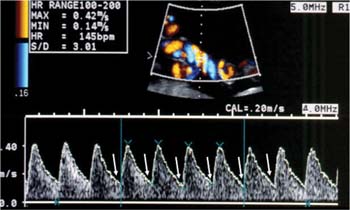
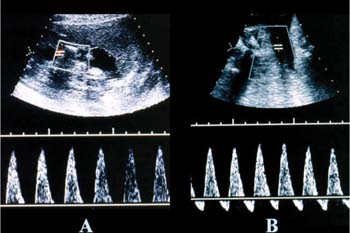
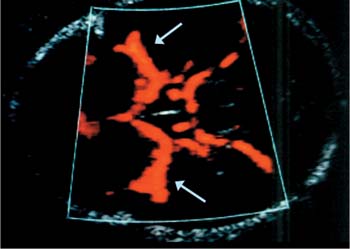
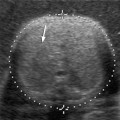
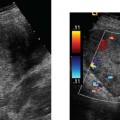
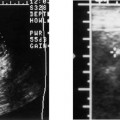
14 Uterine Size Less than Dates: A Clinical Dilemma Accurate pregnancy dating is the most important step in prenatal management. Precise knowledge of gestational age is essential for the management of high-risk pregnancies and, in particular, fetal growth restriction. Although uterine size, as measured by the fundal height, provides a subjective assessment of the fetal size, ultrasound plays an integral and more precise role in confirming gestational age and has been shown to have an accuracy of 3 to 4 days when performed between 14 and 22 weeks of gestation.1 Several definitions exist in the literature for the diagnosis of intrauterine growth restriction (IUGR). The definition that is most commonly used in clinical practice is an estimated fetal weight at less than the 10th percentile for gestational age. At this diagnostic threshold, ~70% of fetuses will be small for gestational age (constitutionally small) and have no increase in perinatal morbidity or mortality.2Using the fifth percentile as a cutoff for the diagnosis of IUGR may be more clinically applicable, given that perinatal morbidity and mortality have been shown to increase beyond this threshold.3 Of all the ultrasound-derived bio-metric parameters, the abdominal circumference is the most sensitive indicator for growth restriction in the fetus. An abdominal circumference of less than the 2.5th percentile for gestational age carries a sensitivity of greater than 95% for the diagnosis of IUGR.4,2 The growth profile of the abdominal circumference should therefore be monitored closely in fetuses at risk for growth abnormalities. Furthermore, when estimating fetal weights by ultra-sound, the appropriate growth curves should be used. Curves generated at high altitudes will underestimate IUGR by ~50% for sea-level populations.6 When compared with appropriately grown fetuses matched for gestational age, IUGR fetuses have an increased risk of perinatal morbidity and mortality.7 Long-term follow-up studies have shown an increased incidence of physical handicap and neurodevelopmental delay in growth-restricted fetuses.8,2 The presence of chronic metabolic acidemia in utero, rather than actual birth weight, appears to be the best predictor of long-term neurodevelopmental delay.10 In pregnancies with growth-restricted fetuses, timing of the delivery is the most critical step in clinical management. Balancing the risk of prematurity with the risk of long-term neurodevelopmental delay is a serious challenge facing physicians involved in the care of these pregnancies. Traditionally, the management of pregnancies with fetal growth restriction relied on cardiotocography for fetal surveillance. During cardiotocography, the physician looks for heart rate variability as a sign of fetal well-being. Heart rate variability is the final result of the rhythmic, integrated activity of autonomic neurons generated by organized cardiorespiratory reflexes.11 In growth-restricted fetuses, higher baseline rates, decreased long- and short-term variability, and delayed maturation of reactivity are seen in heart rate tracings.12,2 These studies have relied on computer-generated analyses of fetal heart rate tracings in their evaluation. Unaided visual analyses of fetal heart rate records show limited reliability and reproducibility.14,2 Furthermore, the presence of overtly abnormal patterns of fetal heart rate tracings represents late signs of fetal deterioration.16,2 Relying on unaided visual analysis of cardiotocography as the only test of fetal surveillance in growth-restricted fetuses has come under criticism recently because it represents late signs of fetal deterioration and thus its sole use may not optimize long-term outcome of these pregnancies. Doppler ultrasound has been shown to improve outcome in high-risk pregnancies.18 The use of Doppler ultra-sound in the management of pregnancies with fetal growth restriction has received significant attention in the recent literature. Several cross-sectional and longitudinal studies have highlighted the fetal cardiovascular adaptation to hypoxemia and the progressive stages of such adaptation.19–24 Findings from these studies and the use of Doppler ultrasound in the management of the growth-restricted fetus are discussed in the following section. The umbilical arterial circulation is normally a low impedance circulation (Fig. 14–1) with an increase in the amount of end diastolic flow with advancing gestation.25 Umbilical arterial Doppler waveforms reflect the status of the placental circulation, and the increase in end diastolic flow that is seen with advancing gestation is a direct result of an increase in the number of tertiary stem villi that takes place with placental maturation.26 Diseases that obliterate small muscular arteries in placental tertiary stem villi result in a progressive decrease in end-diastolic flow in the umbilical arterial Doppler waveforms until absent and then reverse flow during diastole is noted27 (Fig. 14–2). Reversed diastolic flow in the umbilical arterial circulation represents an advanced stage of placental compromise and is associated with more than 70% of placental arterial obliteration.28,2 The presence of absent or reversed end diastolic flow in the umbilical artery is commonly associated with severe intrauterine growth restriction and oligohydramnios.30 Figure 14–1 Normal Doppler waveforms obtained from the umbilical artery in the third trimester. In the third trimester of pregnancy, the umbilical circulation is a low impedance circulation. Note the increased amount of flow at end diastole (white arrows). Figure 14–2 (A) Absent end-diastolic velocity and (B) reversed enddiastolic velocity are noted in the umbilical circulation when the downstream impedance is increased. These Doppler waveforms are associated with significant fetal compromise. Doppler waveforms of the umbilical arteries can be obtained from any segment along the umbilical cord. Waveforms obtained from the placental end of the cord show more end diastolic flow than waveforms obtained from the abdominal cord insertion.31 Differences in Doppler indices of arterial waveforms obtained from different anatomical locations of the same umbilical cord are generally minor and have no significance on clinical practice.25 The cerebral circulation is normally a high impedance circulation with continuous forward flow throughout the cardiac cycle.32 The middle cerebral artery is the most accessible cerebral vessel to ultrasound imaging in the fetus and it carries more than 80% of cerebral blood flow.33 In the presence of fetal hypoxemia, central redistribution of blood flow occurs, resulting in increased blood flow to the brain, heart, and adrenals and a reduction in flow to the peripheral and placental circulations. This blood flow redistribution is known as the brain-sparing reflex and plays a major role in fetal adaptation to oxygen deprivation.32,2 The right and left middle cerebral arteries represent major branches of the circle of Willis in the fetal brain. The circle of Willis, which is supplied by the internal carotids and vertebral arteries, can be imaged with color flow Doppler ultrasound in a transverse plane of the fetal head obtained at the base of the skull. In this transverse plane, the proximal and distal middle cerebral arteries are seen in their longitudinal view, with their course almost parallel to the ultrasound beam (Fig. 14–3). Middle cerebral artery Doppler waveforms, obtained from the proximal portion of the vessel, immediately after its origin from the circle of Willis, have shown the best reproducibility.35 Figure 14–3 Axial view of the fetal head in the second trimester with color Doppler showing the circulation at the level of the circle of Willis. Note the course of the middle cerebral arteries, almost parallel to the ultrasound beam (white arrows).
Ultrasound Evaluation
Fetal Arterial Doppler Ultrasound of the Umbilical Circulation
Fetal Arterial Doppler Ultrasound of the Middle Cerebral Circulation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree