Fig. 13.1
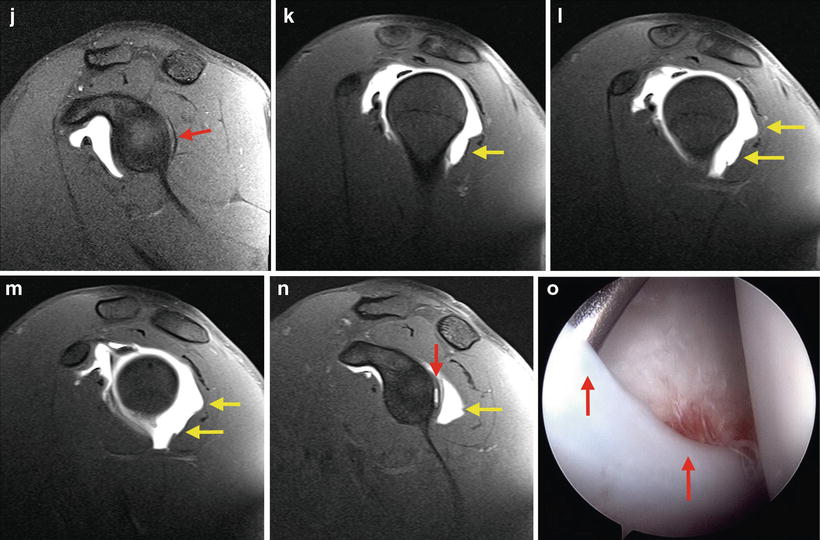
(a–d) Right shoulder T1-weighted images showing a moderate-sized tear of the posterior labrum (red arrow) without changes on the posterior capsule. These findings are consistent with a Type I posteroinferior labral tear. (e) ABER position sequence showing the posterior labrum detachment. (f–i, f–n) Axial and sagittal T1-weighted images of a left shoulder showing a posterior labral tear (red arrow) accompanied with a patulous posterior capsule (yellow arrow), without an obvious capsule tear. (j, n) Medial sagittal images of the right and left shoulders, respectively, showing the extension of the posterior labral detachment and the intact osseous glenoid rim (red arrow), with the associated more patulous posterior capsule on the left side (yellow arrow). (o, p) Detached and frayed posterior labrum on a right shoulder (red arrows). (q, r) Right shoulder. Debrided posterior labrum and posterior capsule secured with anchors (green arrows). Shifting the capsule superiorly and medially on the glenoid can be noted. Suture of the defect of the posterior cannula with PDS (blue arrow). (s–u) Left shoulder. Detached and frayed labrum (red arrow) and patulous posterior capsule with a posterior capsule tear (yellow arrows) with muscle evident through the tear. (v) Repaired posterior capsule tear with PDS sutures placed side to side (blue arrows). (w) Repaired posterior labral tear on a left shoulder (green arrow). PDS sutures of the side-to-side repair of the posterior capsule tear are visible (blue arrows)
The ABER position sequence also shows the posterior labrum detachment (Fig. 13.1e).
The same axial images on the left shoulder (Fig. 13.1f–i) show a similar posterior labral tear, this time accompanied with a more patulous posterior capsule, without an obvious capsule tear. This redundancy of the posterior capsule can also be observed on sagittal images (Fig. 13.1f–m), and the extension of the posterior labral detachment can be evaluated in a more medial sagittal image (Fig. 13.1n) showing the glenoid rim without bone loss.
Because of his worsening symptoms over the last year, a concordant physical exam, and a bilateral MRI with evidence of a posterior labrum tear and instability, he was indicated for arthroscopy with posterior labrum tear repair and capsulorrhaphy at the end of the season.
Arthroscopy
The operations were staged 6 weeks apart, starting with the right shoulder.
The procedure was performed in beach chair position under combined anesthesia. The right shoulder was examined under anesthesia prior to prepping and draping. It was stable anteriorly and inferiorly, but grade III posterior instability was found on jerk testing.
A posterior arthroscopy portal was established slightly lateral to the standard position, adjacent to the humeral head in anticipation of posterior repair. Anterior and high lateral rotator interval portals were created under needle localization.
Diagnostic arthroscopy revealed an intact anterior, superior, and inferior labrum to 6 o’clock. His posterior labrum was detached and frayed (Fig. 13.1o, p), and he had a capacious posterior capsule.
The posterior labrum was debrided to stable tissue and was found to be detached from approximately the 6:30 position to the 11 o’clock position. The posterior glenoid was debrided with a shaver down to bleeding bone. A total of five single loaded 3.0 mm absorbable anchors were placed posteriorly, using a suture lasso to shuttle sutures throughout the posterior capsule and then around the detached labrum using a two-bite technique, shifting the capsule superiorly and medially on the glenoid (Fig. 13.1q, r).
The posterior cannula was removed, and the resulting capsule defect was closed with a single #0 PDS suture.
The same setting was used for performing the surgery on his left shoulder 6 weeks later.
During examination under anesthesia, his left shoulder was stable anteriorly and inferiorly and had a grade II posterior clunk.
The posterior labrum was detached and frayed, and the posterior capsule was patulous with a posterior capsule tear (Fig. 13.1s–u). This was an oblique capsule split that went toward the humeral anatomic neck with cuff muscle evident through the tear posterior inferiorly.
The posterior capsule tear was repaired with a total of 3 #0 PDS sutures placed side to side with the joint using a suture lasso across the tear (Fig. 13.1v).
The posterior labrum tear was localized between 2 and 6 o’clock, and a total of four anchors were placed, repairing the posterior labrum anatomically into its appropriate position with generous bites of capsule also taken (Fig. 13.1w). The posterior cannula was withdrawn, and a final PDS suture was placed across the capsular defect from where the cannula was inserted.
Discussion
This case demonstrates several things common with posterior shoulder instability. Posterior shoulder instability is often seen in football [26] due to the repetitive blocking and engagement of other players with the arms outstretched in flexion. This places a lot of repetitive load on the posterior joint and can result in damage. Posterior capsule tears and reverse humeral avulsion of the glenoid ligaments (rHAGL) lesions can present in addition to posterior labrum tears or in isolation. In an acute setting, rHAGL and posterior capsule tears result in intra-articular contrast leaking into the posterior cuff musculature on the axial views or seen tracking down along the proximal humerus on the sagittal oblique cuts. These lesions can be a challenge to see on the MRI, in a chronic setting. Once scarring has occurred, imaging findings are limited, making the interpretation of the MRI more challenging. The torn stump cannot be distinguished from remodeled scar, and there is no edema or hemorrhage. A redundancy of the posterior capsule can be present (Fig. 13.1f–i), and a pseudo-pouch may form distally along the humeral neck (Fig. 13.1f–m). In addition, close inspection of the posterior and inferior capsule should be done at the time of arthroscopy to look for the lesions since they can often be missed on imaging.
There are several technical tips for repairing the posterior labrum and tears of the posterior capsule. First, the senior author prefers to use a posterior portal that is approximately 2 cm more lateral than a standard portal, which brings the cannula just along the posterior humeral head. This provides a much better angle for placing anchors in the posterior glenoid. If a standard posterior portal is used, then an additional lateralized posterior portal or percutaneous suture anchor portal will be needed to place anchors. It is recommended to repair the labrum from inferior to superior while visualizing from a superior rotator interval portal. Posterior capsule tears and rHAGL lesions can be repaired arthroscopically as well. Pearls for these repairs include using a suture passer and/or bird-beak penetrator to shuttle sutures across the capsule tears side to side. Often an additional anchor in the anatomic neck of the humerus will be needed for rHAGL lesions to restore the capsule attachment to the humerus. These sutures can be placed from the posterior portal or using a suture passer from an anterior portal, depending on the location. Sutures should be placed from inferior to superior. Suture knots may be tied on the internal or external surface of the capsule depending on how the sutures are passed and shuttled. A 70° arthroscope may be helpful to visualize rHAGL lesions or very low posterior capsule tears. Lastly, the authors prefer to always close the defect of the posterior created by the posterior cannula for cases of posterior shoulder instability. This defect often becomes large due to the thin nature of the posterior capsule and the frequent manipulation and stress on the posterior cannula. This capsule cannula defect is done at the very end of the procedure by withdrawing the cannula just outside the capsule and shuttling an absorbable (0-PDS) suture or two across the defect.
Case 2: Reverse Bony Bankart
History/Exam
A 19-year-old member of a college football team presented to the clinic complaining of left shoulder difficulties the entire prior season. He had an injury end of the prior season which had worsened, with several injuries during the recent season despite use of a shoulder stabilizing brace. He noted no pain with regular daily activities but occasionally crepitus and popping sensations.
On physical examination, the left shoulder demonstrated full range of motion and excellent strength. He had some pain on posterior loading but presents with a no subluxation on jerk test. He had pain with O’Brien testing and has no anterior apprehension.
Imaging
Plain X-rays show a reverse bony Bankart lesion (Fig. 13.2a, b) of considerable size, displaced 2 mm. An MRI arthrogram of the left shoulder was performed.
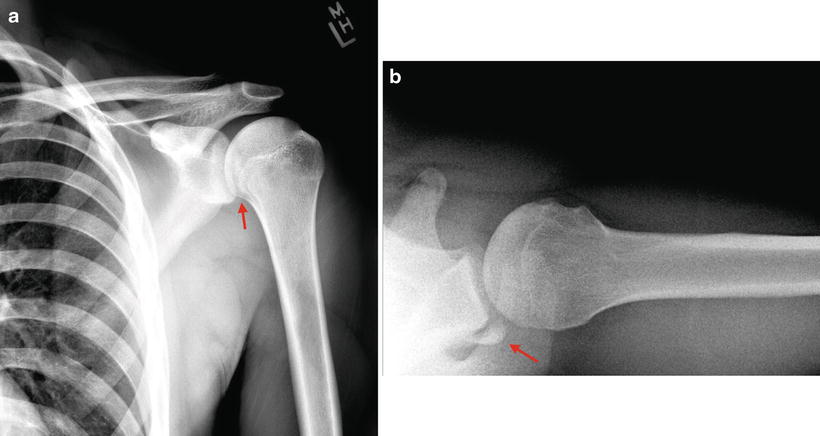
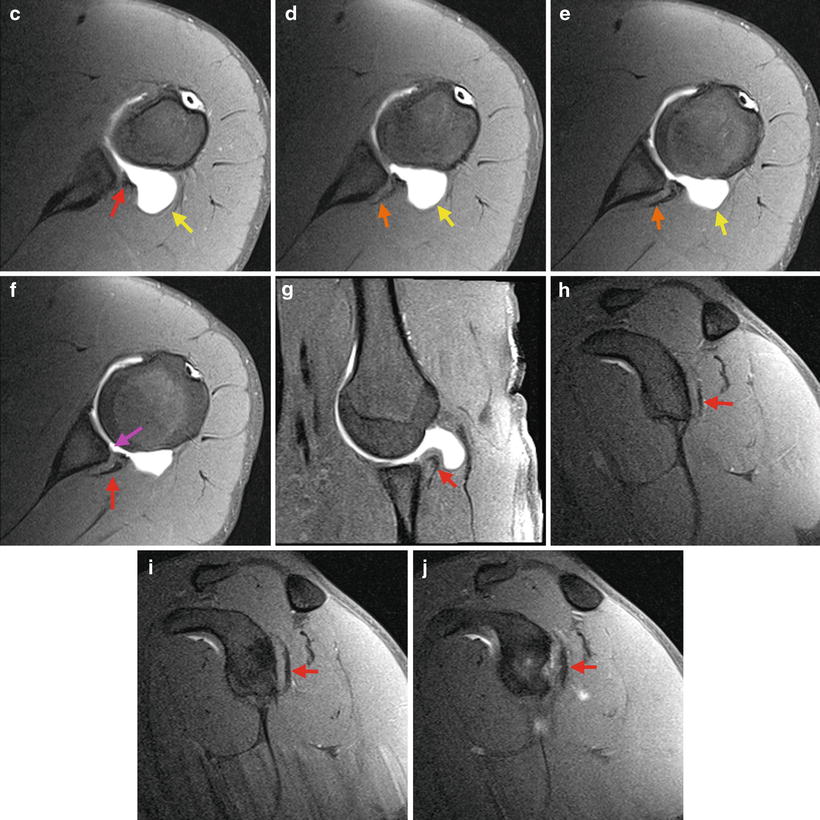
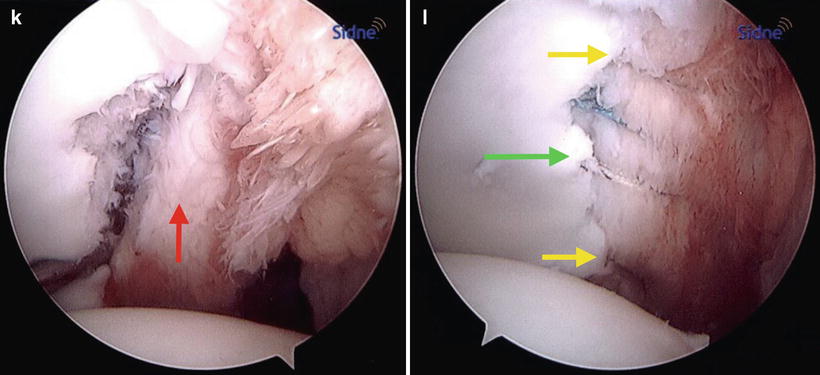
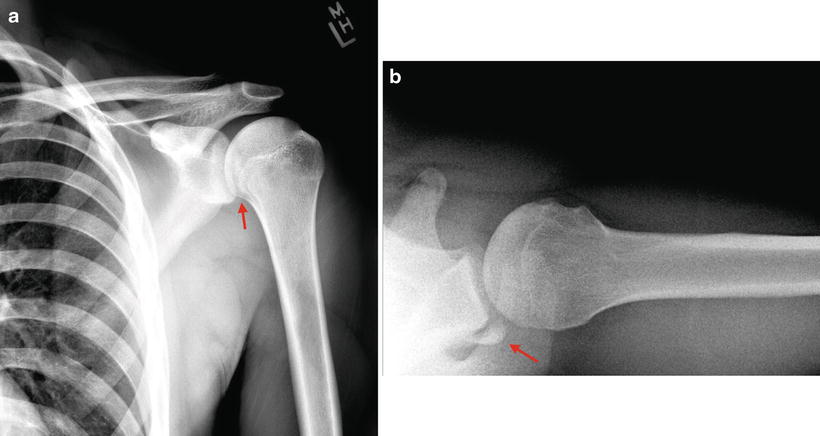
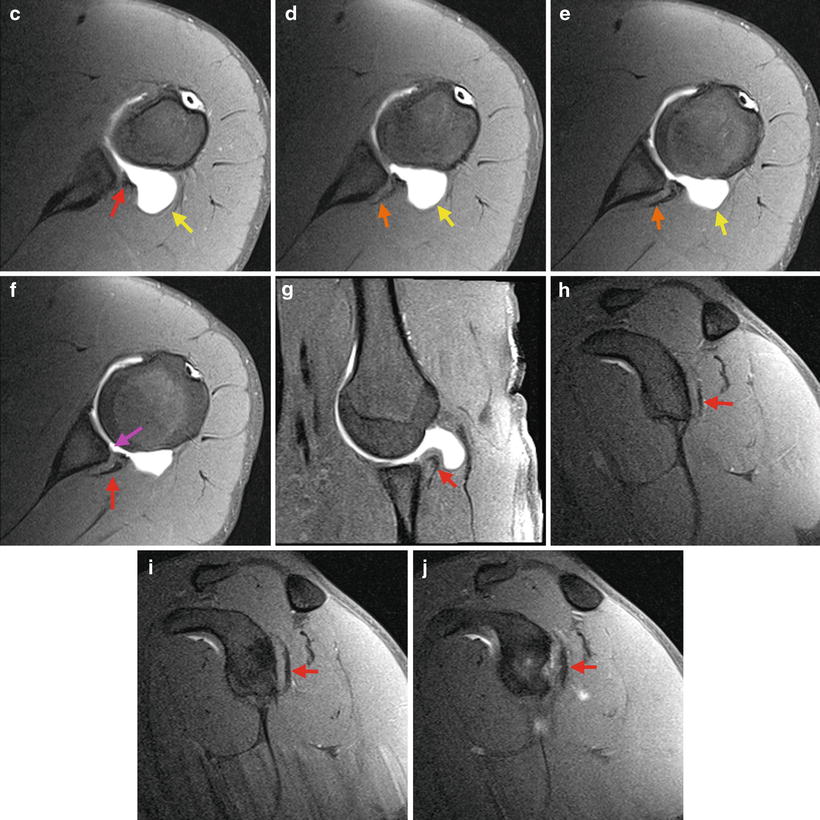
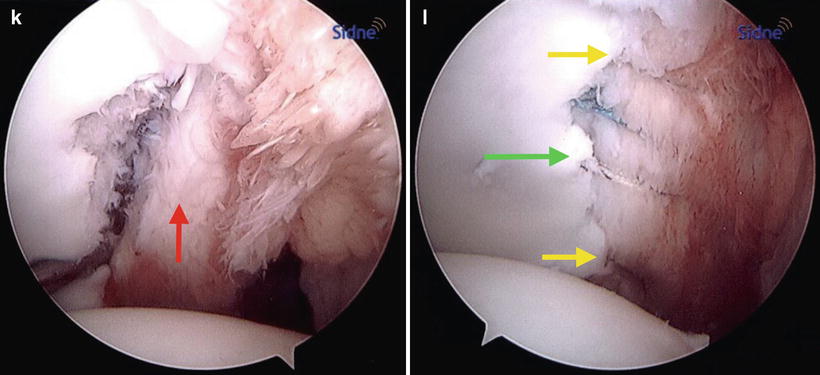
Fig. 13.2
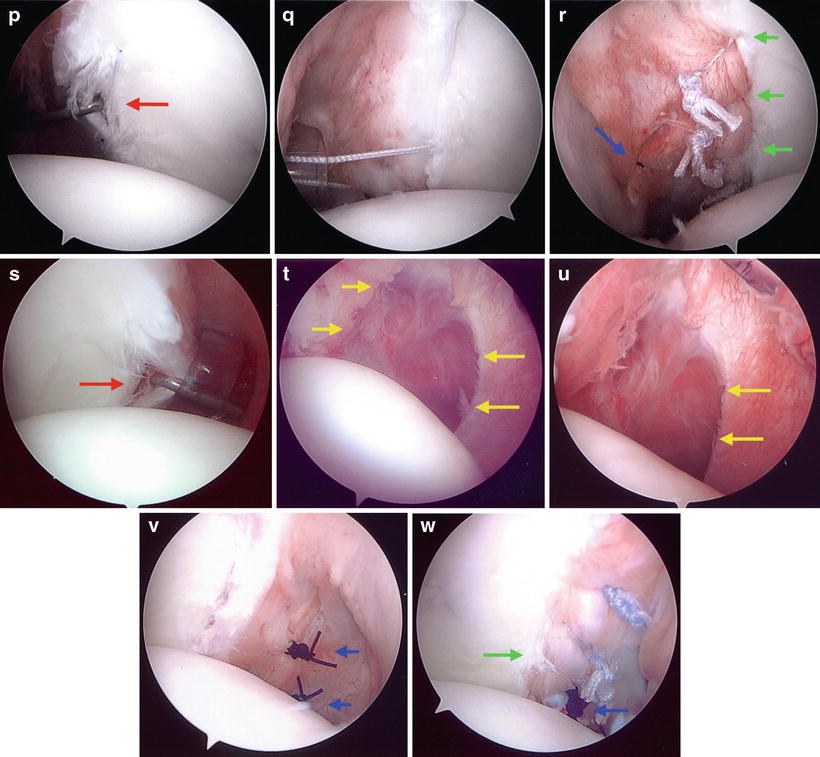
(a, b) AP and axial views X-rays of a left shoulder showing a reverse bony Bankart lesion with 2 mm of displacement (red arrows). (c–f) Axial T2 images with fat saturation showing a posterior glenoid fracture (red arrow) with an articular cartilage defect (pink arrow) and a chronic appearing tear of the posterior and posteroinferior labrum with avulsion of the posterior scapular periosteum (orange arrow) and a patulous posterior capsule (yellow arrow). (g) ABER position T1 fat saturation sequence showing a reverse bony Bankart (red arrow). (h–j) Sagittal T2 images with fat saturation showing a bony Bankart (red arrow). The area of the affected glenoid articular surface can be visualized. (k) Left shoulder with a reverse bony Bankart injury involving the entire posterior glenoid and associated posterior labrocapsular complex (red arrow). (l) Two-row construct repair around the reverse bony Bankart and associated labrocapsular complex (green arrow). Additional anchors were used to repair the labrum above and below this two-row construct around the bony fragment (yellow arrows)
Axial T2 images with fat saturation (Fig. 13.2c–f) show a posterior glenoid fracture with articular cartilage defect and a chronic appearing tear of the posterior and posteroinferior labrum with avulsion of the posterior scapular periosteum.
The ABER position T1 fat saturation sequence shows the reverse Bankart and the bony fragment in the most distal cuts (Fig. 13.2g). Sagittal T2 images with fat saturation (Fig. 13.2h–j) show the bony fragment and the area of the glenoid articular surface affected by the fracture.
There is no apparent femoral head lesion on the MRI. The bone marrow signal intensity is within normal limits. Other structures, like the biceps tendon, acromioclavicular joint, rotator cuff, and subacromial space, appear normal.
Having repeated posterior injuries on his left shoulder and imaging studies showing a posterior bony Bankart lesion, the patient was indicated for arthroscopy with posterior Bankart repair. An open repair was also considered, but because of the size of the bony lesion, it was anticipated that it could be addressed arthroscopically.
Arthroscopy
The procedure was performed in beach chair position under combined anesthesia. The left shoulder was examined under anesthesia showing a grade 1 posterior translation. The patient had full range of motion and was stable anteriorly.
A posterior arthroscopy portal was created slightly lateral to the standard position, and anterior and high rotator interval portals were made under needle localization.
Diagnostic arthroscopy revealed an intact rotator cuff and long head of the biceps. The patient’s subscapularis, anterior labrum, and superior labrum were normal. There were two small cartilage loose bodies in the axillary recess that were approximately 5–6 mm in diameter that were removed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree