Strong potential for success
Relative potential for success
Persistent hip joint pain as confirmed by history/exam/intra-articular injection
Index procedure included implantation of nonabsorbable implants
Under- or unaddressed FAI
MRI signs of failure to heal at prior intended repair
Minimal degenerative hip disease
New onset of different pain in previously untreated area
Intact labrum without prior repair or healed prior repair
Reasonable expectations
Persistent capsular insufficiency (iatrogenic)
No narcotic medication requirement
Persistent feeling of instability
Absence of major dysplastic or extra-articular impingement morphology
Thickened capsule or adhesions visible on MRI
Persistent painful psoas snap
Persistent mechanical symptoms
Table 35.2
Authors’ experience with poor indications for revision hip arthroscopy (Evidence-Based Medicine Level of Evidence: 5)
Objective | Subjective |
|---|---|
Progressive and severe degenerative joint changes | Pain in a location inconsistent with hip pathology |
Severe hip dysplasia | Incomplete or no response to prior treatment performed |
Absence of abnormal hip findings on exam or radiographs | Without complication and without surgical implants |
Severe bone deformity in areas inaccessible to arthroscopic exposure | Lack of definably different surgical goals in the setting of persistent hip area pain |
Surgeon’s experience |
Clinical Evaluation of Patients with Persistent Dysfunction After Hip Arthroscopy
When evaluating a patient who has failed arthroscopic hip surgery, it is important to take a detailed history. It is important to identify the characteristics of pain that led to the first surgery and chronologic detail of the pain after that surgery. It is important to tease out if the pain is different in quality or intensity, whether there was a new trauma to the hip, or if the pain ever went away. Understanding the patients and their expectations and insight into their problem is an art that comes with experience but is vital in counseling and educating patients.
Physical exam should include a comprehensive evaluation of all possible causes of hip pain. This includes multi-positional musculoskeletal exam to evaluate gait, stance, core strength, lumbosacral spine pathology, pinpoint areas of maximal tenderness, hip range of motion, provocative maneuvers, weakness, and abnormal sensation or reflexes. It should also include a basic abdominal exam to rule out non-musculoskeletal causes of hip pain. We defer female pelvic exams, but if there is any question of a genitourinary cause of hip or groin pain, a referral to the gynecologist is initiated. Comprehensive review of the history and physical exam in this patient group are beyond the scope of this text, yet it is the opinion of the authors that these considerations are the best guides for selecting appropriate treatment for this patient group.
Imaging of Postoperative Hip
Postoperative changes can complicate the interpretation of imaging studies. Retained implants can cause distortion of MRI imaging decreasing the quality of the study. It is also challenging to identify clinically significant new findings in the postoperative hip.
Standard radiographic studies should include an AP pelvis, AP hip, and a lateral view of the hip (frog leg or cross table) [14]. These images should be scrutinized for pathology including cam and pincer impingement, hip arthritis, fracture, dysplasia, SI joint arthritis, and lumbar stenosis. Original imaging from before the initial surgery should be available for comparison.
MRI arthrogram should be the study of choice when evaluating for intra-articular soft tissue pathology in the postoperative hip. Blankenbaker et al. performed a retrospective review of 20 patients who had undergone revision arthroscopic hip surgery for recurrent labral tear after initially undergoing a labral debridement [15]. Original and postoperative MRI arthrograms, as well as surgical documentation of the revision procedure, were available for evaluation. All MRI arthrograms were obtained at the same institution using the same protocol. Two fellowship trained musculoskeletal radiologists reviewed the images retrospectively. Nineteen patients were diagnosed with recurrent labral tear intraoperatively. Fourteen tears were identified by consensus retrospective review on MRI arthrogram (12 based on high intensity line to the labral surface, two based on labral distortion and paralabral cyst formation). The other five patients were found to have only labral shortening. They concluded that a recurrent labral tear can be diagnosed on MRI arthrogram by the presence of a new high intensity line to the labral surface, an enlarged or distorted labrum, or a new paralabral cyst.
McCarthy and Glassner have shown the useful correlations between arthrography and arthroscopy in the revision setting [16]. We currently use a combination of MRI and MRI arthrogram to evaluate patients after hip arthroscopy when standard plain radiographs do not reveal the complete diagnosis. Figure 35.1 provides a summary of our most common uses for both studies.
Fig. 35.1
Surgical considerations for review of MRI and MRI arthrogram of the hip in the revision setting
Cases
Case 1: Postoperative Adhesions
History, Clinical Presentation, and Exam
A 32-year-old female presents for second opinion when she failed to have any significant relief after arthroscopic labral debridement and microfracture of a chondral defect 8 months prior. The operative note indicated that minimal labrum debridement in the anterior acetabulum was performed along with a femoral head microfracture procedure. The patient expressed that her initial complaint prior to index surgery was groin pain during and after physical activity for 6 months.
Her only period of significant relief after her first surgery was from an intra-articular steroid injection. Her rehabilitation protocol following the index procedure included crutch protection for 6 weeks. Physical therapeutic exercise was initiated at 8 weeks.
On physical exam, she had pain with flexion adduction internal rotation. She also had a decrease in arc of motion compared to her uninjured side. FABER testing and off the table extension testing reproduced pain. There was tenderness over the anterior hip capsule with no signs of infection and well-healed incisions.
Imaging
Plain radiographs showed no signs of residual femoroacetabular impingement or arthritic change. MRI arthrogram was obtained which demonstrated postoperative adhesions and loss of normal capsulolabral architecture and lacked any significant alternate pathology (see Fig. 35.2).
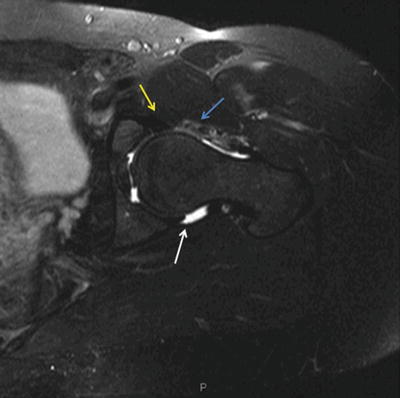
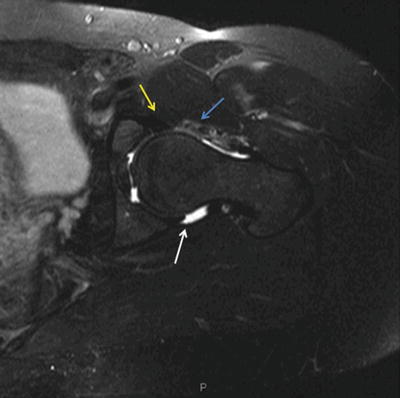
Fig. 35.2
Axial T2-weighted MRI arthrogram image demonstrating low signal interruption of the intra-articular contrast at the area of prior surgical exposure (blue arrow). Anteriorly, there is loss of the normal supraacetabular recess as evidenced by lack of contrast fill between the labrum and capsule (yellow arrow). Posteriorly, the normal supraacetabular recess contrast fill is demonstrated in the area distant from the prior surgical field (white arrow)
Treatment
After discussion of risks and benefits, the patient elected for revision hip arthroscopy. During arthroscopy, the labrum was found to be healed in the area of prior debridement, and no segmental loss was present. The supraacetabular space was obliterated with adhesions along the anterior labrum (Fig. 35.3). The area of prior capsulotomy scarred directly to the femoral head region of microfracture (Fig. 35.4). Operative treatment included mechanical and thermal lysis of adhesions and closure of the prior capsulotomy defect.
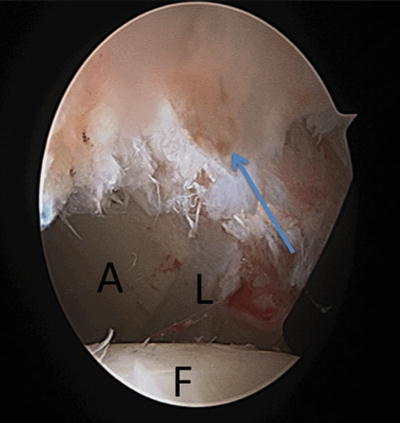
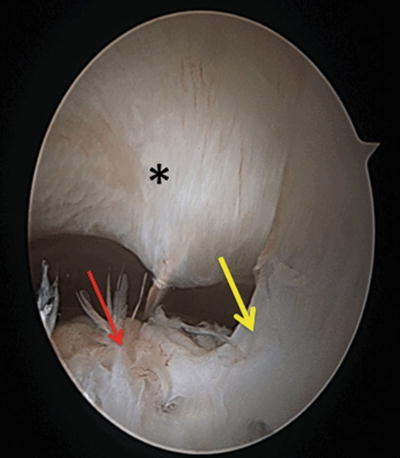
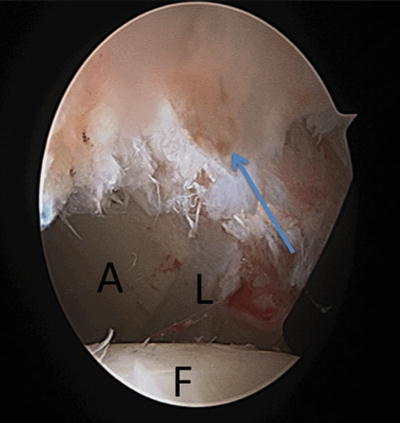
Fig. 35.3
Arthroscopic image corresponding with MRI arthrogram shown in Fig. 35.2 at the level of the acetabular rim. Adhesions obliterating supraacetabular recess (blue arrow) in postoperative zone. A acetabulum, F femoral head, and L labrum
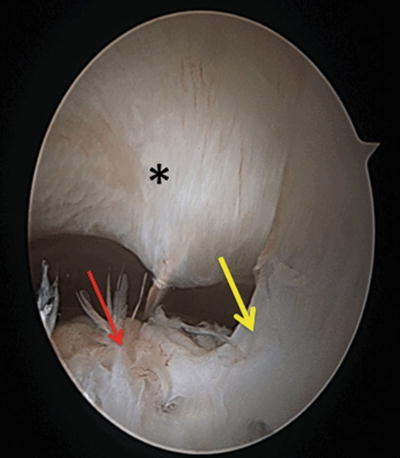
Fig. 35.4




Arthroscopic image in the peripheral space corresponding with MRI arthrogram shown at the level of the capsule-femoral head adhesion. Normal capsule (asterisk); adhesion (yellow area) sweeping from prior capsulotomy to femoral head at the area of prior microfracture (red arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








