Abstract
Pleural thickening has a variety of causes and often must be distinguished from pleural masses, while pleural calcifications are frequently the result of chronic infections, including bacterial or tuberculous empyema. The pleural plaques of asbestos may be localized soft tissue but frequently calcify with a characteristic radiologic appearance on both chest x-ray and CT. Involvement of parietal versus visceral pleura is pathologically significant in the separation of asbestos-related pleural thickening from the inflammatory and neoplastic causes of pleural disease, but this distinction is limited to those patient with a pneumothorax that separates the two layers of pleura.
Keywords
asbestos-related pleural plaque, empyema, hemothorax, lung cancer, mesothelioma, metastases, rheumatoid pleural disease, splenosis, talcosis, tuberculosis
Questions
- 1.
What is the most likely diagnosis for the case illustrated in Fig. 5.1 ?
- a.
Mesothelioma.
- b.
Metastases.
- c.
Empyema.
- d.
Lung cancer.
- e.
Lymphoma.
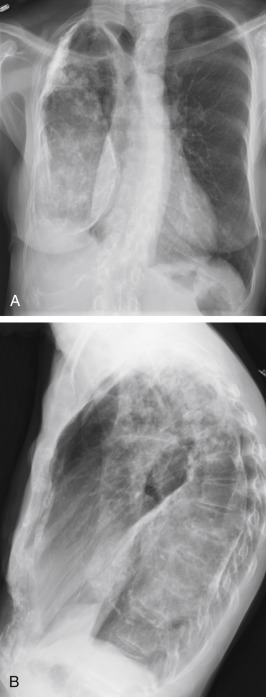
Fig. 5.1
- a.
- 2.
The large calcification in Fig. 5.2 is most probably caused by:
- a.
Tuberculosis.
- b.
Asbestosis.
- c.
Mesothelioma.
- d.
Empyema.
- e.
Talcosis.
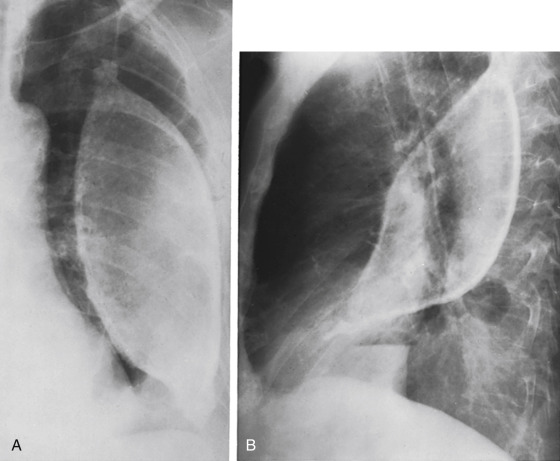
Fig. 5.2
- a.
- 3.
Which one of the following interstitial lung diseases is most likely to have associated plaques of pleural thickening?
- a.
Rheumatoid lung.
- b.
Scleroderma lung.
- c.
Usual interstitial pneumonitis.
- d.
Desquamative interstitial pneumonitis.
- e.
Asbestosis.
- a.
Discussion
Pleural thickening must be distinguished from pleural fluid ( Chart 5.1 ). Like pleural effusion, pleural thickening is usually appreciated as a thick white line between the lucent lungs and ribs. Lateral decubitus views are frequently necessary for distinguishing free pleural effusion from pleural thickening, but loculated effusions are not as easily distinguished from pleural thickening. This may sometimes be accomplished by comparison with prior examinations. When the pleural thickening is of recent onset (days to weeks), pleural effusion is the most likely cause of the opacity, whereas if the process has been stable for months to years, it is most probably true pleural thickening. As with pleural masses, ultrasound or computed tomography (CT) may be essential for distinguishing loculated fluid collections from pleural thickening or nodules.
- I.
Infection
- II.
Neoplasm
- III.
Collagen vascular (rheumatoid arthritis 369 )
- IV.
Trauma (healed hemothorax)
- V.
Inhalational diseases
- VI.
Other
- A.
Organization of serous pleural effusion
- B.
Sarcoidosis 635
- C.
Splenosis 270
- D.
Fat 160
- E.
Mimics (extrathoracic musculature) 88
- A.
Organizing Effusion
Organization of an infected pleural effusion (empyema) is one of the most common causes of pleural thickening. The detection of a small amount of associated pleural fluid may seem unimportant but is vital for diagnostic thoracentesis. 478 The fluid may appear to be nondiagnostic, but it provides material for culture and cytologic studies. An organizing fibrothorax is definitely less diagnostic because it usually consists of chronic inflammatory cells and fibrosis. It may be the end result of a variety of bacterial, fungal, and tuberculous pulmonary infections. In such cases, the radiologic finding of pleural thickening is nonspecific, and the radiologic diagnosis usually depends on associated pulmonary findings. Apical pulmonary cavities with associated pleural thickening are characteristic of prior granulomatous infection, such as tuberculosis or histoplasmosis. 388 A strongly reactive skin test may confirm the diagnosis. Additional complications should be suspected in patients with old cystic lesions or cavities who develop a new pleural opacity in the area of the old abnormalities. A new area of pleural thickening in the same vicinity is suggestive of new complications, which include reactivation of tuberculosis, scar cancer, or a new infection, such as aspergilloma, which develops in old cavities and may cause pleural thickening. 340 As with other causes of inflammatory pleural thickening, the histologic appearance of the pleural disease secondary to aspergilloma is nonspecific. The fungus is not usually identifiable in the pleural reaction.
The less specific appearance of extensive pleural thickening over the bases, with associated parenchymal scars, can best be diagnosed as chronic empyema when a definite history of previous pneumonia is obtained. Some noninfectious causes of pleural effusion, such as rheumatoid disease, occasionally fail to resolve, with the final result of a thick pleural reaction ( Fig 5.3 ). 369 A history of known rheumatoid arthritis may suggest this diagnosis. In addition, positive results of serologic studies for rheumatoid factor may also suggest the diagnosis, particularly if there is a history of thoracic disease prior to the onset of joint disease.