MR imaging has an important role in the evaluation of the postoperative foot and ankle. In this article, a variety of operative techniques and postoperative findings in the foot and ankle are described, including tendon and ligament reconstruction, as well as the treatment of tarsal coalition and Morton neuroma. The role of MR imaging in the assessment of complications of foot and ankle surgery is also detailed.
Key points
- •
MR imaging of postoperative tendon repair, reconstruction, and augmentation are potentially challenging examinations to interpret. Clinical history is important when interpreting these cases.
- •
Postoperative tendon appearance varies by time from surgery.
- •
There are a variety of operative approaches for lateral collateral ligament reconstruction.
- •
Abnormal findings on postoperative imaging may not correlate with symptoms.
- •
A variety of MR imaging sequences is used to differentiate osteomyelitis from other entities; in particular, the T1 sequence increases specificity.
Introduction
MR imaging of the postoperative ankle and foot can be challenging. The anatomy is compact with a variety of structures in close proximity. Additionally, postoperative changes may considerably alter expected anatomic relationships. Factors that inform imaging interpretation often stem from the primary diagnosis, subsequent management, intended therapeutic consequences, complications, and the current presenting symptoms. This article touches on a selection of surgical approaches to common ankle and foot problems, and their expected outcome. Possible complications will also be discussed. Although radiography is the principal imaging modality for postoperative imaging, MR imaging allows problem-solving in symptomatic and refractory cases, particularly when soft tissue disease is suspected. This discussion focuses on fundamentals of MR imaging technique and applications in the postoperative ankle and foot.
Introduction
MR imaging of the postoperative ankle and foot can be challenging. The anatomy is compact with a variety of structures in close proximity. Additionally, postoperative changes may considerably alter expected anatomic relationships. Factors that inform imaging interpretation often stem from the primary diagnosis, subsequent management, intended therapeutic consequences, complications, and the current presenting symptoms. This article touches on a selection of surgical approaches to common ankle and foot problems, and their expected outcome. Possible complications will also be discussed. Although radiography is the principal imaging modality for postoperative imaging, MR imaging allows problem-solving in symptomatic and refractory cases, particularly when soft tissue disease is suspected. This discussion focuses on fundamentals of MR imaging technique and applications in the postoperative ankle and foot.
MR imaging
MR imaging is the favored imaging modality for evaluating the ankle and foot following surgery because of the excellent contrast resolution. In particular, MR imaging is sensitive in evaluating postoperative bone marrow response and in evaluating surrounding soft tissues, including the tendons and ligaments.
MR imaging artifacts generated from implanted metallic objects in the magnetic field are a significant obstacle to obtaining clinically relevant postsurgical MR imaging. Magnetic field susceptibilities created by metals of varying properties, sizes, and orientations lead to signal shift away from the true position, in the form of signal loss, signal pile-up, and geometric distortion. This manifested artifact may obscure clinically relevant surrounding structures. Optimizing MR imaging technique to limit this artifact is, therefore, essential.
Many techniques exist to minimize metallic artifact, the simplest of which include selecting the appropriate field strength, selecting the appropriate sequences, and imaging in multiple planes. Because the degree of distortion increases with magnetic field strength, lower field strength magnets are advantageous. Fast (turbo) spin echo imaging is less susceptible to magnetic field inhomogeneity when compared with gradient echo imaging and is the foundation for most postoperative sequencing. Short tau inversion recovery imaging (STIR) is less susceptible to magnetic field inhomogeneity than frequency selective fat-suppression techniques, which often fail to uniformly fat suppress in the presence of metal. The utility of multiplanar imaging should not be underestimated; MR imaging metallic artifacts are not isotropic, meaning that artifact in 1 plane may be considerably less than in another.
Increasing receiver bandwidth to an acceptable level of signal-to-noise, using shorter echo spacing, reducing slice thickness, and implementing view angle tilting can each help further diminish metal-induced artifact. Multispectral techniques, such as multiacquisition variable-resonance image combination (MAVRIC) and slice-encoding magnetic artifact compensation (SEMAC), can be used at the trade-off of longer scan times, which can be shortened when combined with parallel imaging acceleration.
Routine postoperative imaging is generally performed without contrast. Postcontrast imaging with intravenous gadolinium can be incorporated into the MR examination for the appropriate clinical indications, which would include suspicion of mass or infection.
Separate imaging protocols tailored to evaluate the ankle, midfoot and metatarsals, and distal forefoot are preferred due to different optimal imaging planes for each region and due to postoperative clinical concerns that are unique to each region. The preferred short-axis imaging plane is directed through the talar dome at the ankle, through the metatarsals at the midfoot, and through the MTP joints or plantar plates at the forefoot. These protocols and imaging planes can be adjusted to address the clinical question and region of highest clinical interest.
Patients are imaged in the supine position, feet first, with slight passive plantar flexion. Standard MR examination of the ankle, midfoot, and forefoot is detailed using a high-definition foot and ankle array coil (Invivo, Gainesville, FL) on a 1.5 T GE (Boston, MA) magnet. The sequences and relevant sequence criteria are included in Tables 1–3 for the respective ankle, midfoot, and forefoot. In the setting of known postoperative metal or implants or failed fat-saturation at the time of imaging, the fat-saturated sequences included in the protocol are substituted with STIR sequences. In addition, the receiver bandwidth for the proton density (PD) sequences is doubled.
| Sequence | FOV (cm) | Slice Thickness (mm) | Slice Spacing (mm) | Matrix | NEX | TE | TR | TI | ETL | Receiver Bandwidth |
|---|---|---|---|---|---|---|---|---|---|---|
| Axial T2 | 12 | 3 | 1.0 | 256 × 192 | 2 | 100 | 3617 | — | 23 | 20.83 |
| Axial PD | 12 | 3 | 1.0 | 256 × 224 | 2 | 18 | 2050 | — | 13 | 31.25 |
| Coronal PD FS | 14 | 3 | 1.0 | 256 × 192 | 2 | 20 | 2234 | — | 11 | 20.83 |
| Sagittal T1 | 18 | 3 | 1.0 | 512 × 256 | 2 | Min Full | 500 | — | — | 20.83 |
| Sagittal IR | 16 | 4 | 0.5 | 320 × 192 | 2 | 50 | 4125 | 150 | 8 | 20.83 |
| Coronal PD | 10 | 4 | 0.0 | 512 × 256 | 3 | 36 | 1584 | — | 13 | 31.25 |
| Axial T2 FS | 12 | 3 | 1.0 | 256 × 192 | 2 | 100 | 3434 | — | 19 | 20.83 |
| Sequence | FOV (cm) | Slice Thickness (mm) | Slice Spacing (mm) | Matrix | NEX | TE | TR | TI | ETL | Receiver Bandwidth |
|---|---|---|---|---|---|---|---|---|---|---|
| Coronal PD FS | 14 | 3 | 1.0 | 320 × 192 | 2 | Min Full | 3417 | — | 6 | 20.83 |
| Axial T1 | 14 | 3 | 0.5 | 320 × 192 | 2 | Min Full | 617 | — | — | 15.63 |
| Axial IR | 14 | 3 | 0.5 | 256 × 192 | 2 | 50 | 4800 | 150 | 8 | 22.73 |
| Sagittal T2 | 14 | 3 | 0.5 | 320 × 192 | 4 | 102 | 2767 | — | 23 | 25.00 |
| Sagittal IR | 1 | 3 | 0.5 | 256 × 192 | 2 | 50 | 4800 | 150 | 8 | 22.73 |
| Sequence | FOV (cm) | Slice Thickness (mm) | Slice Spacing (mm) | Matrix | NEX | TE | TR | TI | ETL | Receiver Bandwidth |
|---|---|---|---|---|---|---|---|---|---|---|
| Axial IR | 14 | 3 | 0.5 | 320 × 160 | 2 | 50 | 4425 | 150 | 8 | 20.83 |
| Axial T1 | 14 | 3 | 0.5 | 320 × 192 | 2 | Min Full | 450 | — | — | 15.63 |
| Coronal T2 FS | 14 | 3 | 1.0 | 320 × 192 | 2 | 102 | 3117 | — | 6 | 19.23 |
| Coronal T1 | 14 | 3 | 1.0 | 320 × 160 | 2 | Min Full | 367 | — | — | 17.86 |
| Sagittal T2 | 14 | 3 | 0.5 | 320 × 192 | 4 | 102 | 3017 | — | 23 | 25.00 |
| Sagittal IR | 14 | 3 | 0.5 | 320 × 160 | 2 | 50 | 4425 | 150 | 8 | 20.83 |
Tendon repair and reconstruction
There are many tendon procedures involving the foot and ankle, many of which are named. MR imaging findings may be confusing, particularly if the surgical history is limited. A few principles help guide MR imaging interpretation. Tendons may be repaired directly, reconstructed with tendon graft, and/or augmented by nearby tendons. Augmentations may be the most difficult to evaluate on imaging because tendons may be rerouted, divided, and/or anchored at new locations to support the failed tendon.
Achilles and posterior tibialis reconstructions are relatively commonly performed. Augmentations and transfers may be accomplished with a variety of native tendons, including the flexor hallucis longus, flexor digitorum longus (FDL), and the peroneal tendons. Surgery on the anterior tibialis or extensor tendons constitutes a minority of cases, most often for lacerations or acute trauma.
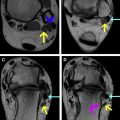
Three characteristics that distinguish injured or postoperative tendons from their normal counterparts are signal heterogeneity, signal intensity, and size. The MR imaging appearance of the postoperative tendon may never completely normalize. Typically, the heterogeneous signal seen in the postoperative tendon will become more uniform by 4 to 8 weeks. Postoperative tendon usually displays intermediate to hyperintense PD or T2 signal. Signal intensity should diminish with time, often stabilizing at intermediate to low-signal intensity. By 12 weeks, repaired tendon or graft may closely approximate the signal of the adjacent nonoperative tendon. It is unusual for a reconstructed tendon in the immediate postoperative period to match the size of a noninjured, preoperative tendon. The reconstituted tendon is most often enlarged, though the size may decrease over time. In general, compared with the preoperative injured tendon, a healed postoperative tendon exhibits less signal heterogeneity, lower signal intensity, and is smaller. Compared with an uninjured tendon, the postoperative tendon may retain modest signal heterogeneity, intermediate (but not high) PD-T2 signal, and enlargement.
Thus, it may be difficult to differentiate postoperative changes from tendinosis. In a study of Achilles tendon ruptures, Möller and colleagues reported poor correlation between clinical findings and those observed on postoperative ultrasound or MR imaging. The only significant imaging finding between operative and nonoperative groups was identified with ultrasound and this did not correlate to clinical measures of strength or range of motion.
Tendinosis is degeneration due to structural breakdown of collagen and other tendon components. The term tendinopathy is often used interchangeably with tendinosis. MR imaging findings in tendinosis include signal heterogeneity, tendon enlargement, and intermediate PD-T2 signal ( Fig. 1 ). Separately, the encasing tissues of a tendon may be abnormal. Most tendons in the ankle and foot have a synovial sheath, such as the flexor hallucis longus and FDL tendons. Tenosynovitis is inflammation of this sheath and is apparent on MR imaging as sheath thickening. There is typically abnormal fluid within the tendon sheath and surrounding edema. The Achilles tendon is distinct in the ankle because it possesses a paratenon, rather than a synovial sheath. The paratenon encloses the Achilles along its dorsal, medial, and lateral margins, and facilitates tendon gliding. Paratenonitis is invoked when there is thickening and edema signal of the paratenon.
Achilles Tendon
The Achilles is the largest tendon in the body. The bulk of Achilles surgery is undertaken for tendon rupture repair. Ruptures are typically spontaneous, occur during recreational sports, and may be attributed to eccentric loading while the gastrocnemius and soleus are maximally stretched (ankle dorsiflexed and the knee extended). Rupture is more frequent in men than women. Peak occurrence is in active 30- to 50-year-olds who are otherwise healthy.
Treatment is controversial with divergent reports supporting both operative and nonoperative approaches. The December 2009 workgroup of the American Academy of Orthopedic Surgery cites limited strength of recommendation for both operative and nonoperative treatment. The workgroup did reach a consensus recommendation that, when considering surgical repair, caution is warranted in patients with comorbidities such as diabetes, obesity, age above 65 years, sedentary lifestyle, and peripheral vascular disease. Young individuals and athletes are more likely to receive operative treatment.
Operative treatment depends on the acuity of the injury, the degree of tendon retraction, and resultant tendon gap. Acute tears with a small gap (less than 2 or 3 cm) may be amenable to end-to-end repair. In contrast, a chronic tear with a larger gap may require augmentation using nearby structures, such as the plantaris tendon or a flap from the gastrocnemius soleus complex. One technique uses a turn-down of gastrocnemius fascia, which is interwoven to span the torn tendon segment. There are multiple variations to this approach. A variety of tendon transfer procedures use nearby tendons, such as the flexor hallucis longus and peroneus brevis.
In either conservative or operative treatment scenarios, MR imaging reliably depicts tendon changes, from a healthy, uniformly low-signal structure to a thickened band with heterogeneous signal. Thickening may be diffuse or focal, most often in a fusiform configuration on sagittal sequences. Signal alterations change over time.
Peritendinous edema is atypical after a few months postsurgery. If present, this may indicate reinjury or ongoing tendinosis. Tendon defects or retears are evident as focal discontinuity of fibers and areas of hyperintense signal on fluid-sensitive sequences. Ossification within the tendon may be associated with retear and should be documented in the radiology report. This is represented by abnormal signal within the tendon substance that is isointense with marrow.
Haglund syndrome is another cause of posterior ankle pain involving the Achilles tendon and occasionally necessitates operative treatment. A prominent posterior calcaneal tuberosity and extrinsic compression via constrictive footwear, such as high heels, results in retrocalcaneal bursitis and insertional Achilles tendinosis. Surgical repair of Haglund syndrome involves osteotomy of the posterior calcaneus protuberance and resection of the inflamed retrocalcaneal bursa. The distal Achilles may be debrided and reanchored to the calcaneus. Postoperative tendon thickening and signal heterogeneity may be apparent on subsequent MR imaging, with anchors present within the calcaneus ( Fig. 2 ).