Sarcoidosis is a systemic disorder of unknown cause, characterized by the presence of noncaseating granulomas. It may involve almost any organ, but most morbidity and mortality result from pulmonary disease. Pulmonary manifestations are present in 90% of patients. Approximately 25% of patients have respiratory symptoms at diagnosis, usually dyspnea; also common are weight loss, fatigue, and sometimes fever or night sweats. Erythema nodosum is common.
Pulmonary lesions may resolve spontaneously or progress to fibrosis; 20% to 25% of patients have permanent functional impairment. Hilar and mediastinal lymph node enlargement is a common finding.
STAGING OF SARCOIDOSIS BASED ON PLAIN RADIOGRAPHS
Sarcoidosis has been described as occurring in stages based on plain radiographic findings:
Stage 0: No visible abnormalities (10% of cases)
Stage 1: Hilar or mediastinal lymph node enlargement not associated with visible lung disease (50% of cases)
Stage 2: Hilar or mediastinal lymph node enlargement associated with visible lung disease (30% of cases)
Stage 3: Diffuse lung disease without lymph node enlargement (10% of cases)
Stage 4: This designation is sometimes used to refer to endstage fibrosis.
The utility of this staging system is limited, although there is some correlation between the stage and the course of disease. Radiographic abnormalities resolve in 65% of stage 1 patients, 50% of stage 2 patients, and 20% of stage 3 patients. However, patients in one stage need not progress to the next. This staging system is not used with CT, which is much more sensitive than radiographs in detecting both lymph node enlargement and lung disease.
LYMPH NODE ABNORMALITIES
Mediastinal lymph node enlargement is very common with sarcoidosis, occurring in 60% to 90% of patients at some stage in their disease. Less than half of patients with lymph node enlargement also show findings of lung disease on plain radiographs. A greater percentage of patients with lymph node enlargement show evidence of lung disease on CT.
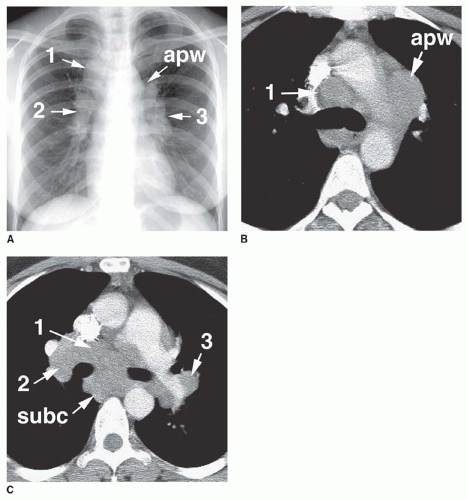
Typically, node enlargement involves the hilar and mediastinal nodes, and lymph node masses usually appear bilateral and symmetrical on chest radiographs. The combination of (1) right paratracheal, (2) right hilar, and (3) left hilar node enlargement, termed the 1-2-3 pattern, is typical of sarcoidosis (
Fig. 15-1; see also
Figs. 8-44 and
8-45 in
Chapter 8). Aortopulmonary window lymph node enlargement may also be seen, a finding sometimes referred to as the 1-2-3-4 pattern (see
Fig. 15-1A).
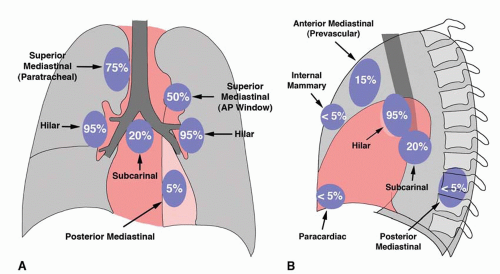
In patients with enlarged nodes, chest radiographs show abnormalities, in order of decreasing frequency, in the hila (85% to 95%), right paratracheal region (75%), aortopulmonary window (50% to 75%), subcarinal space (20%), and anterior mediastinum (10% to 15%;
Fig. 15-2;
Table 8-20). The presence of hilar lymph node enlargement is so typical of sarcoidosis that the absence of this finding in a patient with mediastinal lymphadenopathy should lead you to question the diagnosis. Enlarged internal mammary, paravertebral, and retrocrural lymph nodes can also be seen but are much less common. Unilateral hilar lymph node enlargement is seen in less than 5% of cases. Lymph nodes may show dense, stippled, or eggshell calcification.
On CT, lymph node enlargement is visible in more than 80% of patients with sarcoidosis, with most showing both hilar and mediastinal lymph node enlargement (see
Fig. 15-1B,C; see also
Figs. 8-44 and
8-45 in
Chapter 8). The frequency of visible involvement of specific node groups is somewhat different on CT, as compared to plain radiographs. Specifically, hilar lymph node enlargement is not invariably seen on CT in patients with mediastinal adenopathy. In patients with enlarged nodes, CT shows abnormalities, in order of decreasing frequency, in the right paratracheal space (100%), aortopulmonary window (95%), hila (90%), subcarinal space (65%), prevascular space (50%), and posterior mediastinum (15%). Symmetry, or bilateral node involvement, is visible more often on CT than on radiographs.
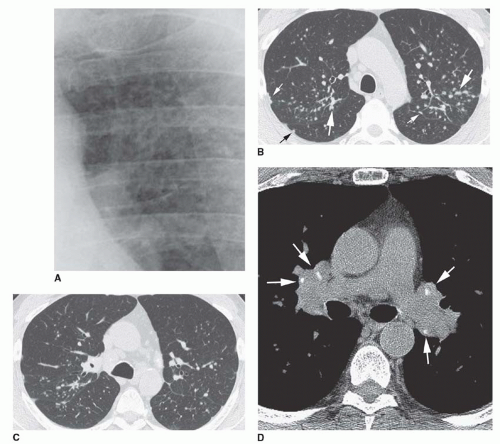
Lymph node masses in sarcoidosis may be quite large. Lymph node calcification is visible on CT in 25% to 50% of cases and may be hazy or dense or show a stippled or eggshell
appearance (
Fig. 15-3D; see also
Figs. 8-38A and
8-45 in
Chapter 8). Rarely nodes appear necrotic or low in attenuation or enhance on CT.