Large volume tissue biopsies
Management of massive hemoptysis
Foreign body extraction
Direct management of endobronchial obstruction
Mechanical coring of lesion using beveled tip
Direct dilation of airway lumen
Indirect management of endobronchial obstruction
Nd:YAG laser
Argon plasma coagulation (APC)
Cryotherapy
Electrocautery
Bougie/balloon dilation
Microdebrider
Management of extrinsic/dynamic airway lumen compression
Silicone stent
Self-expandable stent
The lung cancer epidemic of the mid-twentieth century has made rigid bronchoscopy a vital skill when managing patients with advanced lung cancer. It is estimated that up to 20–40% of patients who suffer from lung cancer will experience an episode of mechanical airway obstruction. In cases of symptomatic airway compromise, the intervention should be rapid and effective with low associated morbidity and mortality. If performed as a staged procedure to establish a stable airway prior to more definitive surgical management, the endoscopic intervention should not interfere with the ultimate surgical plan. If the intervention is palliative, it should require limited follow-up care in an effort to maximize the positive impact on patient quality of life.
The rigid bronchoscope alone is an effective tool and satisfies the above goals.
There are numerous specific technical advantages to the rigid bronchoscope in comparison to the flexible bronchoscope that need to be emphasized, including large volume suction capability, direct airway control, greater therapeutic options, and stent placement (Table 27.2). It is important to remember that the flexible bronchoscope complements the rigid bronchoscope and should not replace it in the airway armamentarium.
Table 27.2
Advantages of the rigid bronchoscope
Large lumen accommodates variety of larger tools and devices |
Large suction capability |
Ventilating lumen minimizes airway obstruction |
Ability to deploy silicone and expandable stents |
Direct ability to manipulate lesions and achieve hemostasis |
Decreased risk of airway fire when using heat energy |
Direct airway control |
Direct ability to isolate right and left airway |
Well-supported oxygenation and ventilation throughout procedure |
Allows for prolonged procedures |
In order to provide multidimensional patient care, the therapeutic endoscopist of the twenty-first century needs to be facile in both the technology first conceived in the nineteenth century and that which was introduced in the twentieth century.
Equipment
The rigid bronchoscope is a powerful yet simple piece of equipment. The rigid bronchoscope acts as a conduit to the airway and accommodates a variety of tools: graspers, dilators, biopsy forceps, stent delivery devices, catheters, and suction devices. There are three main components of the rigid bronchoscope: the barrel, the multifunction head, and the optics and light source.
1.
The Barrel: There are two main varieties of rigid scopes: rigid bronchoscopes and rigid trachea scopes. Rigid bronchoscopes are longer permitting access to the right and left bronchial tree and have side ventilation fenestrations. The rigid trachea scope is shorter, has no side ventilation fenestrations, and cannot reach past the mid- to distal trachea (Fig. 27.1).


Fig. 27.1
Rigid bronchoscope and rigid tracheascope. The rigid bronchoscope is long and has side ventilating fenestrations at its distal end. The rigid trachea scope is shorter and has no side ventilating fenestrations
The rigid barrel is a hollow metallic tube with a beveled distal tip. The proximal end of the scope connects to the multifunction head permitting ventilation and instrument access. The light source attaches to the proximal end of the scope or to the telescope lens directly depending on the make and model. Rigid bronchoscopes are manufactured in various lengths ranging from 33 to 43 cm depending on type and manufacturer. Rigid scopes have both an inner and an outer diameter. The inner diameter of the adult rigid bronchoscope ranges from approximately 7–13 mm, and the outer diameter ranges from 8 to 14 mm depending on the specific scope and manufacturer. Scope size is a critical component of clinical decision making in therapeutic bronchoscopy. Larger scopes can accommodate large stents including Y stents and are excellent for addressing tracheal and proximal mainstem pathology. Smaller scopes can more easily navigate the distal left and right mainstem bronchi, and the bronchus intermedius but may be more limiting as a conduit for certain larger instruments and stents. Smaller scopes can be used serially to access and dilate tight stenosis, minimizing the risk of airway trauma caused by larger scope diameters.
2.
The Multifunction Head: The multifunction head attaches to the proximal portion of the barrel. The multifunction head (Fig. 27.2) has ports to accommodate ventilation and procedural instruments or suction simultaneously. The ventilation port can be attached to either volume ventilation or jet ventilation depending on one’s preference. The rigid bronchoscope is uncuffed, therefore a significant air leak may occur and the tidal volumes delivered will not reflect alveolar tidal volume. Furthermore, it may be difficult to assess end tidal CO2. Jet ventilation allows the operator to maintain an open circuit and freely introduce and remove instruments. Volume ventilation requires a fenestrated cap which must remain closed to ensure adequate ventilation.


Fig. 27.2
The multifunction head can be an independent piece which attaches to the rigid barrel or is a unified extension of the rigid barrel. The multifunction head allows for simultaneous ventilation and airway instrumentation
3.
Optics and Light Source: For intubation, the endoscopist can either use a telescope and camera to direct the rigid scope or direct visualization down the barrel with the naked eye using the light source built into the barrel (Fig. 27.3). Once the airway is secured, the bronchoscopist can deploy a telescope coupled to a camera, pass a flexible bronchoscope, or employ optical forceps which combine the telescopic camera and specialized graspers for visualization. Some endoscopists site directly down the barrel with the naked eye for instrument deployment. Only bronchoscopes with a built-in light source allow the endoscopist direct sight through the lumen of the scope.
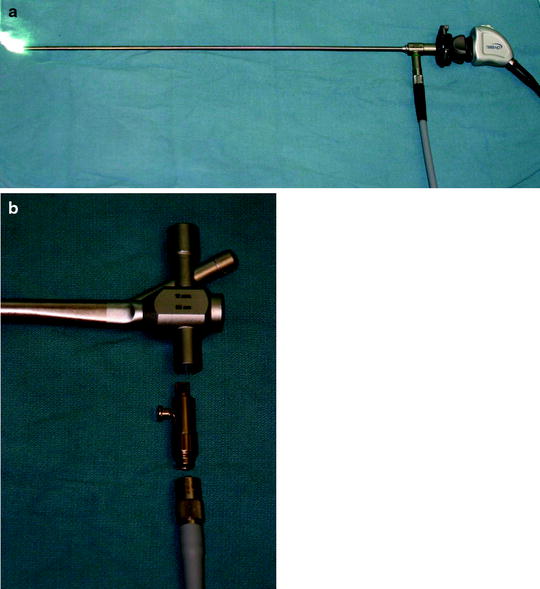
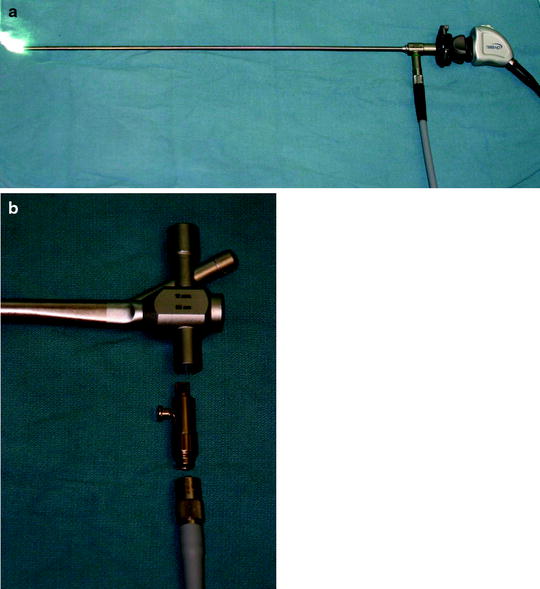
Fig. 27.3
(a) The bronchoscope light source can be attached to a video telescope displaying the image on a monitor. (b) The light source can be built into the multifunction head allowing the bronchoscopist to directly site down the barrel into the airway
Our practice routinely employs both rigid and flexible bronchoscopy concurrently for all procedures. The flexible bronchoscope can also be inserted to extend the endoscopy into the lobar and segmental levels, to inspect the airway beyond obstructing lesions or areas of bronchial distortion.
Tools and Accessories: Instruments have been designed to pass through the main working lumen or barrel of the bronchoscope. Principle accessories include suction catheters, graspers, biopsy forceps, dilators, cautery, stents, and other implements (Fig. 27.4). The common feature of instruments designed for the rigid bronchoscope is that they are larger and stiffer than those built for the working channel of the flexible bronchoscope.


Fig. 27.4
Rigid bronchoscope accessories for deployment down the barrel
Technique
Intubating the patient with the rigid bronchoscope requires appropriate sedation and proper patient positioning. Sedation and use of paralytics depends on the clinical stability of the patient, presence or absence of central mediastinal tumors, and careful communication between endoscopist and anesthesiologist.
The scopes’ rigid construction requires straight and direct access to the larynx. As with all intubations, the teeth are vulnerable, and a tooth guard should be placed to protect the upper teeth during the procedure. When proper technique is employed, there should be no pressure on the upper teeth or lip similar to direct laryngoscope intubation. The patient is positioned supine with either a towel roll under the shoulders or the head of the bed dropped allowing the neck to be maximally extended without floating. This maneuver elevates the larynx and creates a more linear route through the vocal cords. The goal is to achieve anterior linear alignment of the oral, pharyngeal, and laryngeal axis in order to access the trachea (Fig. 27.5).


Fig. 27.5
Patient position in preparation for rigid bronchoscopy intubation
Once the patient is positioned, the bronchoscope is used to directly intubate the trachea and advanced under direct visualization either sighting directly down the barrel or through the telescope and camera optics. It is critical to advance the scope under direct visualization to ensure midline position. If employing the telescope and camera technique, the telescope should always remain within the barrel of the scope with visualization of the distal scope tip at all times to minimize risk of airway injury (Fig. 27.6). The endoscopist uses their nondominant hand and the first finger to push the jaw down. The second finger rests on the roof of the patient’s mouth, and the thumb acts as a fulcrum supporting the scope. The scope, held in the dominant hand, is inserted into the oral cavity perpendicular (at a 90 ° angle) to the operating table. The first visualized structure is the uvula as the scope is advanced to the base of the tongue (Fig. 27.7). When the uvula comes into view, the hand supporting the scope drops using the thumb as a fulcrum, from a 90 ° angle to an approximately 45 ° angle. The scope is now advanced until the epiglottis comes into view (Fig. 27.8). Care is necessary to keep the scope pressure on the operators thumb near the mouth, rather than on the patient’s teeth. The scope is passed under the epiglottis, which is lifted directly anterior to expose the larynx and vocal cords. With the vocal cords visualized and open, the scope is rotated 90 ° to the right or left, so the bevel is parallel to the cords to minimize vocal cord trauma (Fig. 27.9). Once past the cords, the scope is advanced to the mid-trachea to ensure the distal lateral ventilation ports are well within the airway and the ventilating system can be attached to establish active ventilation.
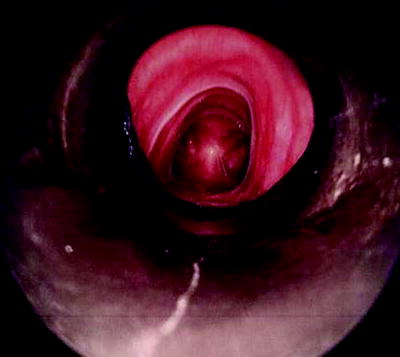
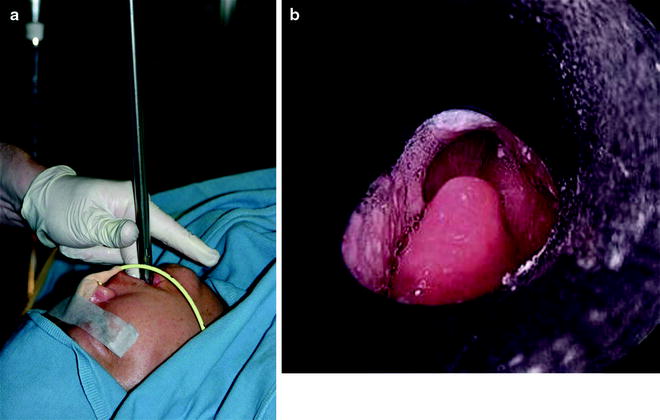
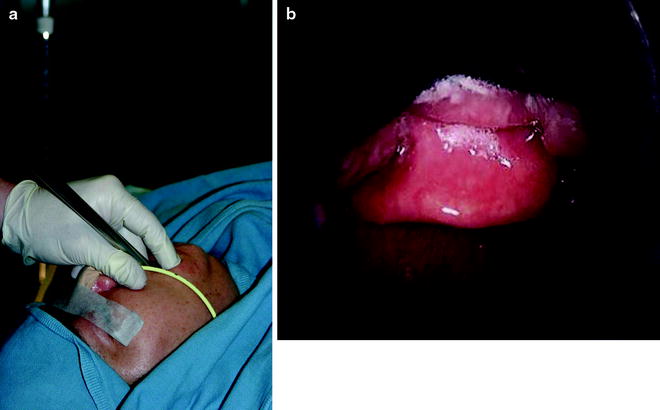




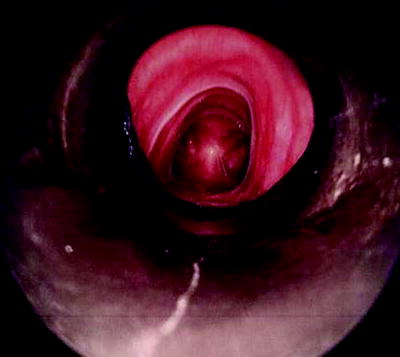
Fig. 27.6
View of the light source and telescope safely tucked in the rigid barrel. This is the view you should have of the distal tip when advancing the rigid bronchoscope
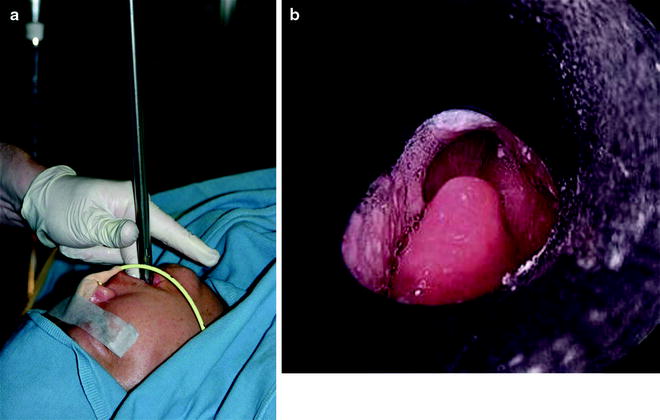
Fig. 27.7
(a) Initial position for rigid intubation. The scope is held perpendicular to the patient’s oral pharynx. (b) In this position, the first structure you should visualize is the uvula
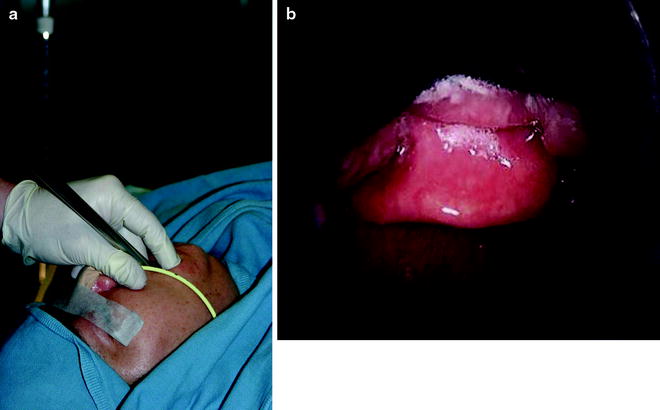
Fig. 27.8
(a) The second position for rigid intubation. The scope drops to a 45 ° angle. (b) In this position you should visualize the epiglottis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree