Chapter 8 Sacroiliac Intraarticular Joint Injections, Posterior Approach, Inferior Entry
The exact innervation of the sacroiliac joint remains under debate. Some authors have suggested that the joint is innervated both posteriorly and anteriorly;3,4 however, others argue that the innervation is exclusively posterior from the lateral branches of the sacral dorsal rami.5,6
The diagnosis of SIJ pain is made by clinical suspicion with the use of the history and physical examination and can be supported by diagnostic intraarticular injections. To date, there are no reliable imaging studies or physical examination maneuvers to accurately diagnose SIJ dysfunction.2
Because of the potential for capsular defects in the sacroiliac joint, the sensitivity and specificity of intraarticular blocks has been called into question.7,8 The interosseus or dorsal sacral ligaments, both potential pain generators, are not blocked through intraarticular injection. Studies have shown that while multisite, multidepth sacral lateral branch blocks do not block the intraarticular joint, they are potentially useful tool to evaluate extraarticular SIJ pain.11
Note: Please see page ii for a list of anatomical terms/abbreviations used in this book.
 Trajectory View
Trajectory View
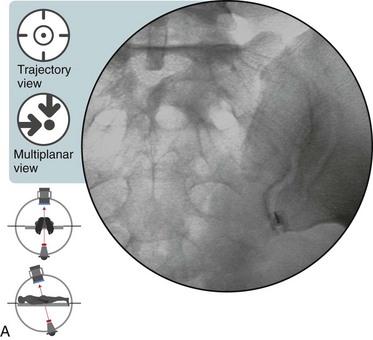
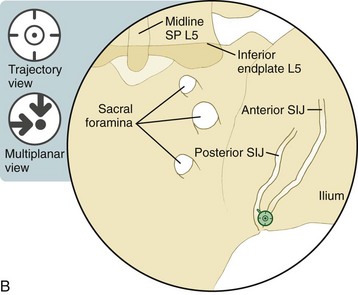
 Oblique the fluoroscope, starting with 5–10 degrees of ipsilateral oblique.
Oblique the fluoroscope, starting with 5–10 degrees of ipsilateral oblique.
 Under live fluoroscopy, move the C-arm to 10–20 degrees contralateral oblique.
Under live fluoroscopy, move the C-arm to 10–20 degrees contralateral oblique.
 Watch for the optimal “hyperlucent” region at the inferior portion of the SIJ.
Watch for the optimal “hyperlucent” region at the inferior portion of the SIJ.
 The target needle destination is the inferior aspect of the medial joint space; this corresponds with the posterior aspect of the SIJ.
The target needle destination is the inferior aspect of the medial joint space; this corresponds with the posterior aspect of the SIJ.The Trajectory View Is Also a Multiplanar View
![]() Notes on Positioning in the Trajectory View
Notes on Positioning in the Trajectory View
 The needle is introduced into the medial aspect of the sacroiliac joint 1 to 2 cm superior to the inferior aspect of the joint.
The needle is introduced into the medial aspect of the sacroiliac joint 1 to 2 cm superior to the inferior aspect of the joint.
 The needle is advanced in this position until it is felt to be firmly placed within the joint. If the periosteum is encountered, the needle should be rotated while gentle pressure is used to facilitate further advancement into the joint.
The needle is advanced in this position until it is felt to be firmly placed within the joint. If the periosteum is encountered, the needle should be rotated while gentle pressure is used to facilitate further advancement into the joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree