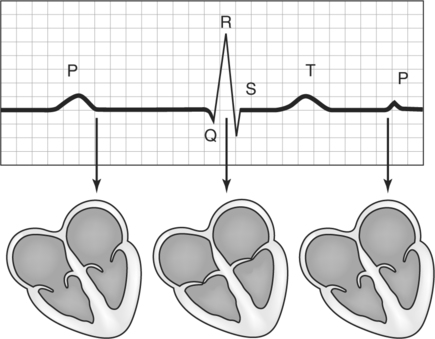
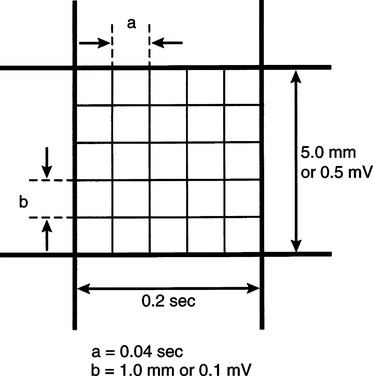
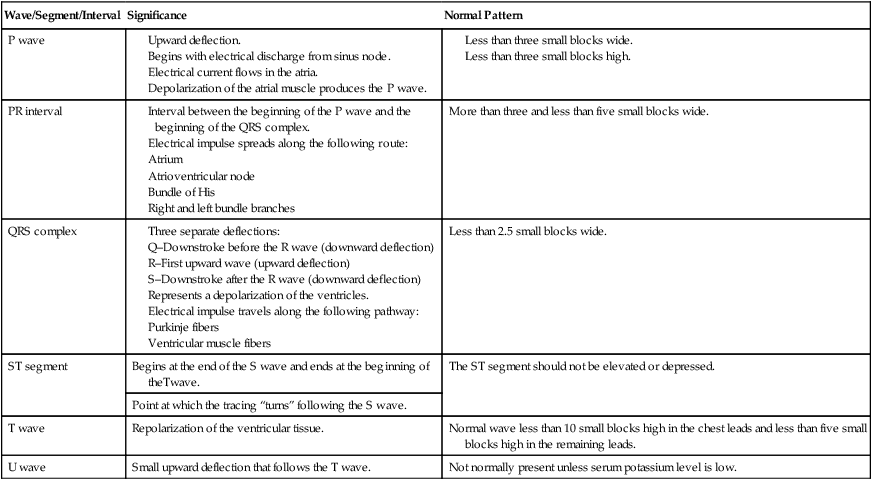
CHAPTER 8 After completing this chapter, the reader will be able to perform the following: Angiography is defined as “the x-ray visualization of the internal anatomy of the heart and blood vessels after the intravascular introduction of radiopaque contrast medium.”1 The contrast medium is introduced by an intravenous or intra-arterial injection or through a catheter that is inserted into a peripheral vessel and guided to the desired target area. In January 2003 the American Registry of Radiologic Technologists (ARRT) introduced two postprimary advanced level examinations to replace its existing cardiovascular–interventional technology examination: vascular–interventional and cardiac–interventional technology examinations. (See www.ARRT.org for content specifications and additional information.) Although the diagnostic portion of the procedures plays an important part of the total patient care, the field of interventional (therapeutic) radiology is rapidly becoming the primary focus of the radiographer’s responsibilities in the advanced procedure field. The techniques learned and practiced in the diagnostic studies are critical to the understanding and practice of interventional procedures. The amount of oxygen that is bound to the hemoglobin contained in the red blood cell can easily be monitored throughout the procedure. It is accomplished noninvasively by means of a pulse oximeter and provides real-time information regarding the oxygen saturation. The physiologic process is the binding of hemoglobin and oxygen to form oxyhemoglobin (HbO2). Pulse oximetry provides a measurement of the oxyhemoglobin saturation of the arterial capillaries (SaO2). The measurements are made by means of a sensor that is attached to the patient’s finger or toe. Figure 8-1 illustrates the TruSat pulse oximeter manufactured by Datex-Ohmeda. This system has a display range from 0% to 100% displayed on a highly visible backlit screen. It provides a measurement of the oxyhemoglobin saturation (SpO2) value and pulse rate. This unit is also equipped with both audio and visual alarms for SpO2 and pulse rate limits. Standard locations on the body for these electrodes are the right and left arms, right arm and left leg, and left arm and left leg. Each segment of the ECG shows the electrical cycle of the heart (Fig. 8-2). The P wave initiates the cycle, and the excitation spreads from the sinoatrial node over the atrium to the atrioventricular node. Peaks Q, R, and S follow as the impulse spreads throughout the atrioventricular bundle of His over the ventricles. At this time, the heart is in ventricular systole. Finally, as ventricular excitation subsides, the T peak is recorded. The U wave is not usually attendant in the normal ECG; it is usually present when the serum potassium level is low and appears as a small upward wave. The small and large blocks on the ECG paper and tracing illustrate the interval in seconds (horizontal blocks) and the measurement of electrical activity in millimeters (vertical blocks) of the wave. Each of the small horizontal blocks represents 0.04 s on the horizontal line and 1 mm on the vertical line (Fig. 8-3). Because each of the large blocks comprises five horizontal and five vertical blocks, its value can be stated as 0.2 s (0.04 s × 5 = 0.2 s) horizontal and 5 mm (1 mm × 5 = 5 mm) vertical. The vertical height is correlated to the electrical activity. Five millimeters of height (one large block) is equal to 0.5 mV of electrical activity. Table 8-1 summarizes the normal ECG tracing and lists the wave, segment, or interval, the significant physiology, and how the normal pattern should be represented on the ECG paper. TABLE 8-1 Summary of the Normal Electrocardiogram
Principles of Angiography
 Describe the historical background of angiography
Describe the historical background of angiography
 List and describe the methods of patient monitoring
List and describe the methods of patient monitoring
 Define the principles of pulse oximetry
Define the principles of pulse oximetry
 Describe the basic principles of electrocardiography
Describe the basic principles of electrocardiography
 Identify the method for evaluating the electrocardiogram tracing
Identify the method for evaluating the electrocardiogram tracing
 Identify some common cardiac arrhythmias
Identify some common cardiac arrhythmias
 Identify and describe the various means for obtaining vessel access
Identify and describe the various means for obtaining vessel access
 Describe the procedure for the Seldinger technique for vessel puncture
Describe the procedure for the Seldinger technique for vessel puncture
 Describe the various arterial and venous access approaches
Describe the various arterial and venous access approaches
 Describe the direct exposure of an artery or vein for vessel access
Describe the direct exposure of an artery or vein for vessel access
HISTORICAL PERSPECTIVE
MONITORING TECHNIQUES
Physiologic Monitoring
Pulse Oximetry (Oxygen Saturation)

BASIC PRINCIPLES OF ELECTROCARDIOGRAPHY
Wave/Segment/Interval
Significance
Normal Pattern
P wave
PR interval
More than three and less than five small blocks wide.
QRS complex
Less than 2.5 small blocks wide.
ST segment
Begins at the end of the S wave and ends at the beginning of theTwave.
The ST segment should not be elevated or depressed.
Point at which the tracing “turns” following the S wave.
T wave
Repolarization of the ventricular tissue.
Normal wave less than 10 small blocks high in the chest leads and less than five small blocks high in the remaining leads.
U wave
Small upward deflection that follows the T wave.
Not normally present unless serum potassium level is low.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine