diseases) or of the abdomen (pancreatitis, subphrenic abscess); 2 extrathoracic carcinoma, either metastatic to the pleura or mediastinal nodes (most commonly due to breast carcinoma) or via diaphragmatic lymphatics (carcinoma of the pancreas or retroperitoneal lymphoma); 3 collagen diseases (rheumatoid arthritis, systemic lupus erythematosus); 4 cirrhosis with ascites; 5 closed chest trauma or abdominal surgery. Fig. 3.7a, b Encapsulated fluid in the minor fissure; a pseudotumor, The lobulated effusion has a typical spindle-shaped form. Severe heart failure with interstitial pulmonary edema. Fig. 3.8a, b Loculated right posterior hydropneumothorax post surgery for esophageal carcinoma. An air–fluid level is seen around the right lower lobe (arrows), secondary to the rupture of the displaced stomach which is seen as a density over the right heart border.
Roentgenologic Signs of Pleural Effusion
Disease | Radiographic Findings | Comments |
Neoplasms |
|
|
Bronchogenic carcinoma |