15 Ruling Out Fetal Anomalies In the first few weeks after conception, the embryo undergoes growth, morphogenesis, and differentiation of tissues and organs. This is termed the embryonic period and lasts until about 8 weeks gestational (menstrual) age. The remaining weeks of gestation are termed the fetal period, during which rapid growth occurs.1 Fetal anomalies most often result from abnormal morphogenesis or differentiation during the embryonic period. Ultrasound is the imaging modality of choice for evaluation of the fetal anatomy to assess for fetal anomalies. The fetus can be assessed from multiple angles in multiple planes to obtain the images required. The real-time capabilities of ultrasound permit evaluation even while the fetus is moving. In addition, real-time scanning allows identification of fetal cardiac activity before other means of assessment can document fetal life. Real-time is essential when assessing the fetal heart for structural or rhythmic abnormalities. Fetal anomalies occur in ~2.5% of newborn infants,2,2 and, in most cases, no prior history of a fetal malformation is present. There are, however, some conditions associated with increased risk of fetal anomaly, including a prior family history of congenital anomaly, maternal diabetes, advanced maternal age, and exposure to certain teratogens, drugs, or infections during pregnancy. Upon conception, signs associated with increased risk of fetal malformation include abnormal amniotic fluid volume, either polyhydramnios or oligohydramnios, abnormal maternal serum α-fetoprotein levels, and multiple gestations. Given any of these conditions, ultrasound is used to evaluate the developing fetus for an anomaly. The American College of Radiology, American College of Obstetrics and Gynecology, and the American Institute of Ultrasound in Medicine have published joint standards for antepartum obstetrical ultrasound that include a list of the fetal anatomical structures that should be evaluated when performing ultrasound during the second and third trimesters (Table 15–1).4 Although it is not possible to detect all fetal anomalies prenatally, if these standards are used for fetal evaluation, most major congenital malformations will be detected. In some cases, more specialized examinations may be required, whereas in other cases, a fetal anomaly may not be visible on prenatal ultrasound.
Head |
Lateral ventricles and choroid plexus |
Midline falx and cavum septum pellucidum |
Posterior fossa to include cerebellum and cisterna magna |
Heart |
Four-chamber view including its position in thorax |
Spine |
Cervical, thoracic, lumbar, and sacral |
Stomach |
Urinary bladder |
Umbilical cord insertion at anterior abdominal wall |
Kidneys |
Extremities |
Images taken for fetal measurements |
Biparietal diameter/head circumference |
Abdominal diameter/circumference |
Femur length |
aFrom: AIUM Practice Guideline for the Performance of an Antepartum Obstetric Ultrasound Examination. American Institute of Ultra-sound in Medicine; 2003. Published in conjunction with the American College of Obstetricians and Gynecologists (ACOG) and the American College of Radiology (ACR).
Ultrasound Evaluation
The Fetal Head
During an obstetrical ultrasound examination, three views of the fetal head are routinely obtained: the biparietal diameter, the cerebral ventricles, and the posterior fossa. The biparietal diameter view is an axial view of the fetal head at the level of the paired thalami and cavum septum pellucidum (Fig. 15–1). On this view, the presence of the head is confirmed and the cranial contour is assessed. The midline falx and cavum septum pellucidum are typically visible. The normal fetal head is oval in shape with a smooth contour.
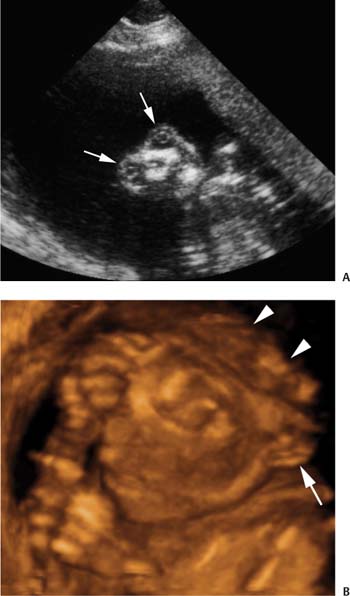
Anencephaly (Fig. 15–2) is a neural tube defect where the cranium and brain tissue are absent. The lower face is usually normally formed, but the forehead above the orbits and the cranium above the cervical spine are absent.
Figure 15–1 Image of the fetal head for the biparietal diameter measurement. Axial image at the level of the paired thalami (arrows) and the cavum septum pellucidum (arrowhead) is used for measurement of the biparietal diameter.
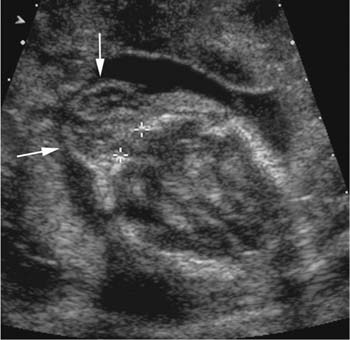
An encephalocele (Fig. 15–3) is a neural tube defect involving the cranium. These lesions are often identified on the biparietal diameter view. A defect in the skull is present, through which intracranial contents herniate outside the skull. Most encephaloceles are midline and posterior involving the occipital bone. Less common are frontal and parietal encephaloceles. Sonographically, the encephalocele defect appears as an interruption in the calvarium with a sac containing soft tissue and sometimes fluid protruding outside the skull.
Figure 15–2 Anencephaly. (A) Sonogram of fetal face with absence of forehead above the orbits (arrows). (B) Three-dimensional image of a fetal head demonstrating absence of the cranium above the ear (arrow). Dysplastic brain tissue is seen posterior to the face (arrowheads).
Figure 15–3 Encephalocele. Axial sonogram of fetal head demonstrating occipital defect (calipers) with brain tissue and meninges protruding outside the skull into the encephalocele (arrows).
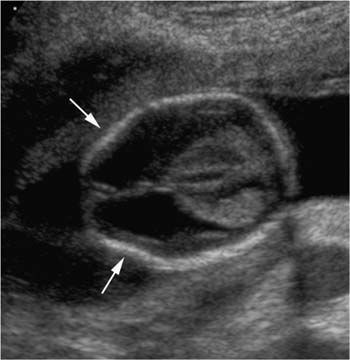
Flattening of the frontal bones in the second trimester, giving the appearance of a “lemon”-shaped head (Fig. 15–4) on the biparietal diameter view, is associated with meningomyeloceles. When this finding is present, the posterior fossa should be evaluated carefully for a Chiari II malformation, and the spine should be examined for spina bifida.5
Figure 15–4 “Lemon” sign. Axial view of the fetal head in a fetus with a meningomyelocele demonstrating flattening of the frontal bones (arrows) giving the head a lemon shape. There is associated hydrocephalus.
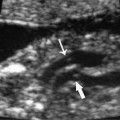
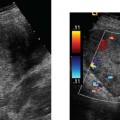
Evaluation of intracranial contents should include assessment of the lateral ventricles, the choroid plexus, and the posterior fossa. The lateral ventricles are evaluated on axial view to assess both the size and the shape of the ventricles. The width of the lateral ventricle is measured at the atrium of the lateral ventricle, perpendicular to the axis of the ventricle (Fig. 15–5), and should not exceed 10 mm. Excess cerebral spinal fluid in the head can be seen with dilatation of the lateral ventricles in such anomalies as hydrocephalus or agenesis of the corpus callosum. Excess fluid may also be a sign of an abnormal configuration of the ventricles, as in anomalies such as holoprosencephaly or porencephaly.
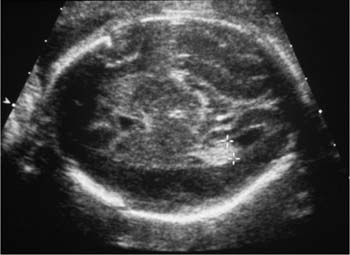
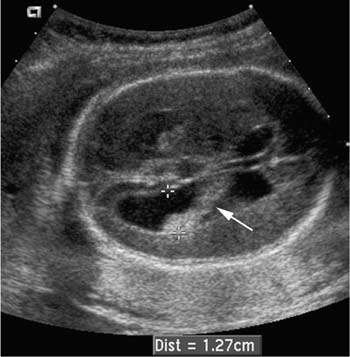
Hydrocephalus is defined as dilatation of the lateral ventricles. It may be an isolated anomaly, or it may result from in utero exposure to infection or a toxic agent, or it may be part of a syndrome or other complex congenital malformation. Hydrocephalus is commonly seen in association with meningomyeloceles and Dandy-Walker malformations. On ultrasound the diagnosis of hydrocephalus is made when the width of the lateral ventricle at the atrium measures more than 10 mm on axial view (Fig. 15–6),6 and the choroid plexus appears to dangle away from its mid-line attachment.7 If the lateral ventricles are dilated, then the third ventricle, located between the thalami on axial view, should be examined to look for dilatation. Aqueductal stenosis is a cause of hydrocephalus that leads to dilatation of the lateral and third ventricles with a normal fourth ventricle and posterior fossa.
Figure 15–5 Lateral ventricular measurement. Axial view of the fetal head demonstrating measurement of a normal lateral ventricle. The measurement is taken at the level of the atrium of the lateral ventricle (calipers).
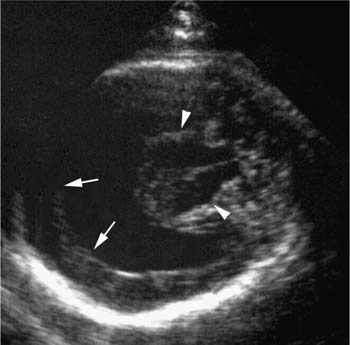
An abnormal configuration of the cerebral ventricles is seen with holoprosencephaly (Fig. 15–7), a developmental anomaly in which there is absence or incomplete cleavage of the prosencephalon. This malformation is characterized by fusion of the lateral ventricles into a single ventricle that communicates across the midline. The cerebral hemi-spheres are fused as well, and the falx is absent or rudimentary. This anomaly is often associated with abnormalities of the fetal face, including midline facial clefts, hypotelorism, a proboscis, and cyclops.3
Figure 15–6 Hydrocephalus. Axial sonogram of the fetal head showing a dilated lateral ventricle (calipers) with the choroid plexus dangling from its medial attachment (arrow).
Figure 15–7 Holoprosencephaly. Vaginal sonogram of the fetal head demonstrating a single cerebral ventricle between fused cerebral cortex (arrows) and fused thalami (arrowheads).
The choroid plexus is examined for its position in the lateral ventricle and for cysts. This is best done on the same view used to assess the cerebral ventricles. A dangling choroid plexus, where the posterior end of the choroid plexus is abnormally separated from the medial wall of the lateral ventricle, is seen with hydrocephalus. Choroid plexus cysts (Fig. 15–8) may be seen in the second trimester and are associated with increased risk for chromosomal abnormalities, especially trisomy 18.8 These cysts are round, anechoic, with thin, smooth walls. Sometimes in the early second trimester, the choroid plexus has a “spongy” appearance, containing lobular, hypoechoic areas. This is a normal finding that should not be confused with choroid plexus cysts.
Figure 15–8 Choroid plexus cyst. Axial image of the fetal head demonstrating a cyst (arrow) in the choroid plexus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree