, Joungho Han2, Man Pyo Chung3 and Yeon Joo Jeong4
(1)
Department of Radiology Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(2)
Department of Pathology Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(3)
Department of Medicine Division of Pulmonary and Critical Care Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(4)
Department of Radiology, Pusan National University Hospital, Busan, Korea, Republic of (South Korea)
Abstract
Pulmonary infection can also be classified into several radiologic and pathologic patterns according to its morphologic features. The three most common patterns are lobar pneumonia, bronchopneumonia, and interstitial pneumonia. Less common forms of infection include cellular bronchiolitis, septic embolism, miliary infection, and lung abscess. Because less common forms of infectious condition have been dealt in previous other chapters, the three most common patterns only are described in this chapter.
Pulmonary infection can also be classified into several radiologic and pathologic patterns according to its morphologic features. The three most common patterns are lobar pneumonia, bronchopneumonia, and interstitial pneumonia. Less common forms of infection include cellular bronchiolitis, septic embolism, miliary infection, and lung abscess. Because less common forms of infectious condition have been dealt in previous other chapters, the three most common patterns only are described in this chapter.
Lobar Pneumonia
Lobar pneumonia is characterized histopathologically by filling of alveolar airspaces by an exudate of edema fluid and neutrophils. This filling is usually uniform within the affected lung and typically extends across pulmonary segments. The consolidation usually begins in the periphery of the lung adjacent to the visceral pleura and spreads via inter-alveolar pores and small airways centripetally, sometimes to involve the entire lobe. Bronchi that remain filled with gas and become surrounded by the expanding inflammatory exudate are often seen as air bronchograms on CT scans. The most common causative organisms are Streptococcus pneumoniae, Klebsiella pneumoniae (Fig. 26.1), and Legionella pneumophila.
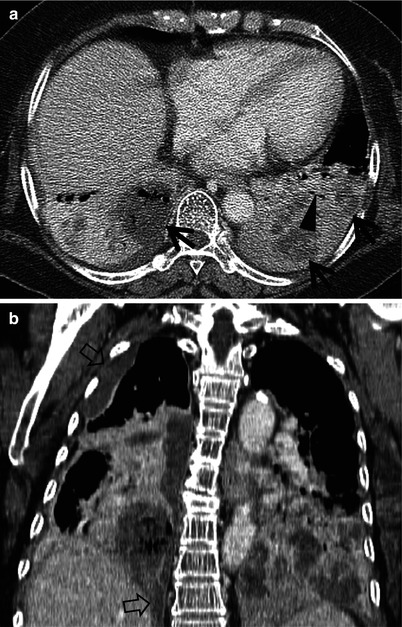
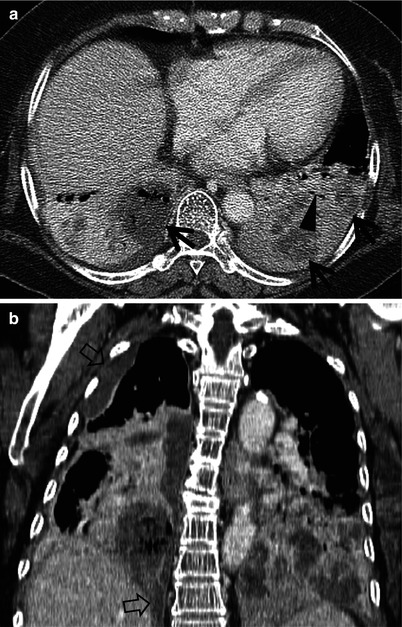
Fig. 26.1
Klebsiellapneumonia in a 62-year-old woman. (a) Mediastinal window of enhanced CT scan (2.5-mm section thickness) obtained at level of liver dome shows dense lobar consolidation in both lower lobes containing multifocal areas of necrotic low-attenuation areas (arrows). Also note CT air-bronchogram signs (arrowhead) within consolidative lesions. (b) Coronal reformatted image demonstrates necrotic lobar consolidation involving both lower lobes. Also note right pleural effusion (open arrows)
On CT scans, homogeneous airspace consolidation involving adjacent segments of a lobe is the predominant finding. On HRCT, areas of ground-glass opacities (GGO) denoting incomplete filling of alveoli can be seen adjacent to the airspace consolidation [1]. The consolidation typically extends across lobular and segmental boundaries.
Segmental or lobar form of tuberculous pneumonia may occur in adults; in AIDS or non-AIDS immunocompromised patients including pregnant women, elderly, diabetics, alcoholics, and transplanted patients. Multiple small cavities may be shown within the consolidative lesion [2, 3] (Figs. 26.2 and 26.3).
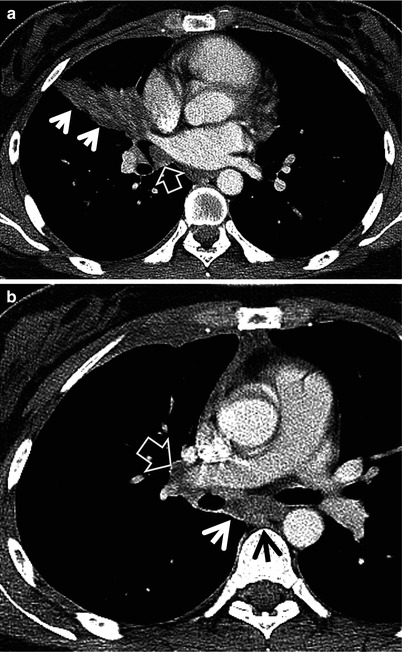
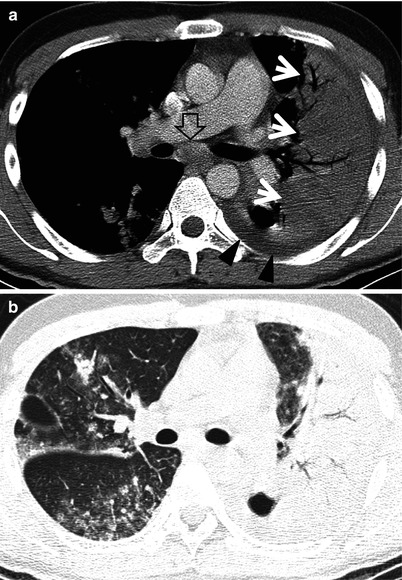
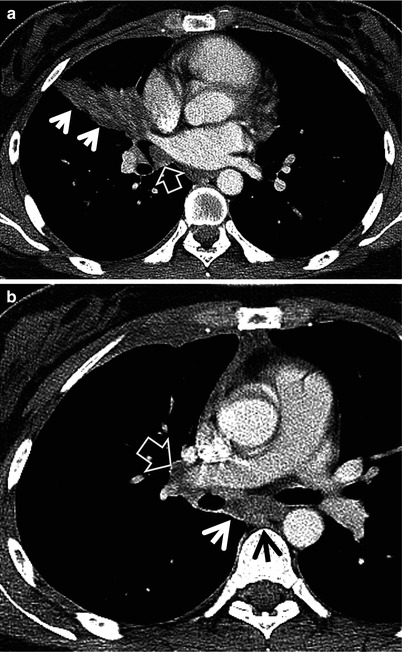
Fig. 26.2
Tuberculous pneumonia manifesting as segmental consolidation in a 26-year-old woman. (a) Mediastinal window of enhanced CT scans (5.0-mm section thickness) obtained at level of basal trunk shows segmental consolidation (arrows) in right middle lobe. Also note enlarged right hilar lymph node (open arrow). (b) CT scan obtained at level of distal left main bronchus demonstrates enlarged and necrotic subcarinal lymph node (arrows) and right hilar node (open arrow)
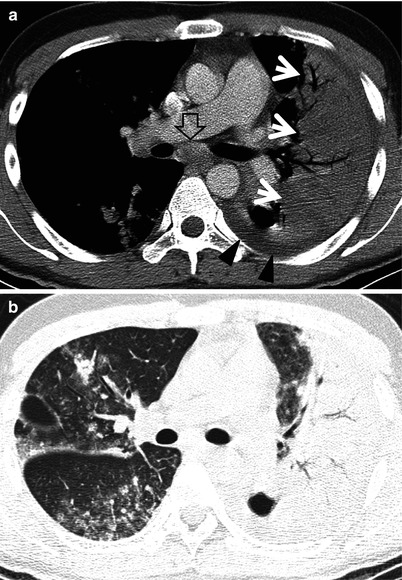
Fig. 26.3
Lobar consolidation as a manifestation of pulmonary tuberculosis in a 24-year-old man. (a) Mediastinal window of enhanced CT scans (5.0-mm section thickness) obtained at level of main bronchi shows lobar consolidation (arrows) in left upper lobe. Some parenchymal lesions are also seen in right lung. Note enlarged subcarinal lymph node (open arrow) and left pleural effusion (arrowheads). (b) Lung window image obtained at the same level to a demonstrates adds findings of tree-in-bud signs and small nodules in contralateral right lung suggestive of bronchogenic spread of tuberculous pneumonia
Bronchopneumonia
Bronchopneumonia is characterized pathologically by patchy, predominantly peribronchiolar inflammation. The reason why this localization is different from lobar pneumonia is unclear but may be related to relatively less abundant edema formation (associated with more difficult spread of infection within the lung) and more virulent organisms (resulting in greater tissue destruction) in bronchopneumonia. Although initially patchy, progression of disease may result in lobular and segmental consolidation (Fig. 26.4). The main causative organisms are Staphylococcus aureus, Haemophilus influenzae, Pseudomonas aeruginosa, and anaerobic bacteria.
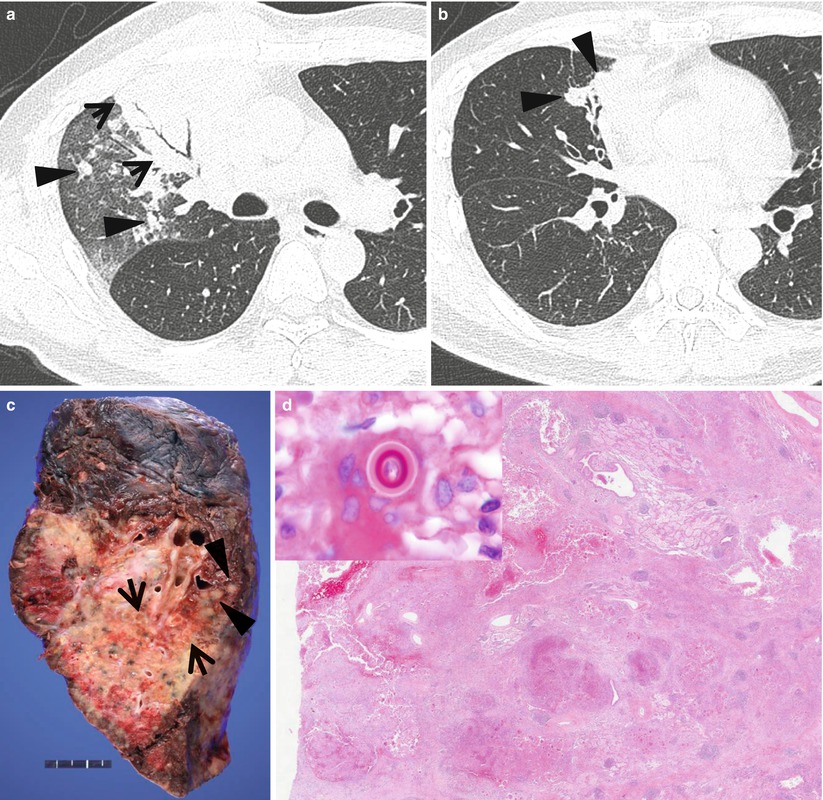
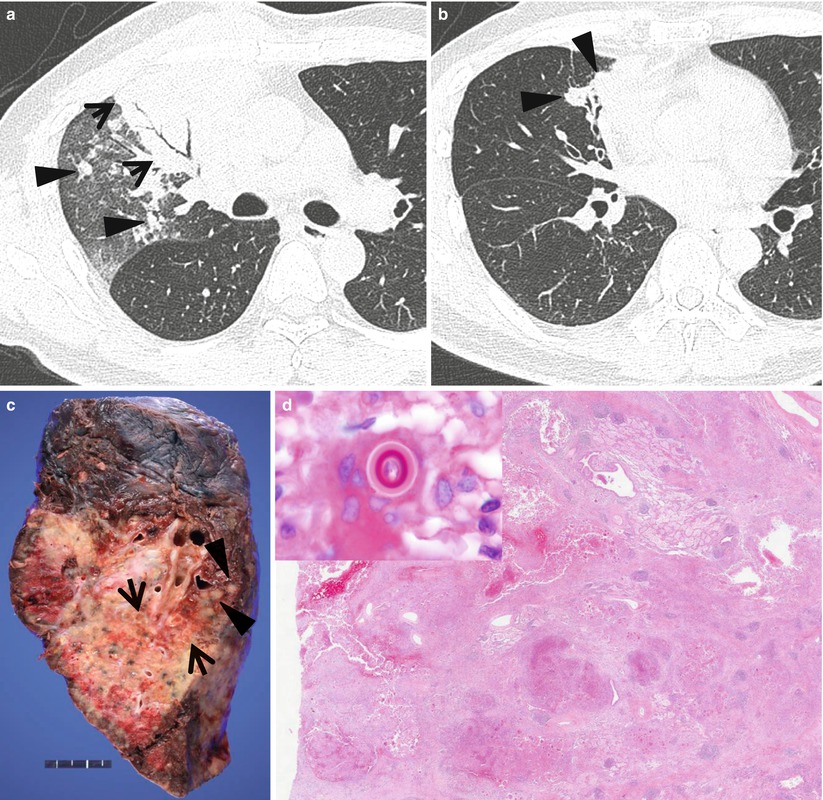
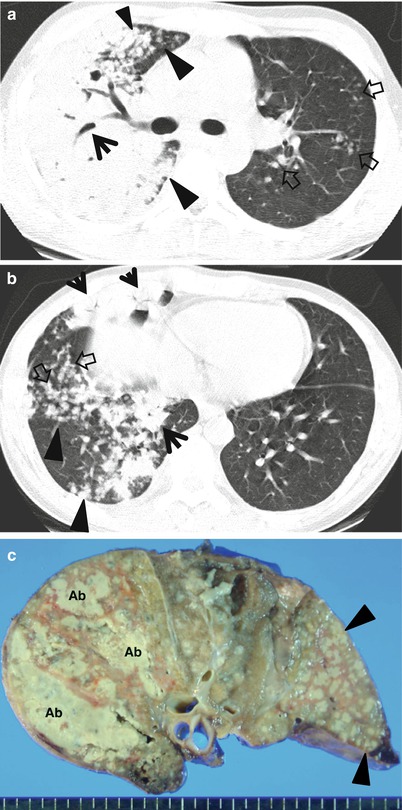
Fig. 26.4
Pulmonary blastomycosis manifesting as morphologic bronchopneumonia in a 45-year-old man. (a) Lung window image of thin-section (1.5-mm section thickness) scan obtained at level of main bronchi shows combination of subsegmental consolidation (arrows), acinus-sized small nodules (arrowheads), smaller nodules, and ground-glass opacity in right upper lobe. (b) CT scan obtained at level of basal trunk demonstrates nodular clustering (arrowheads) in right middle lobe. (c) Gross pathologic specimen obtained with right upper lobectomy depicts mainly consolidative lesion, but also small nodular lesions (arrowheads). Lesion has multifocal areas of small abscess (arrows). (d) Low-magnification (×4) photomicrograph discloses suppurative granulomatous inflammation. Inset: double-walled yeast in cytoplasm of multinucleated giant cell consistent with blastomycosis
Characteristic findings on HRCT include centrilobular small nodules and branching linear structures, airspace nodules, and multifocal lobular consolidation or GGO [1] (Fig. 26.5). The small nodules and branching linear opacities result in an appearance resembling a tree-in-bud and are related to the presence of the inflammatory exudate in the lumen and walls of membranous and respiratory bronchioles and the lung parenchyma immediately adjacent to them (Fig. 26.6). This appearance is similar to cellular bronchiolitis caused by viruses, Mycoplasma pneumoniae and Chlamydia [1, 4]. Unlike the latter (atypical pneumonias), however, the tree-in-bud pattern in bacterial bronchopneumonia usually comprises only a small proportion of the HRCT abnormalities. In addition, thickening of bronchovascular bundles is more frequently observed in atypical pneumonia, in which individual opacity tends to be distributed at the inner zone in addition to the middle and outer zones and be recognized smaller than those of bacterial pneumonias [1] (Fig. 26.5).
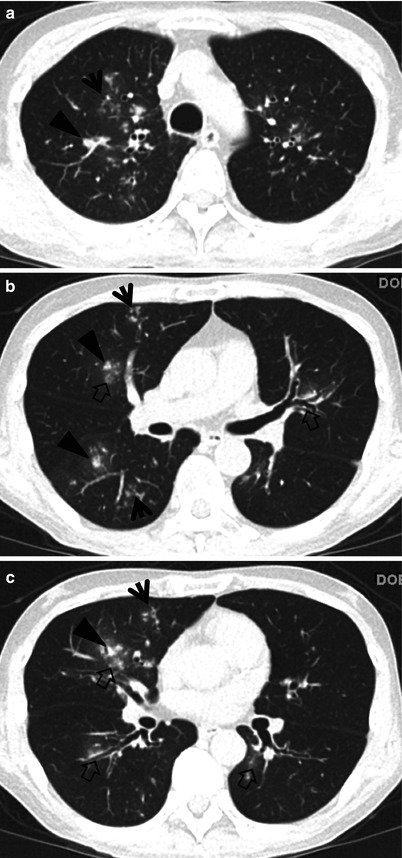
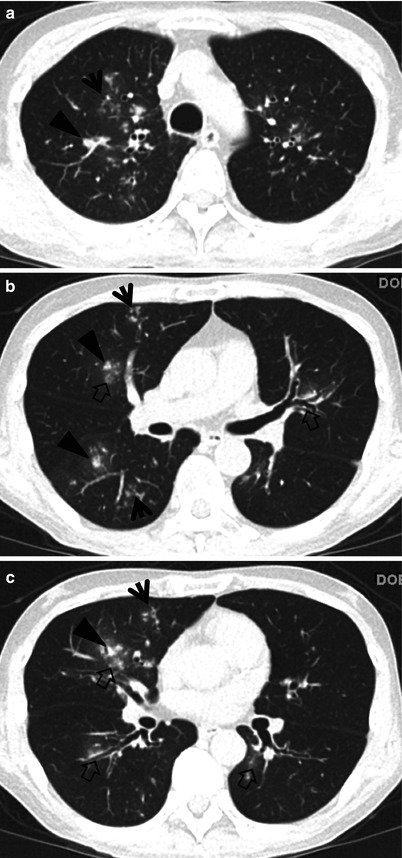
Fig. 26.5
Mycoplasma pneumoniae pneumonia in a 29-year-old man who received hematopoietic stem cell transplantation owing to acute myeloid leukemia. (a–c) CT scans (2.5-mm section thickness) obtained at levels of aortic arch (a), bronchus intermedius (b), and basal trunks (c), respectively, show lung abnormalities comprising tree-in-bud signs (arrows), small nodules (arrowheads) and ground-glass opacity lesions (open arrows) in both lungs. Please note involvement of both central and peripheral portions of lungs