8 Postoperative Findings and Follow-Up
Ventriculoperitoneal and Ventriculoatrial Shunts (Fig. 8.1)
Frequency: shunt malfunction is a common problem, with repeated failures reported to occur up to approximately every 18 months in a large group.
Suggestive morphologic findings: new occurrence of hydrocephalus (undershunting), bilateral subdural hygromas (overshunting).
Procedure: risk of irreversible brain damage; neurosurgical shunt revision.
Other studies: ultrasound when possible.
Checklist for scan interpretation:
 Evidence of shunt failure or slit ventricle?
Evidence of shunt failure or slit ventricle?
 Pathogenesis
Pathogenesis
Ventriculoperitoneal and ventriculoatrial shunts are used for the treatment of hydrocephalus in children. The following forms can occur:
• Congenital forms: aqueductal stenosis, Arnold-Chiari malformation, arachnoid cyst, and other cysts
• Acquired forms: postmeningitic, post-hemorrhagic, tumor-associated
The causes of shunt malfunction include:
• Displacement of the shunt
• Proximal obstruction of the shunt by ingrowth of choroid plexus or distal obstruction by fluid collections, etc.
 Clinical Manifestations
Clinical Manifestations
Shunt malfunction presents clinically with general signs of increased intracranial pressure, usually consisting of headache and impaired consciousness. Symptoms relating to the peritoneal or abdominal end of the shunt are also nonspecific.
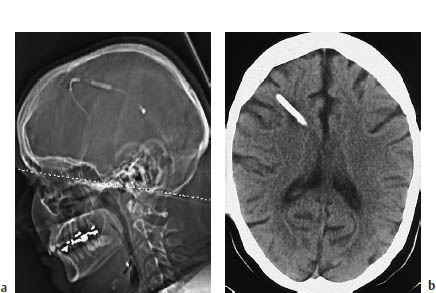
8.1a, b Ventriculoatrial shunt in a patient with hydrocephalus, caused by a pineal cyst (not shown).
The hallmark of undershunting is dilatation of the ventricular system compared with the previous examination. This may be accompanied by sulcal effacement. Overshunting (valve malfunction) leads to hygroma formation.
Cranial computed tomography (CT) should be supplemented by thoracic or abdominal CT to evaluate the peripheral limb of the shunt.
 Differential Diagnosis
Differential Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



