Fig. 33.1
A variety of activities, such as a water skier being pulled forward, can result in proximal hamstring rupture
Oftentimes, the patient reports a history of a “pop” or a series of “pops” and when asked to localize the pain points to the proximal lower gluteus and proximal posterior thigh. Initially the injury can seem innocuous, and the inexperienced clinician may falsely diagnose these injuries as a hamstring muscle strain. However, with a suspicious mechanism of injury, such as a slip on a wet floor and a history of a pop, the clinician should error on the side of caution and order an MRI to assess the level and severity of the injury.
Usually within 48–72 h, a significant ecchymosis is apparent in the midthigh region, which quickly darkens and extends distally sometimes all the way to the foot (Fig. 33.2). While some mild ecchymosis may occur in a mid hamstring muscle strain, it is nowhere near the severity and size of the ecchymotic changes seen in a proximal hamstring avulsion injury.


Fig. 33.2
Ecchymosis following a complete proximal hamstring avulsion
Although hamstring strains reliably heal after a period of rest and dedicated physiotherapy, nonoperative management of complete ruptures and high-grade partial ruptures may result in low return to sports, persistent pain, weakness, and instability [5–9]. While the natural history of partial tears is not clearly defined, certain partial tears, particularly those with retraction greater than 2 cm and tendinous detachment greater than 50 %, have also been shown to do poorly with nonoperative management [9–11].
Given the unreliable results with nonoperative management, the trend has been toward open repair with suture anchor fixation as the surgical method of choice [2, 5, 9, 10, 12–17]. This can be performed through either a transverse or vertical incision. Whereas open repair leads to high rates of good and excellent outcomes in both the acute and chronic setting [18, 19]; complications include wound dehiscence 2.4 % [20], wound infection 1–2.4 % [16, 20, 21], seroma 2.4 % [20], posterior cutaneous neuralgia 9.8–40 % [15, 20], hypertrophic scar formation 2.0 % [16], wound fistula 1.1 % [11], incisional numbness 60.9 % [12], and cosmetic deformity 60.9 % [12].
Arthroscopic and endoscopic techniques have been used throughout sports medicine in an effort to minimize surgical incisions, decrease morbidity, and speed recovery. In an effort to mitigate the potential morbidity of an open repair, advanced surgical techniques have allowed us to endoscopically treat some of these injuries to the proximal hamstring. Here we present a case example of one of our patients treated with endoscopic repair of a proximal hamstring injury.
Case Description
The patient is a very active 53-year-old female who presented 6 weeks months after sustaining an injury to her right hamstring while sprinting during a soccer match. She attempted rest and rehabilitation but complained of persistent pain, weakness, and inability to return to explosive acceleration required in sports that she enjoyed including recreational soccer. The exertional symptoms included cramping of the mid-substance hamstring musculature as well as sharp pain and sitting intolerance at the ischial tuberosity region. On physical examination, she had tenderness over the ischial tuberosity with a small palpable defect over the proximal hamstring origin. She had pain with resisted knee flexion and slightly decreased sensation in the sciatic nerve distribution. MRI revealed a high-grade partial avulsion with approximately 2 cm of retraction (Fig. 33.3a, b). Given that she had failed conservative management and desired to return to soccer, she elected to undergo proximal hamstring repair, and an endoscopic approach was discussed as an option.
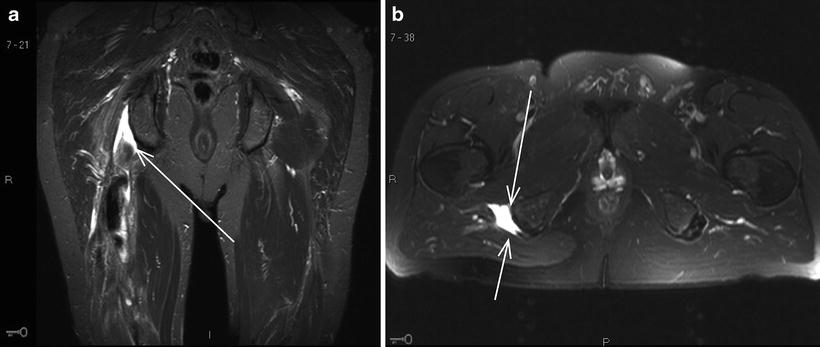
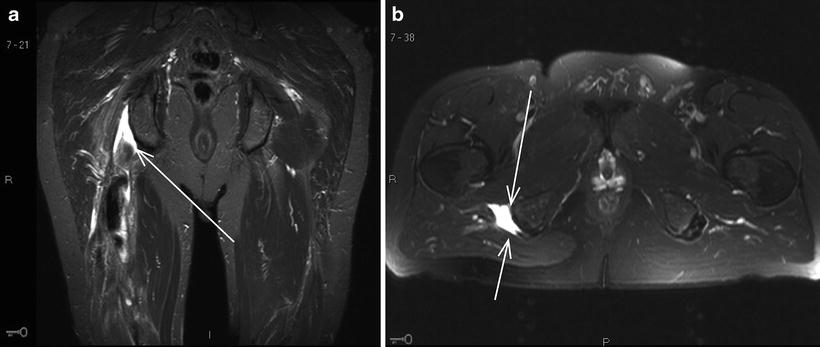
Fig. 33.3
(a, b) MRI of proximal hamstring avulsion: coronal and axial views
Under general endotracheal tube anesthesia, the patient was placed in the prone position with the gluteal and posterior thigh prepped and draped. The first portal, the direct posterior portal, was made in the gluteal crease over the proximal hamstrings. The arthroscope was placed into the subgluteal space and, using a low-pressure pump, the space was insufflated with fluid; the subgluteal is defined as the space between the gluteus maximus and proximal hamstring fascia. Under direct visualization, a second portal, the posterolateral portal, was made in the gluteal crease just lateral to the first portal, directly over the lateral facet of the ischial tuberosity. An arthroscopic shaver was carefully used to debride the ischial bursa and develop the subgluteal space (Fig. 33.4). Working laterally, the shaver was used bluntly to identify the sciatic nerve. Several adhesions were bluntly dissected from the sciatic nerve. Care was taken to avoid damage to the sciatic nerve throughout the remainder of the case. Next, the ischial tuberosity and proximal hamstring ruptured fibers were visualized (Fig. 33.5). Approximately 60 % of the tendon footprint was detached and retracted. All scar tissues were debrided. The torn and retracted fibers were thoroughly debrided and “freshened” in an effort to enhance healing upon refixation. A combination of clear cannulas and Passport cannulas was placed into each of the portals. The dissection using the motorized shaver was carried distally 4–5 cm which was helpful in mobilizing the tendon stump and would allow easier reduction to the footprint. An arthroscopic grasper was used to assess mobilization of the tendon (Fig. 33.6). Next, a single 4.5 mm double-loaded poly-ether-ether-ketone (PEEK) corkscrew anchor was used (Arthrex, Naples, FL), and sutures were passed using a combination of angled crescent suture passers and the Scorpion Fastpass suture passer device (Arthrex, Naples, FL). A horizontal mattress configuration was made. A second anchor was placed, and similar suture passing through the proximal hamstring tendon was performed. With the knee flexed, the tendon was easily reduced to the bone using standard arthroscopic suture technique and then tied in place (Fig. 33.7). Solid reduction and fixation were confirmed while flexing and extending the knee.

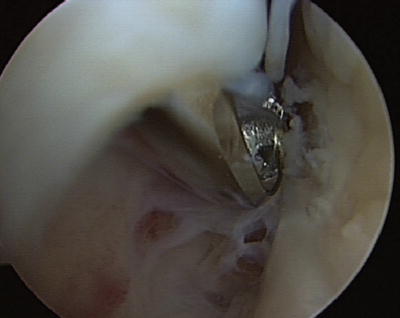
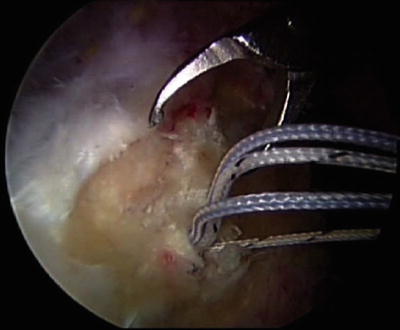
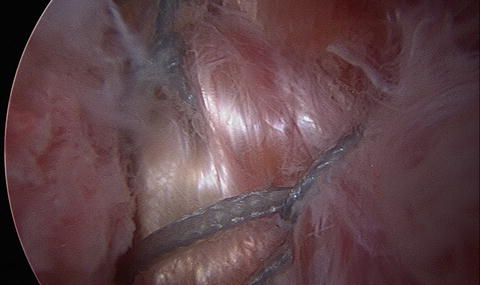

Fig. 33.4
Subgluteal space. Potential space between the gluteus maximus and proximal hamstring fascia
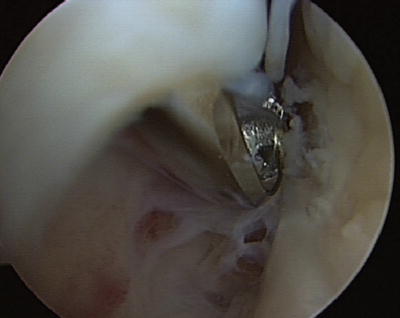
Fig. 33.5
Arthroscopic shaver debriding the empty footprint of the ischial tuberosity at site of avulsed proximal hamstring fibers
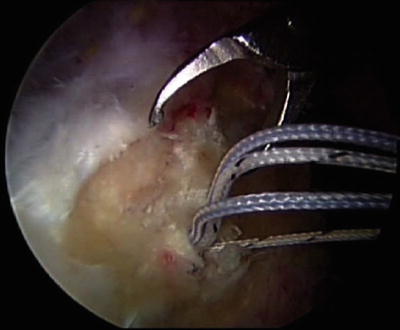
Fig. 33.6
Mobilization of avulsed proximal hamstring tendon
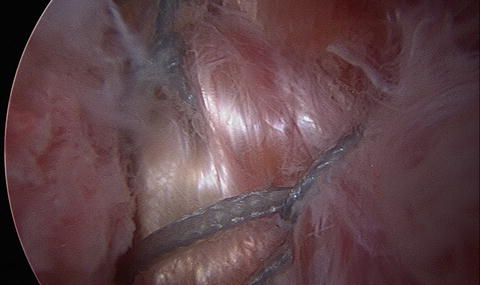
Fig. 33.7
Repaired proximal hamstring fibers reduced to anatomic footprint of ischium
The patient was discharged home the same day. Aspirin 325 mg was used for 1 month for DVT prophylaxis. A hinged knee brace initially locked in 70° of flexion was progressively brought into full extension over the next 10–14 days. The patient was kept non-weight bearing until full extension was achieved. Weight bearing was then gradually progressed to full by 6 weeks, and crutches were abandoned. Physical therapy and range of motion exercises were initiated at this point. Strengthening exercises began at 12 weeks with progressive return to sport at 4–6 months. Final follow-up was 1 year after the surgery. The patient had normal muscular contour, full strength, and range of motion and had returned to competitive recreational soccer at the same level as prior to the injury. The numbness that was experienced preoperatively had resolved.
Discussion Points
Anatomic Considerations of the Proximal Hamstring Region
The anatomy of the proximal hamstring is important to review as it has significant implications particularly when attempting surgical intervention whether in an acute or chronic setting. The two most important anatomic considerations involve the sciatic nerve and the true anatomic footprint of the proximal hamstring tendon.
The sciatic nerve courses in close approximation to the proximal hamstring origin at the ischial tuberosity. The sciatic nerve is located just lateral to the proximal hamstring and proceeds to course distally before arborizing and sending branches to each of the muscle bellies of the hamstring complex. The sciatic nerve has two distinct bundles at the proximal level called the tibial branch and the peroneal branch. The tibial branch supplies innervation to the three main muscles of the hamstring complex including the semimembranosus, semitendinosus, and the long head of the biceps femoris. The short head of the biceps femoris muscle is innervated by the peroneal branch of the sciatic nerve, but it is important to note that the short head of the biceps femoris does not contribute to the proximal hamstring tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree