Quality Assurance of Nuclear Medicine Instrumentation
Kai Lee
LEARNING OBJECTIVES
1. Understand the rationale for each quality assurance procedure.
2. Learn the test procedures to monitor the equipment performance.
3. Familiarize with the results and abnormalities found in quality assurance tests.
INTRODUCTION
Accuracy and consistency are important goals for diagnostic nuclear medicine. Achievement of these goals requires artifact-free capable equipment appropriate for the patient’s condition. Regulatory and accreditation agencies also require the equipment to be assured of functioning properly before administration of radiopharmaceutical to safeguard unnecessary radiation to the patient. A quality assurance (QA) program includes a set of test and evaluation procedures to evaluate the performance of the imaging or counting equipment such that it meets or exceeds established reference standards. For a QA program to be effective, the tests must be performed regularly at the appropriate frequencies, requiring only simple apparatus, a short time to perform, with critical analysis of the test results. This chapter presents an overview of QA tests for the imaging equipment, including the gamma cameras, single photon emission computed tomography (SPECT)/computed tomography (CT), and positron computed tomography (PET)/computed tomography (CT) (1,2). A summary of the frequency of the recommended QA tests is given in Table 18.2 at the end of the chapter for easy reference. The readers are encouraged to review the references for QA of the radiation safety survey and radioactivity assay instruments (3,4,5).
GAMMA CAMERA UNIFORMITY TEST
The intrinsic uniformity test is the most sensitive test to assure that the gamma camera is working properly. When exposed to a uniform source of radioactivity, the gamma camera should produce an image with uniform count density throughout the useful field of view. Due to the instability of photomultiplier tubes, variation in light production, and transmission in different crystal regions, gamma camera image nonuniformities may occur. Hot or cold spots in the field of view not only create a false impression of abnormal uptakes in the clinical images, but non-uniformity also causes linearity distortions, loss of resolution, and ring artifacts in SPECT images (6). One may simulate a uniform source of radioactivity or “flood” source by placing a small amount of radioactivity in a syringe and place it at a distance at least five times greater than the camera’s useful field of view. For a typical gamma camera with a field of view of 50 × 40 cm, the point source must be 250 cm or farther away from the detector surface (7). An image is then acquired in a 256 × 256 or 512 × 512 matrix with the collimator removed. Field uniformity tests performed without the collimator are know as the intrinsic flood uniformity tests.
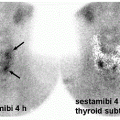
The gamma camera usually has a built-in software to measure integral and differential uniformities as indices of the field uniformity. A well-performing gamma camera should have values of integral and differential uniformities measuring <2.5%. However, gamma cameras having integral and differential uniformity <2.5% do not guarantee images free of artifacts. Careful inspection visually for any subtle hot or cold spots should always be performed. Linearity distortions in both the vertical and horizontal directions are shown in Figure 18.1, even though its integral and differential uniformities are <2.5%. Figure 18.2 shows a severe ring artifact in the SPECT image produced by a gamma camera whose integral and differential uniformity values met the manufacturer specifications; the ring artifact was caused by a small nonuniform spot in the location corresponding to the bull’s-eye of the ring.
Another test for gamma camera uniformity is called the extrinsic uniformity test. It is done by placing a sealed sheet of Co-57 directly on the collimator. Co-57 (t1/2 = 271.8 d) sheet sources are commercially available with 10, 15, or 20 mCi of Co-57 activity uniformity distributed better than 1% (8). The extrinsic uniformity test is not as sensitive as the intrinsic uniformity test for assessing the uniform response across the field of view of the gamma camera but is convenient to do daily and detects defects in the collimator. Most radioactive material licenses allow daily extrinsic uniformity test for its expediency, but a weekly intrinsic uniformity test has to be done to meet the QA test requirement. On annual basis, an extrinsic uniformity image is acquired using a 128 × 128 matrix for 120 million counts and stored on the computer for correction of subtle hot or cold spots in the projection images of a SPECT study. Such a high-count extrinsic uniformity image is called the uniformity correction matrix to correct for collimator defects and the nonuniform response of the sodium iodide and photomultiplier tube assembly.
RESOLUTION AND LINEARITY
The radioactive material license in some states requires that a resolution and linearity test be done at least once a week. The test is done by placing a four-quadrant bar phantom (aka a quad phantom) in direct contact with the crystal surface after the intrinsic flood test. A quad phantom is a rectangular plate with rows of lead bars in each quadrant. The spacing of the parallel lead bars varies from 2.0 to 3.5 mm at 0.5 mm increment. A static image is then acquired into a 512 × 512 matrix for 5 million counts. The image should clearly show the lead bars spaced at 2.5 mm apart and appeared straight visually. Because of the difficulty in mounting the heavy quad phantom on the bare surface of the gamma camera, many users simply put the quad phantom on the collimator and then a Co-57 flood source on top of the quad phantom to acquire the image. In the author’s opinion, the quad phantom test is not a sensitive test of the system’s resolution and linearity. The system has to have badly deteriorated before an abnormal pattern is shown in the quad phantom image. The resolution and linearity of a gamma camera are strongly affected by its uniformity. Greater attention should be paid to the intrinsic uniformity test, and the SPECT system performance test to be described.
Center of rotation
The center of rotation (COR) is the center pixel in the computer image matrix corresponding to the mechanical axis of detector rotation. Gamma camera heads with the collimator on are heavy and can shift slightly on the mechanical support during rotation. Even a 1-pixel shift can produce an objectionable bull’s-eye artifact in the center of the reconstructed image. The COR test measures the central pixel shift relative to the image matrix for each projection angle and makes the correction during image reconstruction. Shift correction is required to avoid bull’s-eye artifacts in the center of a SPECT image. Latest generation gamma cameras are manufactured with great care to assure mechanical stability so users may perform the COR test once a month using the manufacturer-provided apparatus and software.
SPECT system performance evaluation
The filtered backprojection algorithm commonly used for image reconstruction is a noise amplification procedure. A slight shift in any number of variables can produce noticeable artifacts in a SPECT study. A SPECT phantom test is recommended at acceptance, and at least annually (9).
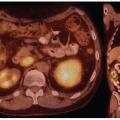
Figure 18.3 shows a typical SPECT three-section phantom. This includes a uniform activity section, a section with groups of plastic rods, and a section with spheres of different sizes and activities. The plastic rods section contains rods from about 5 to 13 mm in diameter. The spheres vary in diameter from 10 to 32 mm. Visual analysis of SPECT resolution is determined by the minimum size rods detectable in the reconstructed image. The ratio of counts per pixel in the spheres to counts per pixel in the surrounding water determines SPECT contrast. Visual assessment for SPECT uniformity is performed in the uniform activity section of the phantom, where the observer evaluates the evenness of count density and the absence of ring artifacts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree