Radiologic Evaluation of Metabolic and Endocrine Disorders
Composition and Production of Bone
Bone tissue consists of two types of material: (a) an extracellular material, which includes organic matrix or osteoid tissue (collagen fibrils within a mucopolysaccharide ground substance) and an inorganic crystalline component (calcium phosphate or hydroxyapatite); and (b) a cellular material, which includes osteoblasts (cells that induce bone formation), osteoclasts (cells that induce bone resorption), and osteocytes (inactive cells).
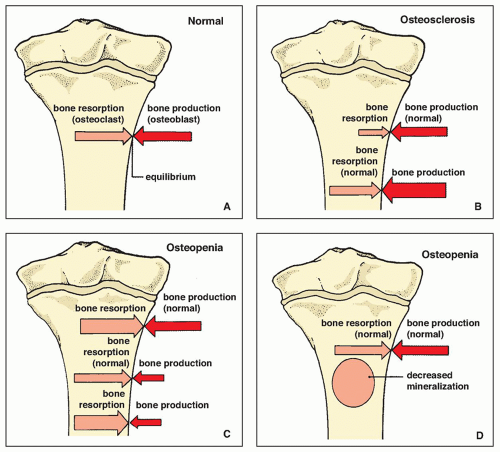
Bone is a living, dynamic tissue. Old bone is constantly being removed and replaced with new bone. Normally, this continuous process of bone resorption and formation is in balance (Fig. 26.1A), and the mineral content of the bones remains relatively constant. In some abnormal circumstances, however, when the metabolism of the bone is disturbed, this balance may be upset. If, for example, osteoblasts are more active than usual, or if osteoclasts are less active, more bone is produced (a state known as too much bone) (Fig. 26.1B). If, however, osteoclasts are normal or overactive and osteoblasts underactive, then less bone is produced (“too little bone”) (Fig. 26.1C). A generalized reduction in bone mass may also be caused by decreased mineralization of osteoid, with equilibrium in the rate of bone resorption and production (Fig. 26.1D).
The growth and mineralization of bone are influenced by a variety of factors, the most important of which are the levels of growth hormone produced by the pituitary gland, of calcitonin produced by the thyroid gland, and of parathormone produced by the parathyroid glands, along with the dietary intake, intestinal absorption, and urinary excretion of vitamin D, calcium, and phosphorus.
It should be remembered, however, that normal bone density changes with age, increasing from infancy until age 35 to 40 years, and then progressively decreasing at the rate of 8% per decade in women and 3% in men.
Evaluation of Metabolic and Endocrine Disorders
Most metabolic and endocrine disorders are characterized radiographically by abnormalities in bone density that are generally related to increased bone production, increased bone resorption, or inadequate bone mineralization. The bones affected by these conditions appear abnormally radiolucent (osteopenia) or abnormally radiodense (osteosclerosis) (Table 26.1).
Radiologic Imaging Modalities
The radiologic modalities most often used to evaluate metabolic and endocrine bone disorders are:
Conventional radiography
Computed tomography (CT)
Radionuclide imaging (scintigraphy, bone scan)
Magnetic resonance imaging (MRI)
Ultrasound (US).
Conventional Radiography
Radiography is the simplest and most widely used method of evaluating bone density. This technique can easily detect even very small increases in bone density; however, it generally fails to detect decreases in overall skeletal mineralization unless the reduction reaches at least 30%. It must be pointed out that normal bone can easily acquire an abnormal radiographic appearance as a result of technical errors, such as improper settings for kilovoltage and milliamperage. Overexposure, for instance, creates the appearance of increased bone radiolucency, whereas underexposure creates an artificially increased bone radiodensity.
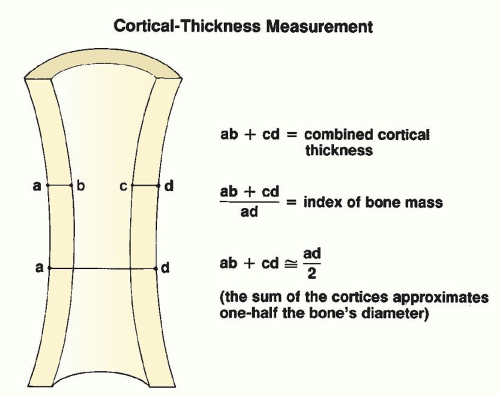
For these reasons, inspection of a standard radiograph should focus less on apparent increases or decreases in bone density but more on the thickness of the bone cortex. Cortical thickness is directly correlated with skeletal mineralization; it can be objectively measured and compared either with a normal standard or with subsequent studies in the same patient. The cortical thickness measurement is obtained by adding the width of the two cortices in the midpoint of a given bone, a sum that should be approximately one half of the overall diameter of the bone; it may also be expressed as an index of bony mass, derived by dividing the combined cortical thickness by the total diameter of the bone (Fig. 26.2). The second or third metacarpal bone is commonly used to obtain these measurements (Fig. 26.3).
A related method for assessing bone density that also uses radiography is the photodensitometry technique. This technique is based on the observation that the photographic density of a bone on a radiographic film is proportional to its mass. Through the use of a photodensitometer, the photographic density of a given bone can be compared with that of known standard wedges, giving an accurate assessment of the degree of bone density.
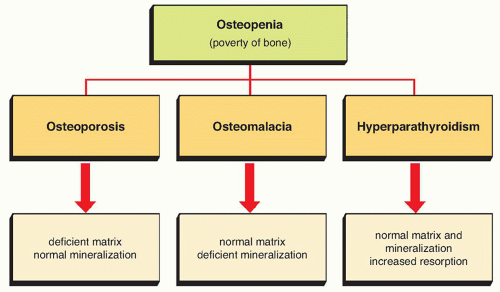
The appearance of relative increased bone radiolucency on standard radiographs should not be called osteoporosis because such a finding
is not specific for osteoporosis, osteomalacia, or hyperparathyroidism. Most authorities agree that increased radiolucency is best termed osteopenia (poverty of bone). Osteoporosis refers specifically to a reduction in the amount of bone tissue (deficient bone matrix) and osteomalacia refers to a reduction in the amount of mineral in the matrix (deficient mineralization); both conditions are characterized by increased bone radiolucency (Fig. 26.4). As Resnick has pointed out, any condition in which bone resorption exceeds bone formation results in osteopenia, regardless of the specific pathogenesis of the condition. In fact, diffuse osteopenia is found in osteoporosis, osteomalacia, hyperparathyroidism, neoplastic conditions such as multiple myeloma, and in a wide variety of other disorders.
is not specific for osteoporosis, osteomalacia, or hyperparathyroidism. Most authorities agree that increased radiolucency is best termed osteopenia (poverty of bone). Osteoporosis refers specifically to a reduction in the amount of bone tissue (deficient bone matrix) and osteomalacia refers to a reduction in the amount of mineral in the matrix (deficient mineralization); both conditions are characterized by increased bone radiolucency (Fig. 26.4). As Resnick has pointed out, any condition in which bone resorption exceeds bone formation results in osteopenia, regardless of the specific pathogenesis of the condition. In fact, diffuse osteopenia is found in osteoporosis, osteomalacia, hyperparathyroidism, neoplastic conditions such as multiple myeloma, and in a wide variety of other disorders.
TABLE 26.1 Metabolic and Endocrine Disorders Characterized by Abnormalities in Bone Density | ||||||
|---|---|---|---|---|---|---|
| ||||||
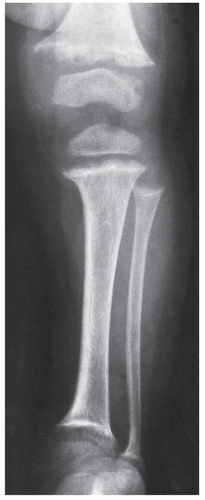
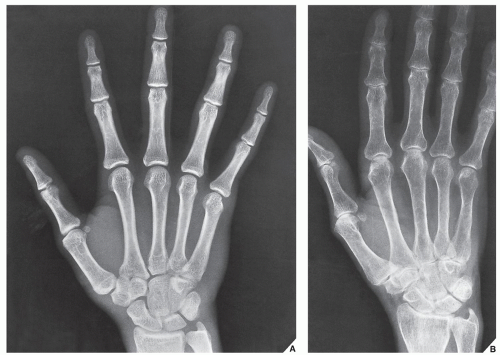 FIGURE 26.3 Cortical thickness of the hand. Dorsovolar radiographs of the hand show normal (A) and abnormal (B) thickness of the cortex of the second and third metacarpal bones. |
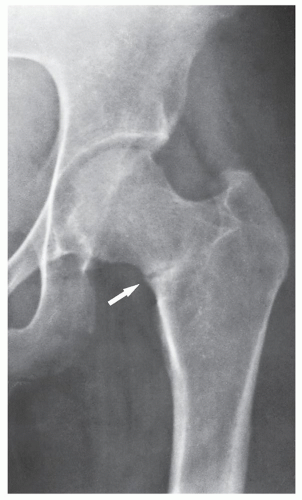
Although osteopenia is a nonspecific finding, radiography can help detect other important radiographic features leading to a specific diagnosis. Among these are Looser zones, representing pseudofractures or insufficiency-type stress fractures that are characteristic of osteomalacia (Fig. 26.5); widening of the growth plate and flaring of the metaphysis, which are typical findings in rickets (Fig. 26.6); subperiosteal bone resorption, an identifying feature of hyperparathyroidism (Fig. 26.7); and focal areas of osteolytic destruction and endosteal scalloping, which are characteristic of multiple myeloma (Fig. 26.8).
Magnification radiography was in the past useful in metabolic disorders for demonstrating the details of bone structure. The subperiosteal bone resorption characteristic of hyperparathyroidism, or cortical tunneling (Fig. 26.9), which may be seen in any process that causes increased bone resorption, was well delineated on magnification studies. Cortical tunneling occurs very early in a pathologic process and may be found even in the absence of other radiographic abnormalities. At the present time, magnification radiography is effectively replaced by more
sophisticated techniques, namely, digital radiography and picture archive and communication system (PACS), allowing filmless high-resolution image-display format with advanced reading workstations, already discussed in Chapter 12.
sophisticated techniques, namely, digital radiography and picture archive and communication system (PACS), allowing filmless high-resolution image-display format with advanced reading workstations, already discussed in Chapter 12.
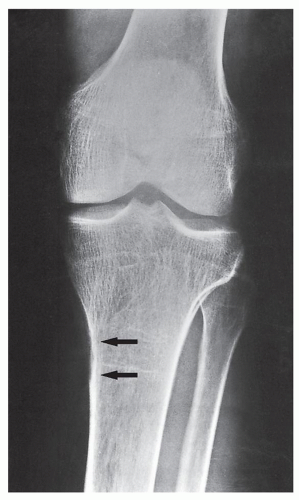 FIGURE 26.7 Hyperparathyroidism. Anteroposterior radiograph of the left knee of a 42-year-old woman with primary hyperparathyroidism caused by hyperplasia of the parathyroid glands demonstrates increased bone radiolucency and areas of subperiosteal bone resorption on the medial aspect of the proximal tibia (arrows), characteristic of the condition.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|