Polymyositis-Dermatomyositis
Aqeel A. Chowdhry, MD
Tan-Lucien H. Mohammed, MD, FCCP
Key Facts
Terminology
Polymyositis: Autoimmune inflammatory myopathy (limb girdle & anterior neck muscles)
Dermatomyositis: Polymyositis + skin rash
Imaging Findings
Nonspecific, multiple patterns based on prevailing histology: NSIP, UIP, COP, DAD
Aspiration common and may alone result in pulmonary disease or be superimposed on other patterns
Hypoventilation also common and may result in atelectasis (discoid or long lines)
Distribution similar irrespective of pattern; primarily involves basilar lung
Dystrophic muscle calcification in polymyositis
Skin or subcutaneous calcifications in dermatomyositis
Whole-body turbo STIR helpful in demonstrating soft tissue inflammatory burden
Top Differential Diagnoses
Nonspecific Interstitial Pneumonitis
Cryptogenic Organizing Pneumonia
Idiopathic Pulmonary Fibrosis
Scleroderma
Clinical Issues
No established association between interstitial lung disease and extent of muscle or skin findings
Polymyositis: Weakness is painless in 66%
Dermatomyositis: Violaceous heliotrope rash over anterior edge of upper eyelids
TERMINOLOGY
Abbreviations and Synonyms
Polymyositis-dermatomyositis (PM-DM), dermatomyositis-polymyositis (DM-PM), dermato-polymyositis (DPM)
Nonspecific interstitial pneumonia (NSIP), cryptogenic organizing pneumonia (COP), usual interstitial pneumonia (UIP), diffuse alveolar damage (DAD)
Definitions
Polymyositis: Autoimmune inflammatory myopathy (limb girdle & anterior neck muscles)
Dermatomyositis: Polymyositis + skin rash
IMAGING FINDINGS
General Features
Best diagnostic clue
Lung disease in patient with muscle weakness
Hint: Elevated diaphragms and subsegmental atelectasis
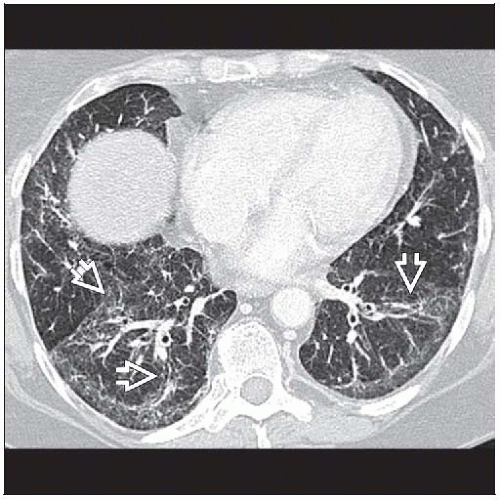
CT Findings
Nonspecific, multiple patterns based on prevailing histology: NSIP, UIP, COP, DAD
Aspiration common and may alone result in pulmonary disease or be superimposed on other patterns
Hypoventilation also common and may result in atelectasis (discoid or long lines)
Distribution similar irrespective of pattern; primarily involves basilar lung
NSIP
Ground-glass opacities > reticular opacities in bronchovascular distribution
Traction bronchiectasis out of proportion to reticular opacities
UIP
Reticular opacities and honeycombing in subpleural distribution
Traction bronchiectasis
COP
Subpleural focal areas of consolidation
Reverse halo sign
DAD
Acute diffuse ground-glass opacities often with traction bronchiectasis
Treatment
Ground-glass opacities, consolidation may resolve
Extrathoracic manifestations
Skin or subcutaneous calcifications in dermatomyositis
Dystrophic muscle calcification in polymyositis, uncommon
Other
High incidence of malignancy, particularly bronchogenic carcinoma
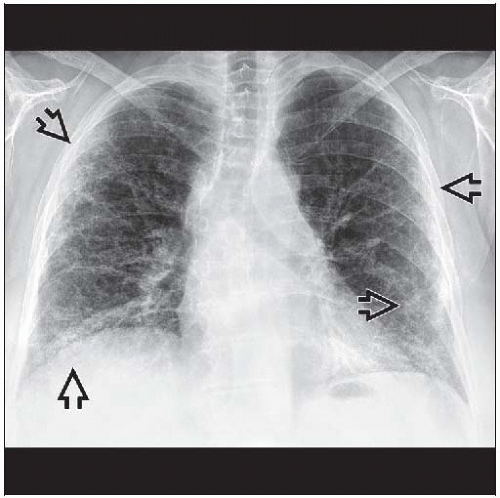
Radiographic Findings
10% have normal chest radiographs
Lung volumes reduced
Elevated hemidiaphragms due to respiratory muscle weakness, atelectasis
Lungs
Nonspecific symmetric, basal reticular pattern of parenchymal involvement, may progress to honeycombing (less often)
Aspiration
Variable appearance, aspiration segments, waxing and waning opacities eventually resulting in fibrosis
Soft tissue calcifications
Often over bony prominences
More common in younger patients
Fluoroscopic Findings
Esophagram
Upper esophagus predominantly involved may result in reflux or aspiration
Swallowing studies useful for diet
Obstruction due to stricture or scarring, late
MR Findings
Whole body turbo STIR helpful in demonstrating soft tissue inflammatory burden
Musculature
Signal intensity abnormalities due to inflammation, edema, scarring
Symmetric involvement
Proximal lower limb girdle, early
Progression to proximal upper limb girdle, neck flexors, pharyngeal muscles
Facial muscles typically spared
Images may be used to guide muscle biopsy
Imaging Recommendations
Best imaging tool
CT: Affects patient prognosis by demonstrating extent of pulmonary involvement, chronicity of disease process, and response to treatment
MR imaging useful to demonstrate areas of muscular involvement
DIFFERENTIAL DIAGNOSIS
Nonspecific Interstitial Pneumonitis
NSIP pattern common in PM-DM
No muscle involvement or skin rash
Cryptogenic Organizing Pneumonia
COP pattern common in PM-DM
No muscle involvement or skin rash
Idiopathic Pulmonary Fibrosis
UIP pattern, seen in PM-DM
Older age group, no muscle involvement or skin rash
Scleroderma
NSIP pattern common
No muscle involvement or skin rash
Esophageal dilatation common, less common in PM-DM
Drug Toxicity
Review drug history
Commonly chemotherapy drugs (bleomycin, cyclophosphamide, nitrosoureas, etc.)
Can result in any pattern seen in PM-DM
PATHOLOGY
General Features
General path comments
Thoracic involvement
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree