Table 21.1 Disease entities that can manifest as solitary pulmonary nodule2 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
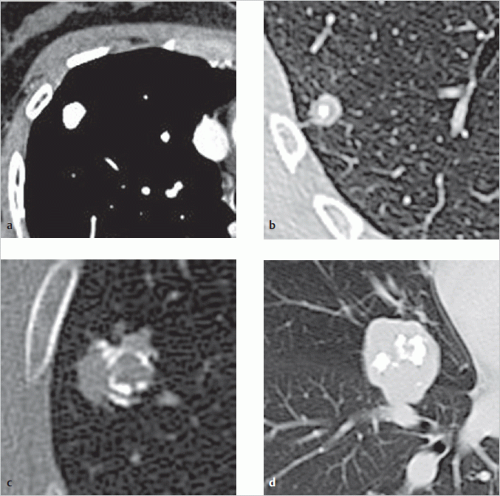 Fig. 21.1 Benign calcification patterns in nodules. (a) Homogeneous calcification. (b) Central calcification. (c) Lamellar calcification. (d) Popcorn-like calcification. |
|
If previous images show at least 2-year nodule stability.
If an extrapulmonary location of the nodule is suspected (e.g., mammillary shadows or rib osteoma; this can be further explored on chest radiography using mammilla markings or rotational fluoroscopy, thus with markedly lower radiation exposure than on CT). CT is often able to visualize small, incidentally detected, nodules not found
on chest radiography or only identifiable retrospectively in relation to the CT findings. Several lung cancer screening studies with low-dose CT have already produced extensive data on the potential malignancy of incidentally detected nodules. At least one nodule was identified on CT in up to two-thirds of all study participants at high risk for lung carcinoma. The majority of these nodules were very small. In all studies, more than 95% of these pulmonary nodules proved to be benign.
| ||||||||||||||||||||||||||||
History of smoking (smoker, current or during the previous 10 years, passive smoker).
History of known malignant tumor.
Family history of lung cancer.
Chronic obstructive pulmonary disease.
Lung fibrosis.
Inhalation exposure to:
Asbestos.
Quartz.
Cadmium.
Arsenic.
Beryllium.
Nickel.
Chromium.
Polycyclic aromatic hydrocarbons.
Radioactive substances such as uranium or radon.
Nodules with a mean diameter (average of longest diameter and diameter perpendicular to the longest diameter, rounded to the nearest full millimeter) of less than 6 mm in patients with no risk factors have such a low risk of malignancy that no further investigation or follow-up is recommended. In persons with known risk factors or if the nodule looks morphologically suspicious, a 12-month follow-up CT scan can be performed.
If a decrease in the size of a nodule has been observed during follow-up or the nodule disappears completely, follow-up is no longer required. Nodule benignity is just about proven.
If there is evidence of nodule stability, follow-up is advisable at variable intervals tailored to the individual risk.
Progressive growth of a nodule during follow-up is suggestive of malignancy and normally needs further investigation (histologic confirmation).
diagnostic work-up should be considered. A multidisciplinary decision on necessary diagnostic measures is recommended, with pneumonologists and thoracic surgeons taking into consideration the aspects listed in ▶Table 21.3. There is no need for further invasive investigation if malignancy appears unlikely in the context of the described morphology criteria. This may also apply in the individual case if PET or contrast dynamic CT yield a negative result.
Medical risk and general condition: If an invasive procedure presents an increased medical risk, caution is exercised when indicating biopsy, especially for nodules with low probability of malignancy. Instead, follow-up is generally recommended and invasive diagnostic exploration is advisable only if there is nodule growth.
Operability: The technical and functional operability are estimated. The latter can be decisive for the choice of ensuing procedure if, as in the case of a central pulmonary nodule, surgery is expected to result in major lung volume loss.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree