Pulmonary Venoocclusive Disease
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Rare cause of pulmonary hypertension due primarily to occlusion of post-capillary venous radicles
Imaging Findings
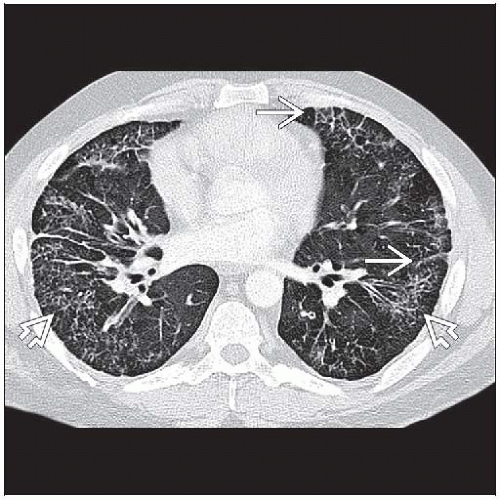
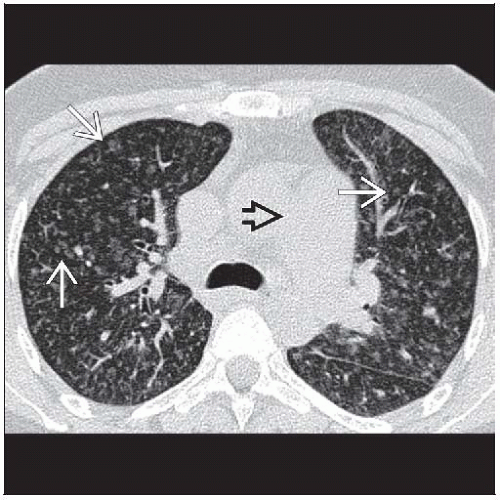
Pulmonary arterial hypertension + smooth interlobular septal lines
Centrilobular ground-glass opacities and septal thickening have random distribution within lung
Thickened interlobular septa (80%), smooth
Centrilobular ground-glass opacities (65%)
Presence of 2 or more findings (lymphadenopathy, septal thickening, centrilobular ground-glass opacities)
Sensitivity 75% and specificity 85% for PVOD
Top Differential Diagnoses
Pulmonary Hypertension
Mediastinal Fibrosis
Pulmonary Capillary Hemangiomatosis (PCH)
Pathology
Etiology: Idiopathic, post bone marrow transplant, chemotherapy drugs
Unknown incidence: PVOD may account for up to 10% of cases of PPH
Pathologic hallmark: Extensive occlusion of pulmonary veins by intimal thickening
Some evidence that proliferation of thin-walled capillaries in PCH histologic reaction to PVOD
Clinical Issues
Normal pulmonary capillary wedge pressure: Hallmark of PVOD
Prognosis very poor: Most patients die within 2 years of diagnosis
TERMINOLOGY
Abbreviations and Synonyms
Pulmonary venoocclusive disease (PVOD), pulmonary vasoocclusive disease
Isolated pulmonary venous sclerosis, obstructive disease of pulmonary veins, venous form of primary pulmonary hypertension, pulmonary artery hypertension (PAH)
Definitions
Rare cause of pulmonary hypertension due primarily to occlusion of post-capillary venous radicles
IMAGING FINDINGS
General Features
Best diagnostic clue: Pulmonary arterial hypertension + smooth interlobular septal lines
Patient position/location: Centrilobular ground-glass opacities and septal thickening have random distribution within lung
CT Findings
Lung
Ground-glass opacities common (100%) but nonspecific
Centrilobular (65%), most specific pattern
Geographic (50%)
Diffuse
Mosaic
Perihilar
Patchy
Thickened interlobular septa (80%), smooth
Range from few to numerous
Peribronchovascular bundle thickening
Distribution of septal thickening and ground-glass opacities: Random
Lymph nodes
Mild lymphadenopathy, mean 15 ± 5 mm (50%)
Pulmonary vasculature
Enlarged main and central pulmonary arteries
Pulmonary vein caliber normal
Cardiac
Dilated right atrium and right ventricle
Thickened right ventricular myocardium
Left ventricle and atrium have normal dimensions
Pleura-pericardium
Pleural effusions (20-40%) may be bilateral, usually small
Pericardial effusion (10%), small
Accuracy
Presence of 2 or more findings (lymphadenopathy, septal thickening, centrilobular ground-glass opacities)
Sensitivity 75% and specificity of 85% for PVOD
Presence of only 1 finding cannot rule out PVOD
Life-threatening pulmonary edema
May follow vasodilator therapy for primary pulmonary hypertension (PPH)
Vasodilators include continuous intravenous infusion prostacyclin (epoprostenol) and calcium channel blockers
Patients with centrilobular ground-glass opacities and septal lines at highest risk
Radiographic Findings
Nonspecific
Enlarged pulmonary arteries (100%)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree