MR imaging is nowadays regarded as the preferred imaging modality for evaluation of soft tissue lesions. As plain radiographs are often the first step in evaluation of musculoskeletal disorders, identification of subtle soft tissue signs may be helpful to select patients who need to be referred for subsequent MR imaging. Although not very sensitive, certain plain film findings, such as intralesional calcification or gas, may allow one to make to a more specific tissue diagnosis and may obviate the need for invasive diagnostic procedures and potential harmful treatment.
Key points
- •
Plain films have a low sensitivity in the diagnosis of soft tissue tumors or tumor-like conditions, but the presence of intralesional soft tissue calcification may be useful for tissue specific diagnosis.
- •
Mineralization in myositis ossificans follows a time-dependent centripetal pattern from the periphery toward the center. The mineralization pattern in extraskeletal osteosarcoma (ESO) is more amorphous and occurs from the center to the periphery.
- •
MR imaging and histology may simulate ESO in the early stage of myositis ossificans. Biopsy should be avoided in the early stage of myositis ossificans.
- •
The use of fat suppression may decrease conspicuity of accessory muscles.
- •
The presence of intralesional air may enhance the specificity of gas-forming infection and of necrotizing soft tissue infections.
Introduction
Because of its high soft tissue contrast and exquisite anatomic resolution, MR imaging is regarded as the imaging modality of choice for evaluation of musculoskeletal soft tissue lesions.
However, most of these abnormalities may be suspected on conventional radiography (CR) by analysis of subtle or indirect signs. These signs are well recognized by experienced radiologists, but are less known and often forgotten by young colleagues who are currently well trained in interpretation of MR imaging. As CR remains often the initial imaging tool in the evaluation of many musculoskeletal disorders, it is important to remember these signs as potential markers of relevant soft tissue pathology. Correct identification and interpretation of soft tissue signs on CR may be helpful to select patients who need to be referred for further MR imaging. On the other hand, in certain scenarios, meticulous analysis of plain film findings may even lead to a more specific tissue diagnosis of soft tissue abnormalities, such as demonstration of phleboliths in slow-flow vascular malformation or the presence of peripheral calcifications in myositis ossificans.
Therefore, correlation of MR imaging findings and radiographic findings is highly recommended, as the information derived from both imaging techniques is often complementary.
The aim of this article is to remind readers of the most valuable signs that may suggest the presence of soft tissue pathology on CR and to discuss their diagnostic strength compared with MR imaging findings.
Discussion of musculoskeletal soft tissue diseases on plain films will be done along with the radiographic density of its major macroscopic components ( Table 1 ).
| Grayscale | Soft Tissue Component |
|---|---|
| Black | Air |
| Dark gray | Fat |
| Light gray | Water and most other soft tissue |
| White (moderate) | Calcification, ossification |
| White (marked) | Metal, iron |
Lesions containing soft tissue mineralization
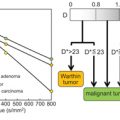
Mineralization in the soft tissues may occur in a large spectrum of disorders including congenital, metabolic, endocrine, traumatic, and parasitic infections. Mineralization is often far better identified on plain films or computed tomography (CT) than on MR imaging. In addition, meticulous analysis of the pattern of intralesional calcification or ossification may be helpful for a more tissue-specific diagnosis of a soft tissue lesion.
Basic Calcium Phosphate Crystal Deposition Disease
Basic calcium phosphate (BCP) crystal deposition disease consists of BCP crystal deposition in either periarticular soft tissues or less frequently the joints. It is also designated as hydroxyapatite deposition disease (HADD), as the deposits are predominantly composed of hydroxyapatite and less commonly of tricalcium phosphate and octacalcium phosphate.
Calcific tendinopathy of the shoulder tendons is the most common manifestation, accounting for 60% of cases, followed by involvement of the tendons of the hip, knee, elbow, wrist, and hand. Virtually any tendon can be involved. Other periarticular tissues such as bursae ( Fig. 1 ), capsule, and ligaments may be also involved. The disease can be divided in a precalcific, calcific, and postcalcific stages, of which the calcific stage is further subdivided into formative, resting, and resorptive phases.

In the formative and resting phases, dense, homogeneous and well-defined calcium deposits are seen on plain radiographs. Calcifications in the formative and resting stages are often more difficult to characterize on MR imaging, because of the low contrast with surrounding tendons.
Patients are often asymptomatic at these stages or may present with only a mild discomfort. On the contrary, acute pain typically accompanies the resorptive phase, in which deposits migrate in surrounding tissues, bursae, joints, or even bones. On radiographs, the calcification becomes fluffy, ill-defined, and less dense, or may even become invisible. Associated bone erosions, bone marrow edema on MR imaging, intraosseous migration, or increased uptake on nuclear medicine studies may mimic a tumor or infection. The clue to the correct diagnosis is the location of the lesion at its specific tendon insertion at the bone and correlation of MR imaging with the presence of calcification on plain radiographs. A targeted CT scan may be useful to demonstrate minute calcifications and bone erosions in complex anatomic areas such as the pelvis ( Fig. 2 ).

Symptomatic BCP in the capsule and ligaments may be associated with adjacent bone marrow and soft tissue edema on MR imaging, whereas the underlying calcification is better seen on corresponding radiographs ( Fig. 3 ).

Calcific tendinopathy of the longus colli is a specific spinal manifestation of BCP disease and may clinically and on MR imaging mimic a retropharyngeal abscess. The identification of calcifications in the longus colli underneath the anterior arc of C1 is the clue to the correct diagnosis ( Fig. 4 ).

Calcium Pyrophosphate Dihydrate Crystal Deposition
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease refers to deposition of CPPD in hyaline cartilages and fibrocartilage of the joints (menisci, acetabular labrum, pubic symphysis, and intervertebral discs), but also in other soft tissue such as ligaments, capsules, and tendons. Both articular and periarticular deposition may be complicated by subsequent inflammation and may result in CPPD arthropathy or painful tophaceous pseudogout of the soft tissues, respectively. In the soft tissues, radiographs show a more linear and/or stratified appearance compared with BCP (HADD), and it should be noted that CPPD crystal deposition occurs in an older population. Overall, the use of MR imaging for evaluation of CPPD of the soft tissues is disappointing or may mimic other soft tissue lesions. On MR imaging, CPPD deposits are of low signal on all pulse sequences. Like other calcifications, they are often difficult to detect and characterize on MR imaging. Gradient-echo sequences may enhance their conspicuity. As meniscal chondrocalcinosis can mimic a meniscal tear, correlation of radiographs with all MR imaging is important to avoid overdiagnosis ( Fig. 5 ).

Calcifications involving the transverse ligament and adjacent to the odontoid process, designated as the crowned dens syndrome, comprise a spinal manifestation of CPPD. Calcifications are often an incidental finding on imaging, but they may be associated with fever, neck pain, and stiffness, and may even mimic meningitis clinically.
Traction Fibro-Osteosis at the Insertion of Tendons at the Bones
Bone production at the insertion of tendons at the bones is common at different locations, and is generally found incidentally on imaging. It is readily detected on plain films but is often more difficult to detect on corresponding MR imaging unless it is accompanied by surrounding inflammation or if contains fatty bone marrow ( Fig. 6 ).

Collagen Vascular Disease
Soft tissue calcifications are also a typical manifestation in collagen vascular disorders such as progressive systemic sclerosis, systemic lupus erythematosus, dermatomyositis, and polymyositis. Calcifications associated with progressive systemic sclerosis involve the hands and wrists. In systemic lupus erythematosus (SLE), they are preferentially located in the lower extremity, whereas calcifications in polymyositis and dermatomyositis typically affect the fasciae and subcutaneous tissues.
Scleroderma-associated calcinosis is usually seen in the finger tips and around the synovial joints of the hands, knees, and elbows.
Patients with scleroderma may present with 1 or more components of the CREST (calcinosis- Raynaud – esophageal dysfunction – sclerodactyly- teleangiectases) syndrome.
Mixed connective tissue disease consists of a combination of SLE, scleroderma, and polymyositis. On MR imaging, calcified lesions are of low signal intensity, both on T1- as on T2-weighted images, and show no contrast uptake after administration of gadolinium contrast ( Fig. 7 ). Active inflammation may be of high signal intensity on fluid-sensitive sequences.

Osteochondromatosis
Synovial osteochondromatosis (SC) is characterized by the formation of numerous metaplastic cartilaginous or osteocartilaginous nodules of small size, within the joint, tendon sheath, or bursa. Synovial osteochondromatosis commonly occurs in large joints, but virtually any joint may be involved.
Primary SC ( Fig. 8 ) is defined by cartilaginous metaplasia, synovial hyperplasia, and production of round cartilaginous nodules of similar size. The joint space is spared or may be even enlarged because of pressure erosion. This occurs preferentially in joints with a tense capsule, such as the hip joint.

Secondary SC ( Fig. 9 ) is part of degenerative joint disease, arthritis, or trauma, resulting in dislodgement of bony or cartilaginous tissue undergoing concentric layering. The nodules are more irregular, often larger and of heterogeneous size compared with nodules of the primary form. The joint space is narrowed. Milgram proposed the following staging system. In the initial stage, there is active synovial disease without loose bodies. The transitional stage is characterized by persistent synovial disease and formation of loose bodies, whereas in the third stage, detached intra-articular nodules are present, with burned-out intrasynovial disease. Approximately two-thirds of nodules calcify or ossify.

Plain radiographs are normal in the initial stage, whereas MR imaging shows increased amount of joint fluid and nonspecific synovitis (see Fig. 9 ). Uncalcified nodules are also invisible on plain radiographs in the transitional stage, and are isointense to muscle on T1-weighted images and hypointense to synovial fluid on T2-weighted images (see Fig. 9 ). Calcified lesions are seen as small, round signal voids. Finally, ossified nodules may demonstrate signal intensities of fatty bone marrow. Plain radiography and CT demonstrate calcified or ossified nodules ( Fig. 10 , Table 2 ).

| Stage | Radiographs | T1-Weighted Imaging | T2-Weighted Imaging |
|---|---|---|---|
| Early | Normal | Hypointense joint fluid | Hyperintense increased joint fluid |
| Intermediate | Normal | Nodules isointense with muscle | Nodules of high signal |
| Late-stage calcified nodules | Calcified nodules | Low signal nodules | Low signal nodules |
| Late-stage ossified nodules | Ossified nodules with concentric rings | Ringlike nodules containing central fat | Ringlike nodules containing alternating fat and cartilage |
Myositis Ossificans
Myositis ossificans is a benign, solitary, frequently self-limiting, ossifying soft-tissue mass encountered often in young patients and related to trauma in more than half of the cases.
The lesion has a typical zonal organization on histology and imaging.
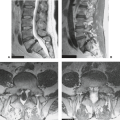
Three time-dependent stages have been described: early, intermediate, and mature. There may be some overlap between these stages. In the early stage (up to 4 weeks), faint peripheral calcifications may appear at earliest 2 weeks of presentation on ultrasound or CT and soon after on plain radiographs. The signal intensity on MR imaging is nonspecific, and the lesion may enhance, simulating a soft tissue sarcoma. Biopsy should be avoided in this stage, as histologic findings may show a high mitotic activity, hyperchromatic myofibroblastic cells, and osteoid matrix, simulating an extraskeletal osteosarcoma (ESO). After 4 weeks to 8 weeks (intermediate stage), a well-defined peripheral calcification with central lucency or hypodensity becomes more apparent on plain radiographs and CT, respectively. MR imaging shows a rim of low SI on all pulse sequences, corresponding to calcifications, but generally calcifications are less conspicuous on MR imaging. There is perilesional edema that gradually disappears after 4 weeks. In the mature stage starting at 8 weeks until 6 to 12 months, calcifications are gradually replaced by ossification, with no residual central lucency on plain radiographs. The calcification-ossification front further develops following a centripetal pattern, with lamellar bone at the periphery proceeding toward the center ( Figs. 11 and 12 ). This centripetal pattern is important in the differential diagnosis with ESO, in which the lesion calcifies from the center to the periphery. MR imaging demonstrates low signal intensity on all sequences in mature lamellar bone with hyperintense areas on T1-weighted images, corresponding to fatty bone marrow formation between the bone trabeculae. The perilesional edema is absent in this stage. Between months 6 and 12, the lesion may spontaneously regress slightly or completely and appear smaller on repeated radiographs (see Fig. 11 ).


Florid reactive periostitis and soft tissue aneurysmal bone cysts are lesions that are closely related to myositis ossificans. Florid reactive periostitis is attached to the underlying cortex, whereas myositis is usually separated from the cortex. Soft tissue ABC contains fluid-fluid levels on MR imaging.
Calcific Myonecrosis
Calcific myonecrosis is an uncommon late sequela of trauma, with a reported delay ranging from 10 to 64 years after an initial traumatic event. It typically affects the lower extremities in the anterior and lateral compartments of the leg. More rarely, the foot and upper extremities are involved.
Plain radiographs show a fusiform mass along with the long axis of the muscles with peripheral calcifications, with a typical linear plate- or plaque-like configuration.
On MR imaging, the periphery of the lesion is of low intensity on T1-weighted images, corresponding to abundant calcification ( Fig. 13 ). T1- and T2-weighted images may demonstrate lesion heterogeneity caused by repeated intralesional hemorrhage with accumulation of blood products, liquefaction necrosis, and calcified areas. The lesion does not enhance, unless there is superimposed inflammation, often caused by mobilization of plaque and penetration through the muscle fascia.