Retinal and Choroidal Blood Flow
Timothy Q. Duong
Eric R. Muir
Retinal Anatomy and Blood Flow
Anatomy
Vision begins at the retina where light is converted into neurochemical and electrical signals. The retina is part of the central nervous system and is made up of multiple structured anatomical layers.1 Starting from the inner layers of the retina at the vitreous and going back toward the choroid, the anatomical layers of the retina are the ganglion cell and nerve fiber layer, inner plexiform layer, inner nuclear layer, outer plexiform layer, outer nuclear layer, inner and outer segments, and retinal pigment epithelium.1 The choroid and sclera are located behind the retinal pigment epithelium, which separates them from the neural retina. Light absorbed in the outer segment of the photoreceptors initiates the signal cascade. The neurochemical and electrical signals propagate through the retina toward the vitreous to the retinal ganglion cells.
The retina is nourished by two separate circulations: the retinal and the choroidal vessels, located on either side of the retina. Both circulations derive from the ophthalmic artery. The retinal vasculature is mainly localized in the inner surface of the retina in the ganglion cell layer, with capillaries protruding into the inner nuclear and inner plexiform layers.1,2 The choroidal vasculature is located outside the neural retina between the retinal pigment epithelium and the sclera. The choriocapillaris, a dense sheet-like layer of capillaries, is next to the retinal pigment epithelium with the larger vessels more posterior in the choroid.3 The choroid primarily nourishes the outer retina and the retinal vessels nourish the inner retina. The photoreceptor cell layers of the outer retina, comprised of the outer nuclear layer and the inner and outer segments, are avascular, situated between the retinal and choroidal vessels. These layers receive oxygen by diffusion, primarily from the choroid. Both circulations have a blood–tissue barrier, protecting the neural retina. The inner blood–retinal barrier consists of endothelial cells, forming tight gap junctions around the retinal vessels, similar to the blood–brain barrier.4 The outer blood–retinal barrier is the retinal pigment epithelium, a sheet of epithelial cells separating the choroid from the neural retina. The choriocapillaris does not have tight gap junctions and in fact has many fenestrations.4 The neural retina is only about 200 to 300 μm thick across many mammalian species.5,6,7 The choroid thickness is less than 90 μm thick in rodents5 and 150 to 300 μm thick in humans, depending on location.8
Blood Flow
The retinal and choroidal vasculatures and blood flow are quite different. The choroid has high vascular density, which gives it one of the highest blood flows of any tissue. Retinal blood flow is similar to cerebral blood flow, and both are much lower than choroidal blood flow. The high choroidal blood flow could be needed to establish a large oxygen gradient between the choroid and outer retina, driving oxygen diffusion to the outer retina.9,10 Retinal blood flow is reported to range from 0.14 to 1.66 mL/g/min, determined by invasive methods in animals such as microspheres and autoradiography, and choroidal blood flow is reported to range from 7 to 19 mL/g/min.9,11,12,13,14,15,16
The two circulations are also regulated differently by various factors.9,17 The retinal vasculature is regulated locally by the metabolic needs of the retinal tissue it supports. Choroidal vessels are separated from the tissue they support (the outer retina) and might not be regulated by the local outer retinal metabolic status. Hyperoxia decreases retinal blood flow,18 and hypoxia causes it to increase.12 Oxygen does not affect the choroidal vessels.19 But both retinal and choroidal blood flow are responsive to carbon dioxide. Hypercapnia increases retinal and choroidal blood flow,19,20 and both blood flows decrease during hypocapnia.21 Flicker visual stimulation will cause retinal blood flow to increase,22 but it is inconclusive whether the choroidal vasculature responds to flicker.23,24 Both circulations autoregulate in response to changes in the ocular perfusion pressure,25,26 the difference in arterial blood pressure and intraocular pressure, although a lack of autoregulation in the choroid has also been reported.20,27 Finally, the choroid is richly innervated by sympathetic and parasympathetic nerves, although the retinal vessels lack any direct nervous control.9,28 Stimulation of sympathetic or parasympathetic nerves causes choroidal blood flow to decrease or increase, respectively.9,28
Retinal and Choroidal Blood Flow Measurement
Optical imaging techniques have been used to study the anatomy and physiology of the retina. Methods to image
retinal hemodynamics include fluorescein and indocyanine green angiography from which the dye transit time and velocity in large retinal vessels can be measured,29,30 laser Doppler velocimetry,18 which can measure blood velocity in large retinal vessels, and laser Doppler flowmetry,31 and laser speckle imaging,32 which detect a nonquantitative perfusion index in the tissue. Optical techniques, with the exception of optical coherence tomography, are depth limited. Some limitations of optical imaging are: (a) most optical signals come from the retinal surface with unknown amounts of contamination from the choroid, (b) many techniques are nonquantitative or provide data at only a discrete point instead of images, (c) optical techniques cannot be used if there is disease-induced opacity of the vitreous, cornea, or lens, and (d) choroidal blood flow cannot easily be assessed with optics because the choroid is located behind the retinal pigment epithelium. Destructive microsphere technique has also been used to measure quantitative blood flow of the retina and the choroid of animals.27
retinal hemodynamics include fluorescein and indocyanine green angiography from which the dye transit time and velocity in large retinal vessels can be measured,29,30 laser Doppler velocimetry,18 which can measure blood velocity in large retinal vessels, and laser Doppler flowmetry,31 and laser speckle imaging,32 which detect a nonquantitative perfusion index in the tissue. Optical techniques, with the exception of optical coherence tomography, are depth limited. Some limitations of optical imaging are: (a) most optical signals come from the retinal surface with unknown amounts of contamination from the choroid, (b) many techniques are nonquantitative or provide data at only a discrete point instead of images, (c) optical techniques cannot be used if there is disease-induced opacity of the vitreous, cornea, or lens, and (d) choroidal blood flow cannot easily be assessed with optics because the choroid is located behind the retinal pigment epithelium. Destructive microsphere technique has also been used to measure quantitative blood flow of the retina and the choroid of animals.27
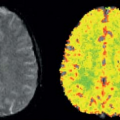
In contrast, magnetic resonance imaging (MRI) can measure blood flow noninvasively and quantitatively, and it provides the possibility of imaging both retinal and choroidal blood flow without depth limitation or signal contamination.
Challenges for Retinal Magnetic Resonance Imaging
In Vivo Issues
In contrast to optical techniques that have high temporal resolution, MRI takes on the order of seconds or minutes to acquire an image. Furthermore, relatively high MR spatial resolution is needed to image the thin retina. As such, multiple repetitions are needed to achieve sufficient signal-to-noise ratio (SNR), resulting in acquisition times of several minutes. Eliminating eye movement is critical for high-resolution MRI, especially during prolonged experiments with multiple measurements. Blood flow MRI of the retina is particularly susceptible to motion artifacts because the retina is very thin and is bounded by the sclera and vitreous, which have different signal intensities than the retina, and the arterial spin labeling (ASL) blood flow signal is dependent on subtraction between separate images (with and without labeling). Minimizing eye movement in animal and human studies entails different approaches. Image coregistration can also be used to align image sets in which eye motion does occur.33
Animals must be anesthetized for MRI, but depending on the anesthesia, motion may still occur. Ear bars and bite bars can be used to robustly immobilize the head, but the eye itself cannot easily be restrained. Thus, the eye can still drift under anesthesia, with the extent of motion dependent on the anesthetic used.34 For instance, the eye is prone to movement under isoflurane, but the combination of isoflurane and a paralytic (pancuronium bromide) eliminates eye movement. Anesthetics such as ketamine with xylazine and urethane produce less eye movement compared with isoflurane alone.34
In human retinal MRI, blinking and eye fixation must be considered. The average duration between human eye blinks is approximately 5 seconds, with a 4- to 8-second blinking period being comfortable.35 MRI pulse sequence parameters should be set with the repetition time of each scan within this range of blinking rates, while allowing a few seconds without data readout to blink. To minimize eye movement, subjects could maintain stable eye fixation on a target inside the magnet bore during data readout, which generates distinct sound cues from the gradients. Using an eye tracker in humans, the displacement of the retina over time during fixation ranges up to 150 μm, with standard deviations over time of 78 and 130 μm for horizontal and vertical eye movements.35 Such displacements can limit human retinal MRI resolution to approximately 100 μm unless eye-fixation stability can be improved with trained eye fixation.
Resolution, Partial Volume, and Signal-to-Noise Ratio
Layer-specific blood flow MRI of the retina requires very high spatial resolution. Because of the limited MRI resolution, partial volume effects, because of the thin retina and its curved geometry, could be significant both in-plane and across the slice thickness. Partial volume effect on blood flow MRI would likely result in underestimated blood flow of the retina or choroid because the vitreous and sclera on either side of the retina have little or no blood flow. In-plane spatial resolutions of 40 to 50 μm have been targeted for retinal and choroidal blood flow layer-specific imaging in rodents.36 In human studies, a spatial resolution of up to 500 μm has been used.37
Assuming a spherical eye, the partial volume through the imaging slice thickness, because of the curvature of the retina through the slice, can be estimated. For a rat eye, assuming a 6-mm diameter and 270-μm thick retina and choroid, a 0.5- and 1.0-mm thick slice would have partial volume of 3% and 13%, respectively, of the total retinal thickness.5 For the larger human eye, a thicker imaging slice can be used. For a human eye, assuming a 25-mm diameter and 600-μm thick retina and choroid, a 6-mm thick slice gives significant partial volume of 61% of the total thickness.37
Partial volume effects can be reduced by increasing spatial resolution, but low SNR is another problem because of the high MRI spatial resolution needed, as
well as the low SNR of ASL blood flow data. Small, high-sensitivity surface coils optimized for imaging the eye, low-noise preamplifiers, high magnetic field scanners, and additional signal averaging (albeit with a longer scan time) can be used to improve SNR. Longer scans can, however, become more prone to eye movements. Improved gradient capability, parallel imaging, and other fast acquisition techniques are expected to improve spatial and temporal resolution.
well as the low SNR of ASL blood flow data. Small, high-sensitivity surface coils optimized for imaging the eye, low-noise preamplifiers, high magnetic field scanners, and additional signal averaging (albeit with a longer scan time) can be used to improve SNR. Longer scans can, however, become more prone to eye movements. Improved gradient capability, parallel imaging, and other fast acquisition techniques are expected to improve spatial and temporal resolution.
Hardware Issues
Layer-specific blood flow MRI of the retina requires very high spatial resolution, which could lead to hardware-related instability because (a) high-resolution MRI is demanding on the magnetic gradients, which can lead to temperature-dependent frequency or phase drifts, resulting in spatial drift of the image and (b) the small high-resolution voxel size makes image drift more apparent. Avoiding or correcting hardware-related issues will result in more stable and reliable MRI data. Careful shimming is also important because the eye is in a region of large magnetic field inhomogeneity, particularly for fast MRI sequences commonly used for blood flow MRI such as echo-planar imaging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree