Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
36.1 Introduction
36.2 Squamous Tumors
36.3 Glandular Tumors
36.3.2 Paget Disease
36.4 Mesenchymal Tumors
36.4.1 Vulvar Sarcomas
Abstract
Vulvar carcinoma is rare, accounting for 3–5 % of female tract cancers. Sixty-six percent of cases occur over the age of 70 years.
36.1 Introduction
Vulvar carcinoma is rare, accounting for 3–5 % of female tract cancers. Sixty-six percent of cases occur over the age of 70 years.
Over 85 % of malignant tumors are squamous cell carcinomas (SCC), followed by melanoma that accounts for 5–10 %.
Vulvar cancer is a visible and palpable disease and should be diagnosed early, but unfortunately 39 % of patients are diagnosed with advanced stages (III or IV).
36.2 Squamous Tumors
36.2.1 Vulvar Intraepithelial Neoplasia (VIN) (Dysplasia, Carcinoma In Situ)
Fifty percent of these women have other neoplasia involving the genital tract, most often cervical intraepithelial neoplasia.
Fifty percent have a history of a preexisting or concomitant sexually transmitted disease, of which condylomata acuminata is the most frequent.
Most patients are symptomatic with pruritus.
36.2.2 Invasive Squamous Cell Carcinoma
36.2.2.1 Etiology
There are three main groups of patients:
1.
Women (mean age, 55 years) who have VIN associated with squamous cell carcinoma. They have a high rate of cervical and vaginal neoplasia. They tend to be heavy cigarette smokers. The tumors are predominantly of the warty or basaloid types. HPV is detected in 75 % of cases.
2.
Older women (mean age 77 years) who do not have associated VIN, but often have vulvar dermatoses especially lichen sclerosus. They do not have a history of heavy cigarette smoking. The tumors are well-differentiated keratinizing squamous cell carcinomas. They rarely contain HPV.
3.
Women with chronic granulomatous disease, mainlygranuloma inguinale.
Diabetes mellitus, immunosuppression, and achlorhydria may be associated with vulvar squamous cell carcinoma.
36.2.2.2 Special Histological Subtypes
Different subtypes of SCC exist; among them is verrucous carcinoma [1].
Verrucous carcinoma is a well-differentiated squamous cell hyperkeratotic epithelial tumor.
It is predominantly locally invasive neoplasia. The condition may occur in young women.
The prevalence is estimated to be 6.5 % among malignant lesions of the vulva.
The diagnosis is based on extensive vulvar pruritus, similar to squamous cell carcinoma.
Warty carcinoma (condylomatous carcinoma) is frequently associated to HPV type 16.
36.2.2.3 Clinical Features
Women presenting with vulvar carcinoma may have a wide variety of presenting complaints relevant to the vulvar tumor, especially if the tumor is at an advanced stage.
No symptoms in 20 % of cases
Long history of pruritus: ++++
Itching, burning, and soreness
A lump or mass on the vulva: +++, or a wite hyperkeratotic plaque
Painful urination
Bleeding or bloodstained vaginal discharge
36.2.2.4 Site of the Tumor
Most often in the labia majora and the labia minora
But can be found anywhere on the vulva: clitoris, fourchette
36.2.2.5 Diagnosis
Classical procedure:
Pelvic clinical examination under anesthetic
Colposcopy
Biopsy (punch or excisional)
36.2.2.6 MR Imaging [2–4]
Primary Tumor
The tumor is best seen on T2-weighted sequences as intermediate signal intensity mass or thickening of the vulvar skin (Figs. 36.1 and 36.2). The relationship of the tumor to the clitoris, urethra, vagina, and anus is important prognostically. If deep invasion is suspected, T2-weighted images in the sagittal or coronal planes can be helpful to assess the cranial extent of tumor.
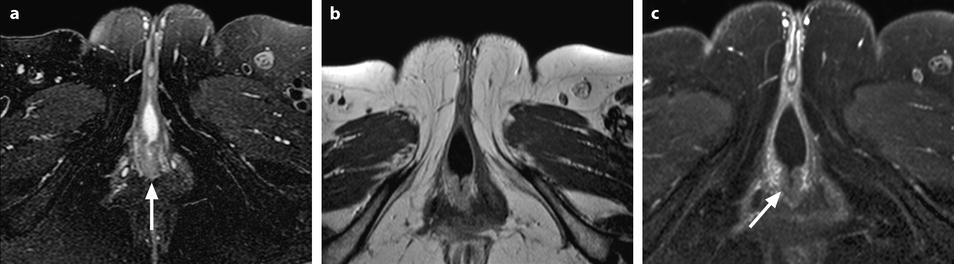
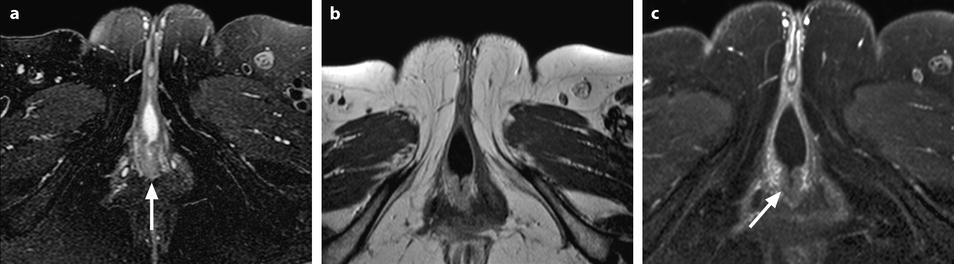
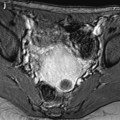
Fig. 36.1
Squamous cell carcinoma of the posterior fourchette (stage IA). Forty five year-old woman with a clinical ulcerated mass of the vulva. Vulvovaginal opacification. On Axial T2W-FS (a), a “horseshoe” tumor of the fourchette (arrow), of intermediate signal, less than 2 cm in diameter, regular, and well confined is displayed (c). On axial T1 (b), and after injection of gadolinium (c), the tumor slightly enhances (arrow in c), and does not extend to the adjacent perineal structures. A normal left inguinal lymphnode is depicted on the different sequences. At pathology resection of the tumor was stage 1A; sentinel ymph nodes were negative
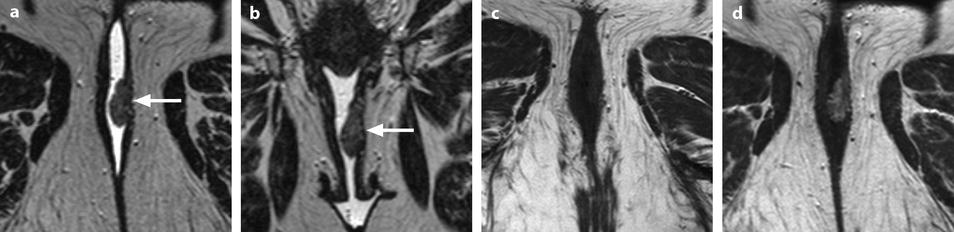
Fig. 36.2
Squamous cell vulvar carcinoma (stage IB). A 69-year-old woman with clinically left minor labia tumor. (a) Axial T2W of the anterior vulva, (b) coronal T2W in front of the vagina and uretral orifice, corresponding, (c) axial T1W, and (d) axial gado-T1W images, after vulvo-vaginal opacification, show a left minor labia tumor (arrows) partially surrounded by gel, 2.5 cm in largest diameter. It has intermediate signal intensity on T2W images and a hypointense signal on T1 image and enhances after gadolinium injection. Radical vulvectomy was performed. At pathology, left sentinel lymph nodes were negative; the tumor was 2.5 cm in size and corresponded to an infiltrative squamous cell carcinoma
Invasion is indicated by replacement of the relatively hypointense muscular coast of the urethra, vagina, or anorectum by intermediate signal intensity tumor, contiguous with the vulvar primary tumor.
Pitfalls of MRI
Stage I cancer may be too small to be detected on MRI.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree