Techniques
Plain radiography
Plain radiographs are often used in the postoperative abdomen to evaluate lines and tubes, bowel gas pattern, retained foreign bodies, and the presence of pneumoperitoneum.
Fluoroscopy
Fluoroscopic upper gastrointestinal (GI) examination with water-soluble or barium enteric contrast can be used to evaluate for leaks in the areas of postoperative change. Depending on the institution, postoperative “leak studies” may be routine following certain procedures (such as roux-en-Y gastric bypass or sleeve gastrectomy). Fluoroscopic enema examination with water-soluble contrast can be used to evaluate a low anterior resection before diverting ostomy takedown. Loopograms can be used to evaluate ileal conduits following cystectomy if there is concern for stricture or recurrent disease.
Ultrasonography
Depending on the surgical procedure, ultrasound (US) can be used to image certain suspected postoperative complications. In the superficial soft tissues, ultrasound can be used to evaluate for localized fluid collections along the abdominal incision. Ultrasound can also be used to evaluate for large intraabdominal collections, although it has lower sensitivity in the detection of small volumes of fluid within the abdomen compared with computed tomography (CT).
Computed tomography
CT plays a crucial role in the diagnosis and management of a variety of postoperative abdominal complications.
Magnetic resonance imaging
Aside from magnetic resonance cholangiopancreatography (MCRP), magnetic resonance imaging (MRI) plays a limited role in the postoperative abdomen.
Protocols
Protocol considerations
- ◼
Fluoroscopic examination in the setting of a suspected leak should always be performed initially with water soluble contrast.
- ◼
If initial trial with water soluble contrast demonstrates no leak and suspicion for a leak remains low, barium may then be given.
- ◼
CT with intravenous (IV) and enteric water-soluble contrast is ideal in evaluating for postoperative fluid collections and other potential complications in the postoperative abdomen.
Suggested computed tomography abdomen/pelvis protocol
- ◼
Should extend from the dome of the diaphragm to the pelvic floor.
- ◼
At least 500 mL of dilute water-soluble oral contrast media given 1 hour before scanning.
- ◼
100 mL of IV contrast administered and scan performed in the portal-venous phase.
- ◼
For assessing complications from urinary collecting system related procedures (cystectomy, etc.), consider CT urography protocol instead.
Specific disease processes
Abdominal wall collections/hematomas
- ◼
Postoperative seromas may be differentiated from abscesses with their lower attenuation values, typically in the 12 to 24 Hounsfield unit (HU) range ( Figs. 37.1 and 37.2 ).

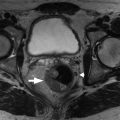
Fig. 37.1
Abdominal wall seroma. Axial unenhanced computed tomography image of the abdomen shows an abdominal wall fluid collection (seroma, asterisks ), located superficial to a renal transplant in the right iliac fossa.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)

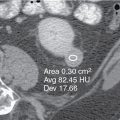
Fig. 37.2
Abdominal wall seroma and mesh. Axial contrast enhanced computed tomography image of the abdomen demonstrates a well-defined ventral wall seroma ( asterisks ), manifesting after ventral hernia repair with mesh ( arrowheads ), in a 51-year-old man.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)
- ◼
Infections involving the incision are reported to be as high as 15% to 25% ( Fig. 37.3 ).

Fig. 37.3
Abdominal wall abscess. Axial contrast-enhanced computed tomography image of the abdomen shows a complex pelvic collection extending into the abdominal wall in a 41-year-old woman that was secondary to pelvic inflammatory disease.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)
- ◼
Although more easily identified by clinical examination, cross-sectional imaging can identify a drainable collection early for percutaneous intervention/drainage.
- ◼
Rectus sheath hematomas may develop as the result of intraoperative injury to the epigastric vessels, and typically resolve within 2 weeks with conservative management ( Fig. 37.4 ).

Fig. 37.4
Abdominal wall hematoma. Axial contrast-enhanced computed tomography image of the abdomen demonstrates a hematoma in the anterior abdominal wall in a 32-year-old woman after cesarean section. The hematoma is below the arcuate line, demonstrates hematocrit effect ( asterisks ), and is associated with extraperitoneal extension of the hematoma into the space of Retzius ( arrowheads ).
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)
Imaging appearances
Ultrasonography
- ◼
Heterogeneous hypoechoic area with surrounding increase in vascularity.
- ◼
Extent may be underestimated if large enough.
Computed tomography
- ◼
Peripheral rim enhancement of a collection suggests organized infection.
Intraabdominal fluid collections
- ◼
Small volumes of fluid and pneumoperitoneum can be seen in the immediate postoperative period following open or laparoscopic surgery.
- ◼
Fluid is naturally absorbed by the peritoneal membrane, and should reduce spontaneously over the postoperative period.
- ◼
Most accumulations of fluid are sterile (seromas), representing reactive fluid, appearing crescent-shaped and unencapsulated.
- ◼
Abscess and pathologic fluid typically takes on an ellipsoid or spherical shape ( Fig. 37.5 ).

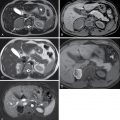
Fig. 37.5
Chylous ascites. A, Axial computed tomography (CT) in a 19-year-old man with extensive retroperitoneal adenopathy ( arrowheads ) from testicular cancer. Retroperitoneal lymph node dissection was performed. B, CT performed 3 months after surgery shows low-density ascites ( arrow ). Chylous ascites was found on paracentesis, indicating lymphatic leakage into the peritoneal cavity after lymph node dissection.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)

- ◼
Hematomas/hemorrhage and extravasated enteric contents (such as from anastomotic leak) tend to be of higher density ( Fig. 37.6 ).

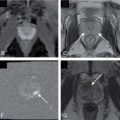
Fig. 37.6
Hemoperitoneum in a 57-year-old diabetic man who had laparotomy for infective aortitis. The patient became hypotensive after aortic graft placement. This axial computed tomography image shows aortic graft ( white arrowhead ), collapsed inferior vena cava ( dashed arrow ), and evidence of layered hemoperitoneum ( solid arrows ), indicating massive peritoneal bleeding. Bilateral ureteral stents ( black arrowheads ) are seen. Intravesical pressure was elevated at 28 mm Hg, indicating elevated intraabdominal pressure in keeping with abdominal compartment syndrome. Emergency decompressive laparotomy was performed, and the patient survived.
(From Sahani DV, Samir AE. Abdominal Imaging , ed 2. Philadelphia: Elsevier; 2017.)
Imaging appearances
Radiograph
- ◼
Not sensitive or specific for the detection of collections.
- ◼
Abnormal mass effect on bowel and gasless areas can be a secondary sign in the presence of a large enough collection.
Ultrasonography
- ◼
Can be used to follow large collections, especially if ionizing radiation is a concern (such as in the pediatric population).
Computed tomography
- ◼
Primary way of detecting and measuring intraabdominal fluid collections.
- ◼
Peripheral rim enhancement of a collection suggests infection ( Fig. 37.7 ).