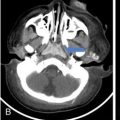
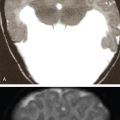
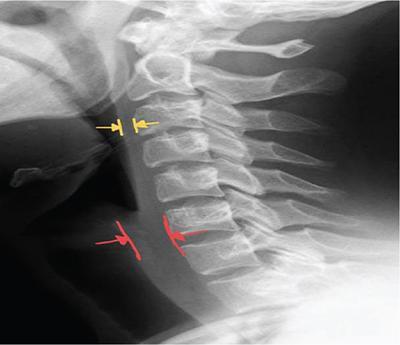
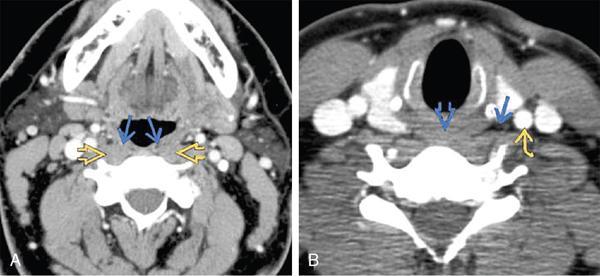
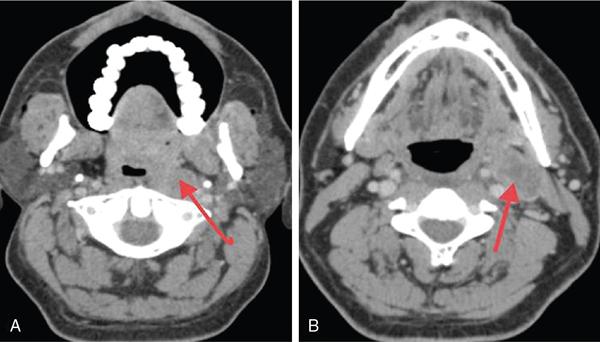
Rajendra Solanki, Shital Turkhiya, Natisha Arora, Amar Suri, Digish Vaghela KEY POINTS Retropharyngeal space (RPS) extends from the skull base to the mediastinum. It is a potential space posterior to pharynx in the upper part and posterior to the oesophagus in the lower part of the neck. Small lesions of RPS are typically not evident on clinical examination. Thus, radiological investigations play a key role in identifying their nature and delineation. RPS is commonly secondarily involved site in common inflammatory conditions such as suppurative retropharyngeal adenitis and less often involved in true retropharyngeal abscess and mucosal origin malignancies. Located anterior to cervical and upper thoracic vertebrae and prevertebral muscles, RPS extends superiorly to base of skull and inferiorly to posterior mediastinum up to the level of tracheal bifurcation. Anterior margin of posterior pharyngeal wall superiorly and posterior aspect of oesophagus inferiorly. Middle layer of deep cervical fascia (ML-DCF) envelopes the RPS. Prevertebral fascia, which is a deep layer of deep cervical fascia (DL-DCF). Skull base where ML-DCF and DL-DCF inserts. The DL-DCF, known as the alar fascia, extends in coronal orientation and divides RPS into two components. However, it is not possible to differentiate the aforementioned two compartments on imaging and so is simply considered as a single compartment. The lateral limits of the RPS are defined by alar fascia. Alar fascia separates RPS from carotid vessels in carotid sheath; however, it is less resistant to the spread of pathology arising from RPS. Thus, RPS fluid collections often extend laterally to carotid space. In the suprahyoid RPS, below the skull base, the RPS is located between prevertebral muscles and the pharynx and contains very little fat. Retropharyngeal nodes, also known as lymph nodes of Rouviere, are located in the far lateral aspect of the RPS, immediately medial to the internal carotid arteries (ICAs). These nodes drain the nasopharynx, oropharynx, nasal cavity, paranasal sinuses, middle ear and prevertebral space. This is most evident in children, where large non-necrotic lateral RPS nodes, in association with prominent adenoidal tissue, are normal findings. These nodes usually regress by puberty. Infrahyoid RPS contains only fat and, thus, can be involved only by nonnodal disease. RPS appears as rectangular space on axial cross-sectional imaging, wider in mediolateral dimension and thinner in anteroposterior direction. Imaging modalities such as plain radiography, fluoroscopy, multidetector computed tomography (MDCT), magnetic resonance imaging (MRI) and positron emission tomography/computed tomography (PET/CT) are useful for evaluation of lesions in RPS. However, the presence of fat in the RPS makes this space easily identifiable on CT (low density) and on MRI (high intrinsic T1 and T2 hyperintensity). Usually lateral view used to assess RPS pathology, especially in paediatric age group. Proper positioning is important as neck flexion may cause pseudothickening of prevertebral soft tissues. Presence of RPS pathology usually causes widening of prevertebral soft tissue. Normal prevertebral soft tissue on lateral radiograph (Fig. 3.18.1). X-rays and fluoroscopy are widely replaced by cross-sectional images such as CECT and MRI with MRI being the investigation of choice in imaging of head and neck pathologies because of its higher soft-tissue resolution and no radiation hazard. CECT is the second preferred investigation (Fig. 3.18.2). Imaging must cover from the skull base to mediastinum because of potential for mediastinal extension of disease. Contrast given by intravenous route is important to determine the enhancement characteristics of an RPS lesion. Plain scan followed by CECT as per requirement, from skull base to mediastinum. Although having radiation hazard, it is having shorter duration than MRI, so study of young children can be done without sedation as compared with MRI. Plain and contrast imaging is done. T1W, T2W, T1/T2 fat-saturated and postgadolinium T1-weighted images are acquired. Ultrasound has a limited role in evaluation of RPS lesions. Deeper pathologies are not accessible by ultrasound. PET/CT allows the detection of disease in the RPS as well as metastatic nodes in unknown primary in RPS. RPS is rarely involved by primary lesions. Two major disease processes that involve RPS are secondary to malignancy from head and neck and infection, the latter being more common. There are mostly secondary to primary head and neck malignancies. Infection usually primarily involves palatine tonsils and nasopharyngeal adenoids; however, spread of infection to retropharyngeal lymph nodes can result in suppuration of lymph nodes with cellulitis and abscess formation. Retropharyngeal lymphadenopathy is an imaging diagnosis, as the nodes cannot be clinically evaluated. Benign enlargement of retropharyngeal lymph nodes usually occurs secondary to infection such as pharyngitis, tonsillitis or generalized systemic viral infection and is commonly seen in children less than 10 years of age. Clinical symptoms are mainly from the primary infection source. Rarely large nodes may deform the pharyngeal contour causing airway compression. NECT/CECT: Often lymph nodes appear as isodense to muscle, making them difficult to detect on plain scan. They may show variable enhancement, usually mild. They are usually <1 cm in size. MRI with IV gadolinium depicts homogeneous low-to-intermediate signal on both T1- and T2-weighted images with variable enhancement on contrast studies. Head and neck infections commonly affect RPS nodes after bacterial pharyngitis. If the infection left untreated, it progresses to suppuration. If still untreated, it develops to abscess formation. Common signs and symptoms are sore throat, odynophagia and elevated WBC count and ESR. It is usually seen in children and young adults and is uncommon in patients >30 years. Extensive cellulitis associated with inflammation and large abscess formation may narrow the airway. Management is to give antibiotics and incision and drainage if it progresses to abscess formation. NECT/CECT: Low density within enlarged lymph node with peripheral enhancement is seen. Associated RPS cellulitis causes prevertebral soft-tissue fullness; rarely, there may be ICA vasospasm, usually self-limited. MRI depicts focal central T2 hyperintensity with increased signal intensity in surrounding tissues. DWI shows restricted diffusion within the suppurative node. T1WI C+ depicts peripheral node and adjacent soft-tissue enhancement. RPS malignant nodes are often clinically occult. Primary cancers which may spread to retropharyngeal lymph nodes are nasopharyngeal carcinoma and squamous cell carcinoma of oral cavity and larynx especially if there is involvement of posterior pharyngeal wall (Fig. 3.18.3A and B). Oral cavity and paranasal sinuses tumours and other non–SCC-like papillary thyroid carcinoma, melanoma and esthesioneuroblastoma can also metastasize to retropharyngeal lymph nodes and should be considered in differential diagnosis of malignant RPS nodes. Pathological markers for malignancy are of size >0.8 cm, any node in medial RPS or nodal necrosis and extracapsular spread irrespective of the size (Figs 3.18.4 and 3.18.5). In the absence of known primary, secondary malignant RPS nodes should raise suspicion of malignancy in pharyngeal mucosal space and nasopharynx and should be thoroughly inspected. Poor prognosis is indicated in patients with malignant RPS nodes and primary outside nasopharynx.
3.18: Retropharyngeal space
Abbreviations
Introduction
Anatomy
Boundaries
Anterior
Posterior
Superior
Inferior
Lateral
Imaging approach
Radiographs
Computed tomography
Magnetic resonance imaging
Other modalities
Approach to pathologies
Pathologies related to lymph node
RPS nodes/nodes of rouviere/nodal hyperplasia
Imaging.
Retropharyngeal adenitis, intranodal abscess
Imaging.
Malignant retropharyngeal space nodes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree