52 Rectus Sheath Block
The rectus abdominis is a vertical muscle of the anterior abdominal wall. The muscle is divided into compartments by the midline linea alba, paramedian linea semilunaris, and transverse fibrous bands.1 Muscles of the lateral abdominal wall (the external oblique, internal oblique, and transversus abdominis) become aponeurotic as they approach the midline. The rectus sheath consists of the rectus abdominis muscles surrounded by these aponeuroses.
Above the arcuate line, the transversalis fascia and the aponeuroses separate the rectus abdominis muscle from the abdominal cavity. Caudal to the arcuate line, the rectus abdominis muscle is in direct contact with the transversalis fascia. In this location, all three of the lateral abdominal wall muscles (external oblique, internal oblique, and transversus) have their aponeuroses pass anterior to the rectus abdominis muscle.2
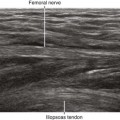
Anterior cutaneous branches of the intercostal nerves enter the rectus sheath from the posterior and lateral sides.3 Epigastric arteries and veins are sometimes identified within the rectus sheath. The anterior intercostal nerves can run alongside these vessels before rising to the surface through the rectus abdominis muscle. The nerves of the rectus sheath are too small to be directly imaged with ultrasound.
Rectus sheath block is useful as part of a combined anesthetic technique for outpatients.4,5 The usual indication for this block is to provide pain relief after repair of umbilical or incisional hernias. It provides an excellent alternative to straight general anesthesia or epidural blocks for surgical procedures around the midline of the abdominal wall.
Suggested Technique
Because of the compartmental nature of the rectus abdominis muscle, two or four injections are usually performed for periumbilical surgery (right and left sides, and sometimes above and below the umbilicus). About 5 to 10 mL of local anesthetic is injected per side per compartment in adult patients. Because the tendinous inscriptions of the muscles are not complete posteriorly,6 some communication between compartments is possible. If local anesthetic is observed to distribute between compartments, no further injection is necessary.
In one study, 21% of rectus sheath injections guided by traditional loss-of-resistance techniques were intraperitoneal.7 These intraperitoneal injections were detected by ultrasound imaging after initial needle placement. Although no complications were observed in this study, intraperitoneal injections are not clinically effective and presumably place patients at risk for injury.