1.20: Radiology information system and picture archiving and communication systems
Devasenathipathy Kandasamy, Krithika Rangarajan
I learned that computer science is not just about syntax & coding. We can make a difference in people’s lives by developing applications.
Kyle Rector
Introduction
Imaging informatics is a subspecialty of radiology which deals with collection, management and delivery of healthcare information from one person or place to another. It covers every aspect of radiology departmental workflow. The workflow of the modern day radiology department has changed quite a lot compared to 2 decades back. Almost all the radiology equipment are digital and capable of transferring images over the network. There are many departments which are completely digital and hardcopies are not used anymore. This complete digital transformation provides a lot of flexibility and ease in day to day workflow. The Radiology Information System (RIS) and Picture Archiving and Communication System (PACS) forms the backbone of the digital infrastructure of any radiology department. RIS orchestrates the entire workflow inside the radiology department communicating with all the scanner and PACS. It also handles the worklists and reports. PACS handles the storage, receiving and sending of radiology images. The Hospital Information System (HIS) handles the data from the entire hospital which are mostly text data. If a hospital has HIS, it orchestrates the entire hospital workflow such as electronic medical records, lab data, etc. HIS initiates the radiology workflow as well such as clinician ordering a study, which will be communicated with RIS. Beyond this step RIS takes over the process and handles the workflow (scheduling, worklist creation, reporting, etc.) inside the radiology department. Each step is communicated with HIS and reports are sent back to HIS completing the workflow. The concept of PACS originated in the 1980s and since then there has been explosive growth all over the globe. Introduction of PACS created a seamless workflow and dramatically reduced the turnaround time and improved the patient care. There are multiple benefits of RIS-PACS such as clinicians can order a procedure online, images are available immediately after acquisition to the radiologists irrespective of their geographical location, more than one radiologists can look at a particular case and there is no issue of manually organizing the hard copies and lost films or reports. The images and reports are securely stored and transmitted which can be accessed only with appropriate credentials. All actions by the user can be tracked and monitored. The basics of RIS, PACS, modalities, storage devices and display devices will be discussed in this chapter.
Industry standards
Before any industry standard came into existence, every vendor had their own proprietary image format which was not compatible with the other vendors. This was a major obstacle to sharing images or text data over the network. To facilitate easy flow of information across the network regardless of the vendors, industry standards such as health Level 7 (HL7) and Digital Imaging and Communications in Medicine (DICOM) were developed over the years. Currently, all the major vendors comply with this standard so that the information is shared across the network and devices without any compatibility issue.
DICOM
DICOM stands for Digital Imaging and COmmunications in Medicine. It is an international standard for medical images and other related digital data. American College of Radiology (ACR) and National Electrical Manufacturers Association (NEMA) came together and developed this standard image format. It includes medical image formats for storage, as well as protocols for various communication services that may need to be used for the work-flow.
This was aimed to overcome the issue of proprietary image formats and propose a common standard which all manufacturers would follow. It has thus become the standard across medical imaging platforms including not only acquisition devices but also the work-stations, archives, servers, printers, etc. All devices that implement DICOM standards are called DICOM compliant devices, and these are usually connected through a DICOM network. Each such DICOM device is a DICOM node or DICOM peer. Each DICOM compliant device implements certain services. These services are detailed by each vendor who is required to provide a “DICOM Conformance Statement” along with the device. The first version was released in 1983 and the latest version which is DICOM 3.0 was released in 1993.
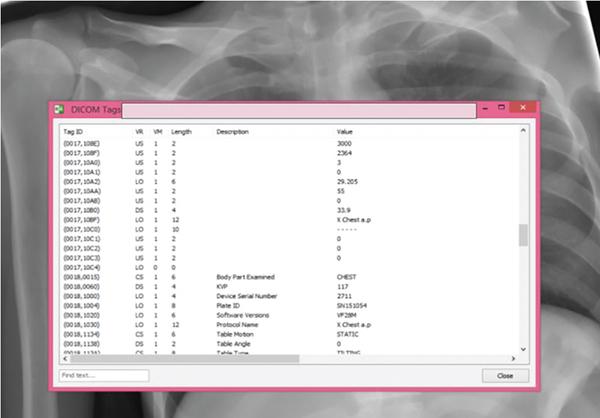
In order to understand how images are queried through PACS, it is important to understand some aspects of a DICOM image. A DICOM file has some header information which contains patient metadata, and it contains image information. For example, DICOM tags associated with the chest X-ray from a patient is shown in the image below (Fig. 1.20.1). This includes View information, information about the acquisition device, as well as patient-related information. The meta-data stored in the DICOM file can be accessed separately, in order to search for the patients with attributes matching a certain search criteria.
HL7
Similar to the DICOM standard which was developed for radiological images, HL7 was developed to standardize the text information flow across networks and devices. It was introduced in 1987 and it uses the application layer in open systems interconnection (OSI). Hence, it is independent of the lower layers such as the hardware and various other variables. According to HL7 format text information would be exchanged as HL7 messages. Any event such as admission, discharge or transfer will be communicated to other devices through HL7 messages. RIS following the HL7 standard will parse the messages from HIS and updates its database.
Integrating the healthcare enterprise
Industry standards such as DICOM and HL7 were developed to make sure there is interoperability among various modalities and devices in the radiology department which sounds good in theory. However, in reality there can be many issues when different vendors are implementing HIS, RIS and PACS. In this kind of heterogeneous environment there can be multiple interoperability issues arising due to ambiguities in interpretations and implementations of DICOM and HL7. Also there can be issues which are not solved by either of the existing standards. This is where IHE comes into play by ironing out the issues arising because of variations in vendor implementations. It is a framework which has been developed by healthcare professionals and industry to promote collaboration among various vendors. There are multiple implementation profiles such as scheduling, reconciliation of data, etc., defined by IHE for various steps involved in radiology workflow. Vendors can declare their conformance for various IHE-defined profiles. Also, IHE organizes an annual event called connectathon where various vendors can participate and demonstrate their IHE profile conformance and their capability to interoperate. This provides a unique opportunity for peer–peer testing of their products and ironing out the issues before implementing it in customer’s place. The reports of these testing processes are available on IHE website which can be used to check any vendor’s compatibility with another for any available profile.
Image acquisition devices
Image acquisition devices or modalities are the originating points of all the images. Any device or scanner such as Digital radiography (DR), computed radiography (CR), CT, MRI, USG, etc., which can generate digital images in DICOM format can be integrated into the network so that the images can be transmitted to various devices. Even the film digitizers which convert films into DICOM images are considered as a modality. Once RIS receives HL7 messages from HIS for a new study, RIS schedules the study and prepares a worklist which is transmitted to the modality. Study is performed by the modality using the demographic details presented by RIS without any manual input by the user which greatly reduces the typographical errors. Modality sends a message to RIS once the study is completed and the corresponding images are sent to PACS for storing it in an organized manner. RIS also checks with the PACS about the proper storage of those images and updates its own database. In this way all the devices including the modalities work in an organized manner to make sure that all the acquired data are stored properly.
Basic PACS components
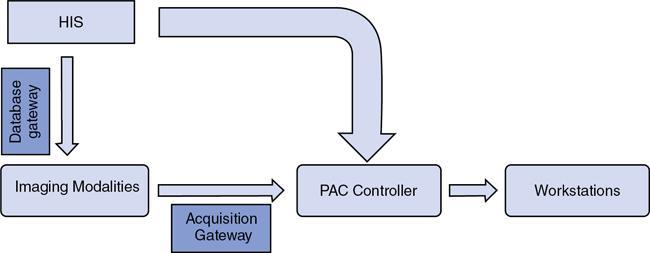
With complete digitization of healthcare, hospitals have moved to the use of Hospital Information Systems (HIS) to manage scheduling, and management of patients. HIS contains many databases; this includes various clinical information databases, and one of these is the Radiology Information System (RIS). The HIS collects information directly from the patient, including the demographic data, and communicates with several sub-systems to collect lab test results, information from radiology reports, and distributes these strategically to facilitate hospital operation (Fig. 1.20.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree