Abstract
Pleural and subpleural pulmonary opacities may often be distinguished by their borders, with tapered borders favoring a pleural origin while a sulcus sign or irregular borders favor a pulmonary origin. Distinction of a loculated pleural effusion from pleural masses may not be possible on the chest x-ray but should be easily distinguished on CT. Solitary peripheral masses are more likely peripheral subpleural pulmonary masses while pleural masses such as metastases and mesothelioma are most often multiple.
Keywords
empyema, mesothelioma, metastases, pleural plaques, round atelectasis, solitary fibrous tumor, splenosis
Questions
- 1.
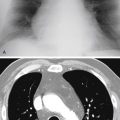
Referring to Fig. 3.1, A-C , which of the following is the most likely diagnosis?
- a.
Metastatic melanoma.
- b.
Metastatic breast carcinoma.
- c.
Invasive thymoma.
- d.
Mesothelioma.
- e.
Metastatic ovarian carcinoma.

Fig. 3.1
- a.
- 2.
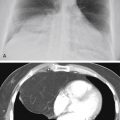
Referring to Fig. 3.2, A and B , the most likely diagnosis for this case is:
- a.
Rounded atelectasis.
- b.
Localized fibrous tumor of the pleura.
- c.
Multiple myeloma.
- d.
Infarct.
- e.
Mesothelial cyst.

Fig. 3.2
- a.
- 3.
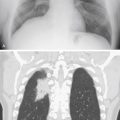
Referring to Fig. 3.3 , which of the following is the most likely diagnosis?
- a.
Mesothelioma.
- b.
Neurofibromatosis.
- c.
Localized fibrous tumor of the pleura.
- d.
Multiple myeloma.
- e.
Invasive thymoma.

Fig. 3.3
- a.
Mark the following questions True or False:
- 4.
_____ A shaggy, irregular border favors a subpleural, parenchymal lung lesion over a pleural lesion.
- 5.
_____ Mesothelioma frequently causes bone destruction.
- 6.
_____ Pleural lesions may be confused with mediastinal masses.
Discussion
Solitary Pleural Opacity
The radiologic evaluation of a solitary pleural opacity ( Chart 3.1 ) is complicated by the paucity of reliable signs for accurate localization. 519 , 588 The opacity should be in a peripheral extrapulmonary location, which may be confirmed by identifying the incomplete border sign (see Fig. 2.4 , A and B ). The peripheral position is easily recognized when the mass is against the lateral chest wall, but the correct location may be more difficult to identify when the mass is either anterior or posterior ( Fig. 3.4, A ). The lateral view (see Fig. 3.2, A ), or even a computed tomography (CT) scan 124 (see Fig. 3.2, B, and Fig. 3.4, B ), may be needed to confirm the peripheral location. A peripheral mass requires consideration of three locations: (1) chest wall, (2) pleura, and (3) subpleural area of the lung. Smooth, incomplete tapered borders with obtuse pleural angles localize a mass to either the chest wall or pleura, whereas shaggy borders and acute pleural angles confirm the diagnosis of a subpleural peripheral lung opacity ( Fig. 3.5, A-C ). One pitfall is that a peripheral lung mass, such as a metastasis, may have smooth borders. Some metastatic tumors and even lymphoma can also disseminate to both the lung and pleura. The foregoing signs for localizing peripheral masses are sometimes indeterminate on the chest radiograph, but they are also applicable in CT scan interpretation. In fact, CT is often required for the precise localization of abnormalities seen on the chest radiograph.
- I.
Loculated pleural effusion
- II.
Metastasis 131
- III.
Mesothelioma 47 (rare)
- IV.
Lipoma 153 , 160 , 183 , 195 , 466
- V.
- VI.
Hematoma
- VII.
Mesothelial cyst
- VIII.
Neural tumor (schwannoma, neurofibroma) 459
- IX.


Some pleural tumors lack the broad-based pleural signs described previously because they have a small area of attachment to either pleural surface and appear more round. The case shown in Fig. 3.2, A and B , was described at surgery as a pedunculated pleural mass. Berne and Heitzman 43 have reported that pedunculated pleural tumors may be fluoroscopically observed to change shape or move with respiration. This motion may also be recorded on inspiration and expiration views. Documentation of free movement in the pleural space distinguishes the chest wall from pleural masses.
Medial pleural opacities are probably the most confusing. A mass in this position is often more suggestive of a mediastinal mass. Because pleural masses and mediastinal masses are seen as a result of their interface with the lung, both have a sharp incomplete border that is frequently tapered; therefore, diagnosis of a medially located mesothelioma can be made only by biopsy. Similarly, mesothelioma arising from an interlobar fissure is difficult to identify correctly as a pleural mass. This is best accomplished by identification of the fissures on the lateral view or with a CT scan.
Pleural tumors, cysts, and loculated effusions all appear homogeneous on chest radiographs, but should be distinguished with ultrasound, CT, or magnetic resonance imaging (MRI) scanning. Pleural tumors may be regarded as solid, but they are not always entirely homogeneous. The large mass shown in Fig. 3.2, A and B , is shown by CT to be heterogeneous, with soft-tissue opacity, a calcification, and areas of low attenuation caused by necrosis. It does not have uniform low attenuation, which is expected with a mesothelial cyst.
Localized fibrous tumor of the pleura (see Fig. 3.2, A and B; answer to question 2 is b ) probably arises from submesothelial mesenchymal cells rather than mesothelial cells and is usually benign, although 37% of such tumors have been reported to be malignant. 124 , 483 Localized fibrous tumor of the pleura should present as a well-circumscribed peripheral mass and should not invade the chest wall or lung. The chest radiographs in this case are not adequate for exclusion of a chest wall mass, but the CT scan shows the mass to be separate from the chest wall and thus makes multiple myeloma an unlikely choice. The CT appearance of this heterogeneous mass further excludes mesothelial cyst. Both pulmonary infarcts and rounded atelectasis are pulmonary processes that typically have a subpleural location. They usually have poorly defined borders, and the CT scan should confirm their pulmonary origin. 375
A solitary pleural metastasis is impossible to differentiate on the basis of its radiologic features from the mass seen in this case. The similarity of a solitary metastasis is illustrated in Fig. 3.4, A and B . Metastatic disease is the most common cause of a pleural mass, with lung and breast cancer accounting for 60% of cases.
Multiple Pleural Opacities
Multiple pleural opacities ( Chart 3.2 ) are usually the result of loculated effusion, pleural masses, or a combination of the two. The radiologic appearance is that of multiple, separate, sharply circumscribed, smooth, tapered opacities ( Fig. 3.6 ) or of diffuse pleural thickening with lobulated inner borders. Loculated pleural effusion is probably the most common cause of this appearance. The causes of loculated effusion include empyema ( Fig. 3.7, A ), hemorrhage, and neoplasms. Lateral decubitus views are of little value in recognizing the condition because some free fluid may coexist with either loculated collections of fluid or solid masses. Sequential radiographs showing a change over a short period should suggest the presence of loculated fluid collections ( Fig. 3.8, A and B ). Ultrasound and CT scans (see Fig. 3.7, B ) may be useful for confirming the presence of loculated fluid collections and for thoracentesis or drainage procedures. A history of recent pneumonia is evidence that favors a loculated empyema. 220 , 519