Renal
The kidney and bladder are two of the most sonographically accessible organs. Both are easily recognizable to those who are new to ultrasound and thus the urinary tract can be a simple starting point for learning point-of-care sonography in the acute care setting.
The primary focus of renal ultrasonography in the emergency setting has been to determine the presence or absence of hydronephrosis.1–4 As with other areas of point-of-care ultrasound, physicians using the modality for this specific goal have begun to explore new indications for imaging the urinary tract. Ultrasound determination of bladder volume and evaluation of bladder filling before catheterization are two such examples.5–14 Another important consideration that has arisen with the focused use of renal ultrasound is the management of unexpected or incidental findings, such as masses and cysts.15–18
 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS
For many years, the standard imaging modality in cases of suspected renal colic was the intravenous pyelogram (IVP). Although IVP is more specific than ultrasound for the detection and characterization of a ureteral stone,19–23 it has several disadvantages in the emergency and acute care settings, which include the use of iodinated contrast material and exposure to ionizing radiation. Noncontrast spiral CT and ultrasound have largely replaced IVP as the preferred imaging studies for patients presenting to the ED with renal colic.24–26
The sensitivity of CT scan in the detection of renal stone disease varies from 86% to 100%.27–35 CT provides excellent visualization of the urinary tract and renal stones, and has a higher sensitivity for renal calculi compared with ultrasound.36 However, CT remains less accessible, involves a considerable exposure to radiation, and does not need to be performed emergently in stable patients with uncomplicated clinical presentations. Many physicians are now using CT in place of both ultrasound and IVP because it allows visualization of the urinary tract as well as extraurinary structures such as the appendix and aorta. A retrospective analysis of ED visits from 1996 to 2007 found a 10-fold increase in the use of CT in patients with suspected renal stone disease.37 However, there was no corresponding increase in the proportion of renal stone diagnoses or hospital admissions. Another study showed that in patients who had resolution of pain with analgesics, immediate imaging by CT in the ED did not lead to reduced morbidity when compared to imaging by CT 2–3 weeks later.38 The widespread use of CT has raised concerns within the imaging community because of the large cumulative radiation dosage being delivered to patients. The successive and repetitive nature of renal colic virtually assures these patients (especially younger ones) a higher iatrogenic cancer risk and, thus, forms a logical argument for judicious use of CT in this population.39,40
Ultrasound, however, can be performed safely and quickly at the bedside with essentially no risks. It is the modality of choice for patients in whom radiation should be avoided such as children and pregnant women. While ultrasound does not give information about renal function, the presence of unilateral hydronephrosis or hydroureter in the setting of hematuria and acute flank pain is very sensitive for the presence of a ureteral stone. Studies comparing point-of-care ultrasound with CT for the detection of hydronephrosis have found sensitivities comparable to comprehensive ultrasonography performed in the radiology suite.41–44
The degree of hydronephrosis, in combination with the patient’s history and response to analgesics, is helpful to determine the need for urgent consultation with a urologist. Studies have found a relationship between the degree of hydronephrosis on point-of-care ultrasound and ureteral stone size on CT.45 In this respect, point-of-care ultrasound often provides sufficient information to efficiently guide the treatment and disposition of the patient. Although a patient with mild-to-moderate hydronephrosis can, with few exceptions, be managed on an outpatient basis, the presence of severe hydronephrosis should prompt further definition of the obstruction by CT and urgent consultation or close follow-up.
In the course of utilizing ultrasound of the urinary tract to detect obstruction, practitioners are identifying other abnormalities with increasing frequency. Some of these represent life- or kidney-threatening processes and may prompt timely definitive treatment. Ultrasound is especially sensitive for the presence of cysts and for distinguishing between solid and cystic masses.46
Since the differential diagnosis in patients with flank or abdominal pain involves other organs visualized well by point-of-care ultrasound, invaluable additional information may be available. Specifically, if no hydronephrosis is seen on ultrasound examination, the physician may proceed to visualize the gallbladder, common bile duct, and abdominal aorta.
In the setting of trauma, ultrasound is not the definitive imaging modality; however, it may be used to triage unstable patients in whom renal injury is suspected but who cannot undergo CT. An evolving application of ultrasound in trauma uses semiquantitative Doppler measurements to evaluate renal blood flow. The renal Doppler resistive index, a measurement of tissue resistance to perfusion caused by vasoconstriction, has been shown to predict occult hemorrhagic shock in normotensive polytrauma patients with high sensitivity and specificity.47
One of the major advantages of ultrasound is that it can be performed directly at the point of care, in conjunction with the physical examination and without having to move the patient to the radiology suite. Sonography in this fashion is being performed by urologists evaluating patients in the ED and is also helpful in remote or austere locations where other imaging may not exist.48,49
 CLINICAL INDICATIONS
CLINICAL INDICATIONS
Indications for ultrasound examination of the urinary tract in the emergency and acute care setting are as follows:
 Acute flank pain/suspected renal colic
Acute flank pain/suspected renal colic
 Acute urinary retention and bladder size estimation
Acute urinary retention and bladder size estimation
 Acute renal failure
Acute renal failure
 Hematuria
Hematuria
 Acute pyelonephritis and renal abscess
Acute pyelonephritis and renal abscess
 Possible renal mass
Possible renal mass
 Trauma
Trauma
ACUTE FLANK PAIN/SUSPECTED RENAL COLIC
A focused point-of-care ultrasound examination of the kidneys is indicated for evaluation of the patient with suspected renal colic. Because of the prevalence of renal stone disease, this diagnosis is in the differential of all patients presenting with abdominal or flank pain. While ultrasonography is primarily utilized in patients presenting with flank pain and hematuria, its use also may be considered in the broader group of patients with undifferentiated abdominal pain and the absence of hematuria since renal stone disease may present in this fashion as well.
Studies have reported very high sensitivity of ultrasound for the detection of urolithiasis.44,50 These studies employed specific protocols, including fasting and IV hydration prior to a comprehensive renal ultrasound that can last up to 30 minutes. Such conditions are not always possible in the ED; more importantly, the goal of emergency renal ultrasound is not to identify stones, but rather to detect hydronephrosis, an important consequence of obstructive uropathy (Figure 12-1). The ability to detect acute urinary obstruction is what makes ultrasound an invaluable tool in the emergency setting.51 Sensitivity and specificity of point-of-care ultrasound for the detection of hydronephrosis range from 80% to 94% and 82% to 99%, respectively.18,41,42,52,53 This is comparable to the sensitivities reported in the urology literature for point-of-care ultrasound48 and in the radiology literature for traditional renal ultrasound.43,50,54
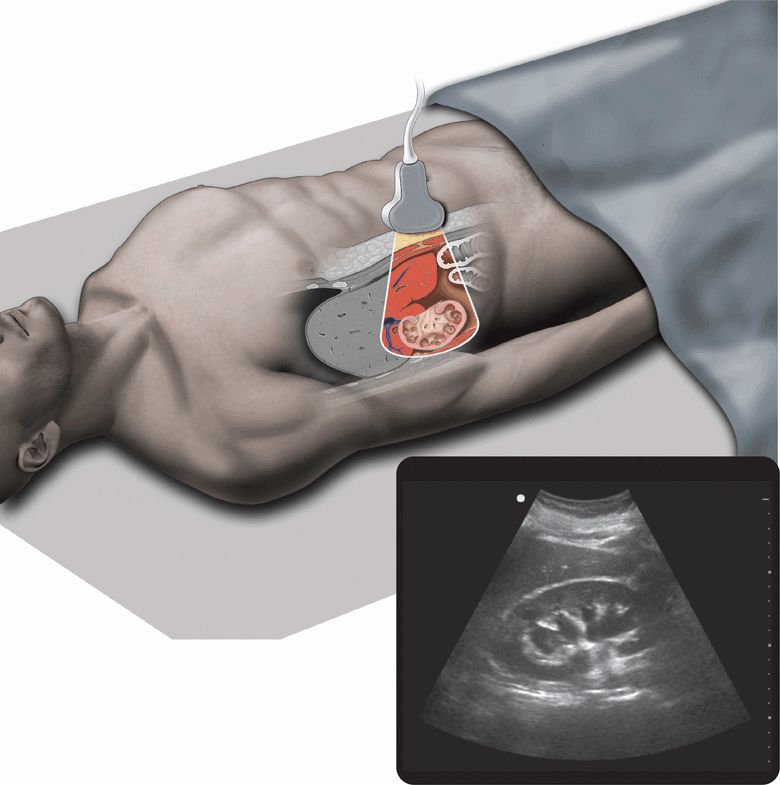
Figure 12-1. Hydronephrosis. Ultrasound techniques and findings are outlined in the corresponding sections of this chapter.
In patients who have no or mild hydronephrosis, a ureteral calculus larger than 5 mm is unlikely.45 Patients who are dehydrated may fail to show the signs of hydronephrosis on ultrasound,20,56 and it is for this reason that oral or IV hydration is recommended before obstructive hydronephrosis can be excluded. Conversely, a patient with a full bladder may have the appearance of bilateral hydronephrosis; if such a situation is encountered, the ultrasound examination should be repeated after the patient voids.56 Because of the variations in hydration and bladder volume, it is extremely important to obtain images of both kidneys (for comparison) and the bladder, and to correlate point-of-care ultrasound findings with the clinical picture.
The persistence of bilateral hydronephrosis may indicate bladder outlet obstruction and thus further study is indicated. With long-standing hydronephrosis, thinning of the medulla and cortex begins to occur.46 The presence of right-sided hydronephrosis is a common finding in pregnancy and should not be confused for pathology.57 Occasionally, the finding of calyceal rupture will be noted by the presence of perinephric fluid with mild-to-moderate hydronephrosis. The finding of urinary extravasation is a specific sign of severe acute urinary obstruction and should prompt urgent urologic consultation.
In a patient without hematuria and a negative point-of-care ultrasound examination for hydronephrosis, the diagnosis of renal colic becomes extremely unlikely; the negative predictive value of this combination is high.41 If microscopic hematuria is present and no hydronephrosis is seen, the consideration of other diagnoses should be made even though the diagnosis of renal stone is still possible. Those diagnoses that are immediately life threatening, such as a ruptured abdominal aortic aneurysm (AAA), must be considered in either scenario. Once the clinician is satisfied that more serious pathologies are not present, the patient may be discharged for further workup as necessary on an outpatient basis, which may include CT, comprehensive renal ultrasound, or stone analysis, if collected. The presence of a solitary kidney, renal failure, or urinary tract infection may be indications for admission or further investigation, despite the absence of significant hydronephrosis, when the diagnosis of renal stones is still under consideration.
An algorithm for the evaluation of renal colic that incorporates the use of focused emergency ultrasonography is outlined in Figure 12-2. Some investigators have used a similar algorithm to safely discharge >50% of patients presenting to the ED with flank pain using only urinalysis, analgesia, and point-of-care ultrasound of the kidneys and aorta.53
Figure 12-2. Algorithm for the evaluation of renal colic.
An evolving technique in the evaluation of renal outflow obstruction involves the imaging of ureteral jets.58,59 In the normal bladder, the intermittent ejection of urine into the bladder from the ureters can be visualized in real-time examination.
ACUTE URINARY RETENTION AND BLADDER SIZE ESTIMATION
Point-of-care ultrasound can assist in the evaluation of patients with symptoms of acute urinary retention. The placement of a urinary catheter for residual urine, as both a diagnostic and therapeutic procedure, has been the traditional approach when acute urinary retention is being considered. Although this approach does quantify the amount of urine retained, it is uncomfortable for patients and incurs a risk of infection. It is therefore preferable to avoid this procedure unless it is clear that urinary retention exists.
Ultrasound can immediately confirm and quantify the degree of obstruction and retention by imaging the urinary bladder and estimating its size. Many of the studies examining bladder volume have been performed by urologists in conjunction with urodynamic measurements.5,7–12,59–67 In this setting, even small degrees of error may be unacceptable. By contrast, a qualitative estimate of bladder size may be very helpful in the emergency setting. Bedside ultrasound can easily classify the bladder volume as small, medium, or large, helping the clinician determine the need for emergent urinary catheterization. The presence of a large distended bladder mandates emergency urinary catheterization, whereas an empty or small bladder on ultrasound suggests another cause for the patient’s symptoms. An intermediate size may require bladder volume measurements to determine the need for catheterization. Whenever the bladder is imaged in this fashion, examine the kidneys for bilateral hydronephrosis, a concerning complication of long-standing bladder outlet obstruction.
When quantitative data are necessary, as in the evaluation of patients with possible spinal cord compression or cauda equina syndrome, ultrasound can reliably estimate the postvoid residual urinary volume. Studies performed on postoperative patients have demonstrated that three-dimensional measurements correlate with volume measured by catheter drainage, which may obviate the need for this invasive procedure (Figure 12-3).67
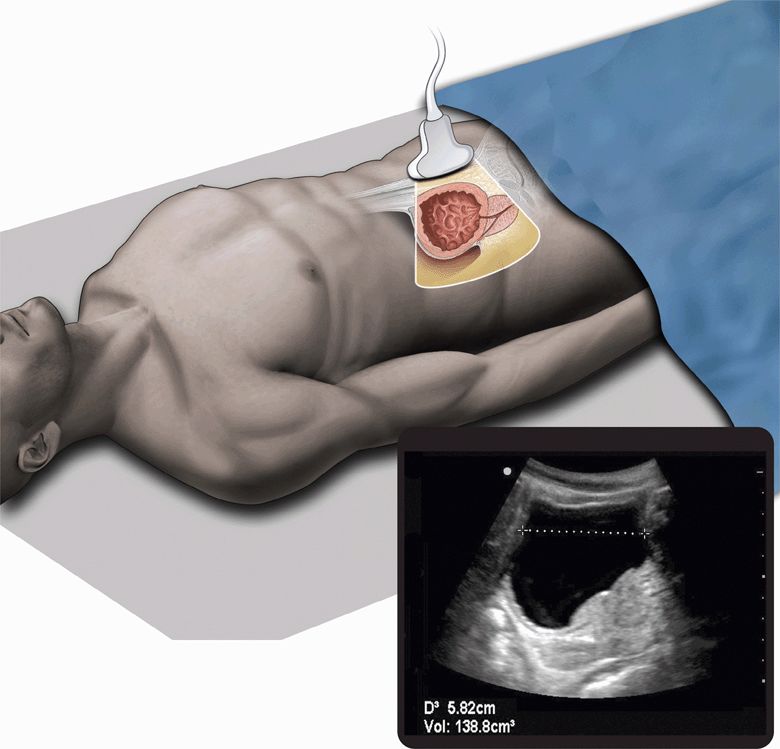
Figure 12-3. Urinary retention. Ultrasound techniques and findings are outlined in the corresponding sections of this chapter.
Another indication for point-of-care ultrasound of the urinary tract is the assessment of bladder volume prior to urinary catheterization of children. Studies have demonstrated that confirming the existence of urine in the bladder prior to catheterization can successfully reduce or even eliminate unsuccessful procedures,13,14 which are painful and often very traumatic.
ACUTE RENAL FAILURE
Renal ultrasound can be a useful adjunct in the evaluation of acute renal failure. The clinical evaluation of acute renal failure begins with a determination of whether the cause is proximal to the kidneys (“pre-renal” failure), distal to the kidneys (“post-renal” failure), or intrinsic to the kidneys themselves (“renal” failure). Because post-renal causes such as obstruction of either ureteric or urethral outflow are readily reversible if identified in a timely fashion, these are most often considered first in the evaluation. Ultrasound is clearly an effective tool in the identification of post-renal obstruction, easily detecting bilateral hydronephrosis, and bladder distention. If only a solitary kidney is visualized and hydronephrosis is present, the need for acute decompression becomes particularly urgent. Moreover, prostatic enlargement, one of the most common causes of lower tract obstruction, can be identified on ultrasound.
After a post-renal cause has been excluded, renal ultrasound may provide still further diagnostic information. Although pre-renal causes of renal failure will not generally cause sonographic abnormalities, several causes of acute and acute-on-chronic intrinsic renal failure will manifest themselves on ultrasound examination. Small, atrophic, and hyperechoic kidneys suggest chronic pathologic processes such as hypertensive nephropathy and chronic glomerulonephritis. The finding of enlarged kidneys with multiple cysts distorting the renal architecture suggests polycystic kidney disease (PCKD) as the cause of renal failure. Unfortunately, many causes of acute renal failure that are intrinsic, such as acute glomerulonephritis and acute tubular necrosis, may have nonspecific or minimal sonographic findings. Furthermore, different clinical entities may have different sonographic manifestations at different stages in their presentation. For this reason, other clinical methods, such as volume status determination, response to fluid therapy, microscopic urinalysis, and measurement of the fractional excretion of sodium must be utilized to distinguish between pre-renal and intrinsic causes of renal failure and guide therapy. Renal biopsy, often necessary to establish a definitive diagnosis, may be facilitated by ultrasound guidance.
HEMATURIA
Hematuria occurs in a vast array of medical conditions. In the patient with renal colic, hematuria is a common finding. However, presence of red blood cells on urinalysis has been found to be nonspecific and may occur in life-threatening conditions such as AAA, ectopic pregnancy, and appendicitis. Patients with microscopic hematuria may benefit from a screening bedside renal ultrasound to rule out hydronephrosis, AAA, and any obvious bladder or renal mass. Initial evaluation of patients with gross hematuria should include a bedside renal ultrasound in addition to laboratory testing of hematocrit and renal function.
In the setting of blunt trauma, patients may have microscopic or gross hematuria. Hemodynamically stable patients with profound hematuria in the setting of trauma should undergo contrast-enhanced CT.
ACUTE PYELONEPHRITIS AND RENAL ABSCESS
Acute pyelonephritis, an extremely common emergency diagnosis, does not necessarily require imaging. In fact, the sonographic appearance of the kidney in acute pyelonephritis is most commonly normal.51 However, in complex cases or those not responding to medical management, ultrasound may be helpful in ruling out complications of pyelonephritis that require surgical management. For example, the formation of a renal abscess may complicate pyelonephritis. Renal abscesses are typically solitary, round hypoechoic masses, often with internal septations or mobile debris, and a degree of posterior acoustic enhancement.51,57 Suspicious lesions identified in the course of the point-of-care ultrasound may prompt consultation with a urologist, a comprehensive sonographic study, and, in some cases, CT scanning to further characterize the lesion and formulate a surgical treatment plan.68 Perinephric abscesses extend beyond the kidney and may be visualized on ultrasound, but are better evaluated with CT. This modality should be sought when lesions are seen to extend beyond the kidney on ultrasound.51
Emphysematous pyelonephritis, a rare but life-threatening infection, deserves special mention. Patients with this infection are most frequently diabetic or immunocompromised for other reasons. Because patients with emphysematous pyelonephritis may have toxic and nonspecific presentations, suggestive findings on point-of-care ultrasound may prompt surgical intervention (either percutaneous drainage or open nephrectomy) that would have otherwise been overlooked or unduly delayed.69–71
POSSIBLE RENAL MASSES
Renal masses are being seen with increasing frequency as a result of both emergency sonography and the incorporation of screening abdominal ultrasound into periodic health evaluations.15,18,72–74 There is no question that the mortality and morbidity of malignancies detected in this incidental fashion are greatly reduced.75–77 Although there is concern regarding the cost-effectiveness of routine use of ultrasound in the absence of specific symptomatology, a mechanism for the follow-up of abnormalities found in the emergency and acute care setting must be available. It cannot be overemphasized that the focused use of ultrasound to evaluate a patient for hydronephrosis is not a substitute for comprehensive sonography or other follow-up studies. Moreover, renal masses discovered on ultrasound almost always require further characterization with another modality, usually CT.51 The majority of malignancies seen in the kidney are renal cell carcinoma (RCC).16,74,78,79 These tumors are extremely variable in their sonographic appearance and may be isoechoic, hyperechoic, or hypoechoic relative to the adjacent parenchyma. It is also important to note that many of these tumors have a partially cystic presentation and may be mistaken for a simple benign cyst.51
Another common tumor seen in the kidney is angiomyolipoma (AML).51,78 These tumors are mostly benign and may be treated conservatively.80 Although they are usually well demarcated and brightly echogenic on ultrasound, there is a significant overlap in their sonographic appearance with that of echogenic RCC.81 This serves to underscore the caution that is required in the interpretation of any mass found incidentally during ultrasound. Any such finding requires follow-up with a comprehensive ultrasound examination, a CT scan, or urologic consultation.
Other tumors that are commonly seen on ultrasound are lymphomas and metastatic malignancies, which commonly appear as irregular nodules, either single or multiple. These may also be diffuse, grossly disturbing the renal architecture or infiltrative, extending into the perirenal and surrounding structures.51 Transitional cell carcinoma (TCC), which is more commonly found in the bladder and ureter than in the renal pelvis, is frequently not visible on renal ultrasound. This is because it is frequently symptomatic (with gross hematuria) before sufficient tumor mass can be seen in the renal pelvis. Its sonographic appearance is one of a hypoechoic mass within the highly echogenic renal sinus.51
Renal cysts are an extremely common finding on ultrasound. Although simple cysts are benign, malignancies may present with a cystic appearance.82 For this reason, caution needs to be exercised before dismissing a lesion seen on sonography as a simple cyst.
PCKD can be recognized as an abundance of cysts of varying sizes that both enlarge and distort the regular renal architecture.51,57,82 Ultrasound is the modality of choice to evaluate this inheritable disorder, which may present with hematuria, flank pain, hypertension, or renal failure. Cysts are frequently present in multiple organs in the body, and there is an association with cerebral aneurysms.82 Urology or nephrology referral is indicated upon discovery of this disorder. Patients with chronic renal failure undergoing long-term dialysis also tend to develop multiple renal cysts. This disorder, known as acquired renal cystic disease (ARCD), is characterized by a huge increase in the incidence of renal malignancies, and for this reason regular surveillance of this condition is indicated.51,82
RENAL TRAUMA
The primary sonographic indicators of major renal trauma are subcapsular hematoma, perinephric hematoma, or calyceal dilation associated with internal echogenicity. These findings may be recognized on the initial trauma ultrasound screening examination or on subsequent examinations. Studies show that while standard B-mode sonography has high specificity for urologic trauma, the sensitivity is low and may miss significant injuries.83–85 Therefore, hemodynamically stable patients with major trauma in whom injury of the renal pedicle is suspected are best evaluated with contrast-enhanced CT, which provides information about renal function and is considered the modality of choice.83 If CT is not available, newer ultrasound techniques such as color Doppler or contrast ultrasound may provide much more information than standard B-mode sonography.86–89
Ultrasound may have a role in the follow-up and management of patients with identified parenchymal injury, such as hematomas and lacerations. These lesions are often well visualized by ultrasound and can be evaluated periodically to monitor their resolution.
 ANATOMICAL CONSIDERATIONS
ANATOMICAL CONSIDERATIONS
COMPARTMENTS OF THE RETROPERITONEUM
Before describing the gross anatomy of the kidney, ureter, and bladder, it is first important to review where these structures lie within the abdominal cavity and their relation to surrounding structures.
The retroperitoneal cavity is divided into three distinct compartments (Figure 12-4), with the kidneys occupying the middle or perirenal compartment. The anterior compartment contains the duodenum, pancreas, descending colon, celiac trunk, and superior mesenteric vessels, as well as associated fat. The posterior compartment, which lies anterior to the quadratus lumborum and psoas muscles, simply contains fat. The anterior and posterior compartments are also referred to as the pararenal compartments.
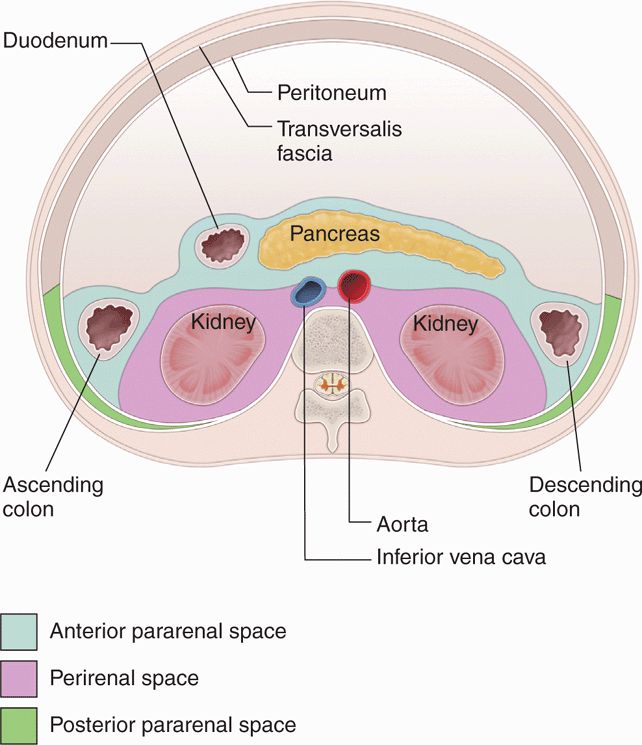
Figure 12-4. Anatomic compartments of the retroperitoneum.
The perirenal compartment is bounded by Gerota’s fascia both anteriorly and posteriorly, although many authors refer to the posterior component of the renal fascia as Zuckerkandl’s fascia. This fascia, which invests the kidneys, adrenal glands, renal hila, proximal collecting system and perinephric fat, merges laterally to form the lateroconal fascia that extends to the parietal peritoneum of the lateral paracolic gutter. This completes the separation of the anterior and posterior retroperitoneal compartments. Thus, the kidneys are surrounded by two distinct layers of fat: the perinephric fat, which lies immediately outside the true fibrous capsule of the kidney, bounded by Gerota’s fascia, and the paranephric fat, which lies in the pararenal compartments outside of Gerota’s fascia.
This compartmentalization of the retroperitoneum is important clinically as it serves to localize various pathologic processes. It also creates a barrier to the progression of various pathologic processes such as hemorrhage and infection. Collections of fluid in the anterior pararenal compartment, for example, are commonly related to pancreatitis or trauma, whereas collections of fluid in the posterior pararenal compartment are uncommon, usually representing spontaneous hemorrhage in patients with coagulopathy or related to trauma.
ANATOMIC RELATIONSHIPS OF THE URINARY SYSTEM
There is significant asymmetry in the position of the two kidneys within the abdominal cavity. The right kidney is bounded anteriorly by the liver, which serves as an excellent acoustic window for sonography. It is usually slightly larger and slightly inferior to the left kidney. The left kidney is bounded anteriorly by several structures, including the pancreas, stomach, spleen, and large and small bowel, making it somewhat more difficult to image, as only the spleen serves as an acoustic window of equal quality to the liver. Both kidneys have symmetrical relationships, with the diaphragms superiorly and the musculature of the retroperitoneum (psoas and quadratus) posteriorly. In the supine position, the superior pole of the left kidney is at the level of the 12th thoracic vertebrae and the inferior pole is at the level of the 3rd lumbar vertebrae. However, it is important to realize that the kidneys are mobile structures within the retroperitoneum, moving with changes in position and with phases of respiration. Figure 12-5 demonstrates the anatomical relationships of the two kidneys.
Figure 12-5. Anatomic relationship of the kidneys.
The renal hilum is the specific area of the sinus where the renal artery enters and the renal vein and ureter exit the kidney on its medial concave surface. The ureters, which arise from the hila of each kidney, travel inferiorly toward the bladder in close relation to the psoas muscle, just anterior to the transverse process of the lumbar spine. As they enter the pelvis, they course medially to cross the iliac vessels and then laterally once again to parallel the margins of the bony pelvis before inserting posteriorly into the bladder.
The bladder, when empty, abuts the posterior aspect of the pubis. As it fills, it expands to fill more of the pelvis, displacing bowel loops into the abdomen. A distended bladder moves into the lower abdomen and gains relationships to the anterior abdominal wall.
RENAL ANATOMY
The kidneys are paired structures that lie obliquely with respect to every anatomic plane. They are situated so that their inferior poles are anterior and lateral to their superior poles. In addition, each hilum is directed obliquely in an anteromedial rather than simply medial orientation. The sonographic significance of this orientation is that the technique for imaging the kidneys must involve adjusting the transducer obliquely in each plane to match the anatomy.56,90
Each kidney is between 9 and 13 cm in its maximum longitudinal measurement, and they decrease in size with advanced age and chronic renal failure. The approximate width and depth of the kidneys is 5 cm and 3 cm, respectively. Each kidney is surrounded by a true fibrous capsule and can be divided into two parts (Figure 12-6), the renal parenchyma and the renal sinus. The renal parenchyma, which surrounds the sinus on all sides except at the hilum, is composed of the outer cortex, consisting of the filtration components of the nephrons, and the inner medulla, consisting of the reabsorptive components (loops of Henle). The cone-shaped medullary pyramids are oriented with their apices, or papillae, protruding inward toward the renal sinus. Thus, the functional unit of the kidney, or renal lobe, consists of a medullary pyramid and its surrounding cortex: urine being filtered by the cortex and then excreted through the papillae into the collecting system. There are between 8 and 18 such lobes in each kidney, bounded by interlobar arteries and veins. The arcuate arteries, which branch from these interlobar arteries, are found at the base of the medullary pyramids and can serve as important landmarks in the interpretation of sonographic images.
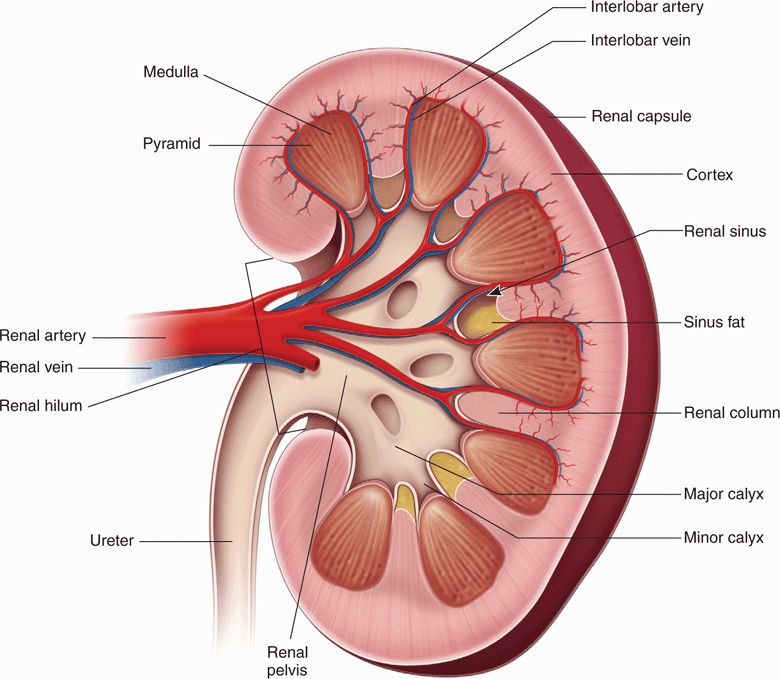
Figure 12-6. Gross anatomy of the kidney.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 CLINICAL CONSIDERATIONS
CLINICAL CONSIDERATIONS CLINICAL INDICATIONS
CLINICAL INDICATIONS ANATOMICAL CONSIDERATIONS
ANATOMICAL CONSIDERATIONS GETTING STARTED
GETTING STARTED TECHNIQUE AND NORMAL ULTRASOUND FINDINGS
TECHNIQUE AND NORMAL ULTRASOUND FINDINGS COMMON ABNORMALITIES
COMMON ABNORMALITIES COMMON VARIANTS AND OTHER ABNORMALITIES
COMMON VARIANTS AND OTHER ABNORMALITIES PITFALLS
PITFALLS CASE STUDIES
CASE STUDIES