Radiation Doses and Radiation Protection
Alfred Pfeiffer
Cyrill Burger
Positron emission tomography (PET), single-photon emission computed tomography (SPECT), and computed tomography (CT) use ionizing radiation, and therefore when these examinations are used, the ALARA principle (radiation dose As Low As Reasonably Achievable) must be observed. Even though there is no legal limitation to the radiation dose given for diagnostic or therapeutic purposes, one should try to minimize patient radiation exposure in PET, SPECT, and CT. A guideline to improve the management of patient doses in medical imaging is the DRL (diagnostic reference level) concept.
A fluorodeoxyglucose (FDG)-PET scan with 370 MBq (10 mCi) of 18F-FDG delivers a radiation dose of approximately 11 mSv to a patient, which is comparable to that from a diagnostic CT, which is in the range of 10 to 20 mSv. This radiation dose is predominantly due to the β+ particles (positrons) emitted from PET isotopes and not from the 511-keV γ-rays resulting from the annihilation process. With shorter-lived PET radioisotopes, radiation exposure is substantially lower, and higher or multiple doses can be given safely, as frequently is the case in water or ammonia studies.
Doses of SPECT examinations are typically much lower because technetium-99m, the most widely used radioisotope in SPECT imaging, exclusively emits γ-rays. It is state of the art to use short-lived and pure γ-emitters. This is different when other isotopes with much longer effective half-lives and/or additional β-ray emission are used.
Therefore, attenuation correction of PET and SPECT data by using radioactive line or point sources in a conventional PET or SPECT scanner does not add much to this dose. Adding CT for attenuation correction and anatomic coregistration conversely results in an additional dose. This dose depends on the quality of the CT scan and the protocol used (unenhanced vs. contrast enhanced, etc.). A low-dose CT with 40 mA, which we believe to yield adequate image quality for most PET-CT and SPECT-CT applications, results in a radiation burden of approximately 2 to 8 mSv. Thus an integrated PET-CT or SPECT-CT examination results in a typical dose of between 10 and 20 mSv and is therefore comparable to a contrast-enhanced CT. The “CTs” (e.g., GE Hawkeye) used for attenuation in SPECT-CT use a much lower tube current (typically 2 mA), and the radiation burden added to SPECT in SPECT-CT thus is in the range of 0.5 mSv, which is negligible.
Introduction
Nuclear medicine examinations deliver a certain amount of radiation to the patient as well as to the personnel involved with the patient before, during, and after the examination. In most countries, laws impose limits for the radiation burden of the personnel. The radiation dose that can be delivered to the patient is generally not restricted but recommended by the DRL.
Patient Radiation Dose
Generally the dose absorbed by the patient for any radiopharmaceutical depends on several factors:
type of decay
radiation energy
radionuclide half-life (physical half-life)
clearance from the body (biologic half-life)
kinetics of distribution in the body
As discussed in Chapter 2, the physical half-life Tphys and the biological half-life Tbiol together yield the effective half-life Teff, which is the relevant parameter for the radiation dose received by the patient:
A brief mathematical analysis shows that Teff is close to the shorter of the two times Tphys and Tbiol if the other one is much longer. Thus, for the short-lived positron-emitting nuclides oxygen 15 (15O) (Tphys = 2.04 minutes) and nitrogen 13 (13N) (Tphys = 9.97 minutes), the clearance from the body is of minor relevance. It becomes more important in the longer-lived nuclides such as fluorine-18 (18F) (Tphys = 109.775 minutes), iodine 124 (124I) (Tphys = 4.18 days), and the various “conventional” radiopharmaceuticals marked with technetium 99m (99mTc)(Tphys = 6.02 hours) or other nuclides emitting single photons.
The radiation dose in nuclear medicine and positron emission tomography (PET) is importantly influenced by the biologic nature of the radiopharmaceutical used. The result is a much wider range of organ doses received in a specific examination than in a computed tomography (CT) examination, in which the absorbed dose is in essence proportional to the absorption coefficient of the irradiated tissue. The calculation of single-organ doses (measured in grays; 1 Gy = 1 J/kg) and the whole-body effective dose (measured in sieverts; 1 Sv = 1 J/kg multiplied by a weighting factor for the biologic effectiveness of different decay types) is sophisticated and based on complex calculation models, which take the uptake values for different organs and the spatial neighborhood of the organs into account.
Table 9.1 Target Organ Doses of PET and SPECT Tracers | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
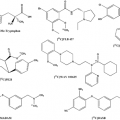
PET Tracers
It is important to note that the major radiation dose in PET comes from the positron and not from the γ-rays produced in the annihilation reaction. The most widely used radiopharmaceutical in clinical PET imaging is 18FDG. Physiologically, it is taken up by the brain and, depending on the fasting state, by the myocardium. It is excreted via the kidneys into the bladder. Thus the organs with the greatest radiation exposure in 18F-FDG studies are the brain, the myocardial wall, the kidneys, and the bladder wall (Table 9.1) (1,2,3). These single-organ doses are weighted for the calculation of the effective whole-body dose. From Table 9.1, we conclude that for a standard dose of FDG of 400 MBq the whole-body effective dose is approximately 8 mSv, which is comparable to the dose received when being examined by full-dose CT. Also note that the radiation exposure with ammonia and water is much smaller because of the shorter half-lives of these compounds (4). The clinical use of long-lived radionuclides such as 124I (physical half-life 4.2 days) is only acceptable if they are bound to a radiopharmaceutical with short biologic half-life.
SPECT Tracers
The patient radiation exposure from single-photon emission tomography (SPECT) tracers varies over a wide range.
Radionuclides with an advantageous combination of γ-ray energy and effective half-lives such as 99mTc in general deliver lower doses to the patient than do long-lived nuclides with a low energy such as thallium 201 (201Tl). Table 9.1 summarizes the radiation exposures arising from intravenous application of some frequently used SPECT radiopharmaceuticals in comparison to PET tracers.
Radionuclides with an advantageous combination of γ-ray energy and effective half-lives such as 99mTc in general deliver lower doses to the patient than do long-lived nuclides with a low energy such as thallium 201 (201Tl). Table 9.1 summarizes the radiation exposures arising from intravenous application of some frequently used SPECT radiopharmaceuticals in comparison to PET tracers.
Transmission Computed Tomography Dosimetry
Dedicated PET scanners without a CT unit use positronemitting sources such as germanium 68 (68Ge) and gallium-68 (68Ga) for transmission scans, which are crucial for the reconstruction of quantitative PET images. The patient’s radiation exposure caused by these transmission scans is about 2 or 3 orders of magnitude below the effective dose resulting from the administration of radiopharmaceuticals and is therefore negligible (5,6). As stated earlier, this is because the photon flux of the line sources used for the transmission scan in PET is very low, and the radiation burden in PET examinations is dominated by the positron radiation. However, with use of a CT scan for transmission correction and for anatomic localization of suggestive lesions, the radiation dose becomes relevant because of the much higher photon flux used in CT and the lower energy of the x-rays used compared with the γ-rays. The radiation dose stemming from the CT portion of PET-CT or SPECT-CT scans must therefore be taken into account.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree