Second and Third Trimester Pregnancy
QUESTIONS
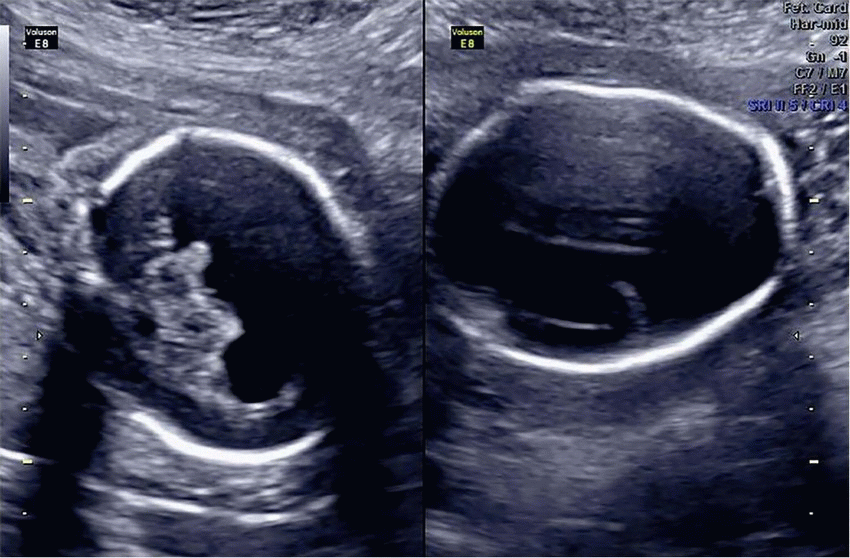
1a A 26-year-old pregnant female with gestational diabetes presents for fetal ultrasound screening. The patient underwent ultrasound at 13 weeks of gestational age followed by fetal ultrasound and fetal MRI at 22 weeks of gestational age.
|
Which of the following is the most likely diagnosis?
A. Hydranencephaly
B. Severe hydrocephalus
C. Alobar holoprosencephaly
D. Acrania
View Answer
1a Answer C. The fetal US and MRI images show a single central ventricle and fused thalami. No falx or interhemispheric fissure is present. These imaging findings are consistent with alobar holoprosencephaly, which is the most severe form of holoprosencephaly. In alobar holoprosencephaly, there is complete lack of separation of the cerebral hemispheres with a large posterior monoventricle. Single midline structures such as the falx, interhemispheric fissure, septum pellucidum, and corpus callosum are absent whereas paired midline structures such as the thalami and basal ganglia are fused.
Holoprosencephaly is a spectrum of congenital abnormalities ranging from incomplete formation of the falx cerebri and interhemispheric fissure to a complete lack of separation of the cerebral hemispheres with a large monoventricle. The three types of holoprosencephaly are alobar (most severe), semilobar, and lobar (least severe). Septooptic dysplasia is considered the mildest form of lobar holoprosencephaly.
In severe fetal hydrocephalus (choice B), the ventricles are severely dilated, but a thin rim of preserved cortical tissue is present peripherally. Also, the middle cerebral arteries are preserved in severe fetal hydrocephalus.
In hydranencephaly (choice A), the cerebral hemispheres of the brain are absent and replaced by sacs filled with cerebrospinal fluid. An incomplete or complete falx is present. Hydranencephaly is believed to result from occlusion of the middle cerebral or internal carotid arteries. Usually the cerebellum and brainstem are formed normally because the posterior circulation is not affected.
Acrania (choice D) is a rare lethal congenital anomaly characterized by an absence of the calvarium.
1b What midline facial abnormality is associated with alobar holoprosencephaly?
A. Hypertelorism
B. Frontal bossing
C. Metopic craniosynostosis
D. Cleft palate and lip
View Answer
1b Answer D. The midline facial abnormalities associated with alobar holoprosencephaly are cyclopia (single midline eye with failed development of nose with or without a proboscis), ethmocephaly (small narrow-set eyes with absence of nose), cebocephaly (small narrow-set eyes with a flattened nose and one nostril), cleft palate and lip, and solitary maxillary central incisor.
Facial and calvarial abnormalities help predict the severity of the brain malformation. Therefore, the presence of facial anomalies should trigger careful search for brain anomalies. “The face predicts the brain.”
References: Barkovich AJ. Congenital malformations of the brain and skull. In: Barkovich AJ (ed). Pediatric neuroimaging, 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2005:291-439.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:362.
Winter TC. Diagnostic imaging: obstetrics, 2nd ed. Lippincott Williams & Wilkins, 2011:1-2.
2a A primigravida is referred at 22 weeks of gestational age for follow-up of prior abnormal prenatal ultrasound findings and elevated maternal alpha fetoprotein (1,500 ng/mL).
|
What additional fetal anatomic imaging should be performed?
A. Fetal heart
B. Fetal brain
C. Fetal GU tract
D. Fetal GI tract
View Answer
2a Answer B. The first image is a sagittal view of the fetal spine showing an open spinal dysraphism or neural tube defect from the L2 to S1 levels. The second image is a coronal view of the lumbosacral neural tube defect with fluid sac containing spinal elements. These findings are concerning for myelomeningocele. Because almost all fetuses with an open spinal neural tube defect are found to have Chiari II malformation, further imaging of the fetal brain is recommended.
2b Additional images from anatomic imaging of the fetal brain are provided.
|
What is the most likely diagnosis?
A. Meckel-Gruber syndrome
B. Dandy-Walker sequence
C. Down syndrome
D. Chiari II malformation
View Answer
2b Answer D. Axial views of the fetal head demonstrate a small posterior fossa, indentation of the frontal bones, and enlarged lateral ventricles. (Fetal ventriculomegaly is defined as >10 mm width across the atria of the posterior or anterior horn of lateral ventricles at any gestational age. The lateral ventricles in this example measure 12.1 and 12.8 mm, respectively, which is considered moderate ventriculomegaly).
Chiari II malformation (also known as Arnold-Chiari malformation), is a congenital malformation of the spine and posterior fossa. It is characterized by myelomeningocele, small posterior fossa with descent of the brainstem and cerebellar tonsils, and ventriculomegaly. It is essential to obtain sagittal and transverse views of the fetal spine on antenatal imaging to evaluate for neural tube defects.
Sonographic findings seen in Chiari II malformation include the lemon sign and the banana cerebellum sign. The lemon sign is the indentation/concave deformity of the frontal bones. The banana cerebellum sign describes the abnormal curved shape of the cerebellar hemispheres that is caused by obliteration of the cisterna magna due to downward shifting of the posterior fossa structures.
Meckel-Gruber syndrome (choice A) is a lethal autosomal recessive disorder characterized by cystic dysplastic kidneys, occipital encephalocele, and postaxial polydactyly. In Dandy-Walker malformation (choice B), the fourth ventricle is dilated and communicates with the cisterna magna. The posterior fossa is enlarged, and the tentorium is elevated. The major congenital anomalies in Down syndrome/Trisomy 21 (choice C) include ventriculoseptal defect, atrioventricular septal defects, duodenal atresia, and ventriculomegaly.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:375-377.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:1133, 1257, 1365.
Woodward PJ. Diagnostic Imaging: Obstetrics, 2nd ed. Salt Lake City, UT: Amirsys, 2011.
3a Prenatal ultrasound evaluation of a 29-week-old fetus was performed. The following images were obtained at the level of the fetal chest and heart.
|
What cardiac chambers is the soft tissue mass occupying?
A. Right atrium and right ventricle
B. Left atrium and left ventricle
C. Right atrium and left ventricle
D. Left atrium and right ventricle
View Answer
3a Answer B. The axial images at the level of the fetal chest (4-chamber heart views) demonstrate rounded, echogenic soft tissue masses occupying the left atrium and left ventricle (the most posterior chamber of a normal fetal heart is the left atrium). The calipers in the second image correspond to a pericardial effusion.
The three most common fetal cardiac masses are rhabdomyoma (58%), teratoma (19%), and fibroma (12%). Rhabdomyoma is a benign myocardial tumor (hamartoma). Most of these tumors are diagnosed before the age of 1 year and are often multiple. In most cases, these lesions regress spontaneously and no treatment is required. Hemodynamically significant lesions can result in congestive heart failure, hydrops, pericardial effusion, and arrhythmias by obstructing outflow tracts or AV valves. They respond well to surgical excision.
3b Which of the following is most likely to be associated with this cardiac mass?
A. Down syndrome
B. Neurofibromatosis type 2
C. von Hippel-Lindau
D. Tuberous sclerosis
View Answer
3b Answer D. There is well-known association of cardiac rhabdomyomas with tuberous sclerosis. Greater than 50% of patients with cardiac rhabdomyomas are found to have tuberous sclerosis. Although tuberous sclerosis has many other manifestations in adult patients, they are rare in fetal life, except for subependymal tubers in the brain.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:397.
Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:1317-1318.
Woodward PJ. Diagnostic Imaging: Obstetrics, 2nd ed. Salt Lake City, UT: Amirsys, 2011.
4 A 21-year-old female presents for prenatal ultrasound at 26 weeks and 3 days of gestational age. Which of the following features is most useful in distinguishing this entity from other congenital lung masses?
|
A. Blood supply from systemic artery
B. Blood supply from pulmonary artery
C. Presence of mediastinal shift
D. Absence of mediastinal shift
View Answer
4 Answer A. Ultrasound images show a hyperechoic, wedge-shaped, solid mass, near the base of the left lung. Doppler interrogation demonstrates an artery arising from the aorta and supplying blood flow to the mass. These imaging findings are most consistent with a bronchopulmonary sequestration.
Bronchopulmonary (BP) sequestration is a congenital lung malformation in which nonfunctioning lung tissue is present without communication to the tracheobronchial tree. Bronchopulmonary sequestrations receive vascular supply from a systemic artery arising either from the thoracic or abdominal aorta. The two main types of bronchopulmonary sequestrations are intralobar and extralobar. Intralobar sequestration shares pleura with the normal lung, and extralobar sequestration is covered by its own separate pleura. Sequestrations are often found in the lower lobes and are more common on the left.
Bronchopulmonary sequestrations are not supplied by pulmonary artery (choice B). Any large chest mass, including a large BP sequestration, can result in mediastinal shift. The presence or absence of this finding does not aid in distinguishing it from other lesions (choices C and D).
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:404.
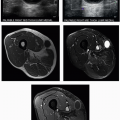
5a Below are images from fetal ultrasound at 18 weeks and MRI at 22 weeks of gestational age. Postnatal radiograph of the neonatal chest and abdomen is also provided.
Morbidity and mortality for this neonate is most likely dependent on which of the following?
A. Congenital heart disease
B. Pulmonary hypoplasia
C. Bowel obstruction
D. Urinary tract obstruction
View Answer
5a Answer B. Ultrasound images of the fetal thorax at 18 weeks of gestational age show echogenic contents in the left hemithorax with mediastinal shift to the right. MRI of the fetus in the coronal plane at 22 weeks demonstrates multiple fluid-filled bowel loops within the left hemithorax with shift of the heart and mediastinum to the right. Postnatal radiography of the chest and abdomen demonstrates airfilled bowel loops in the left hemithorax with shift of the heart and mediastinum to the right. These imaging findings are consistent with left-sided congenital diaphragmatic hernia (CDH).
The herniated bowel loops cause mass effect on the developing lung resulting in pulmonary hypoplasia, which is the main cause of morbidity and mortality in these patients. Such neonates are hypoxic and have persistent fetal circulation due to pulmonary hypoplasia and pulmonary hypertension.
|
5b Which of the following is an appropriate indication for performing a fetal MRI exam?
A. Surveillance of fetal renal pelviectasis
B. Quantification of amniotic fluid volume
C. Assessment for pulmonary hypoplasia
D. Assessment for fetal hydrops
View Answer
5b Answer C. Choice C, “Assessment for pulmonary hypoplasia” is the best answer because MR-derived fetal lung volumes will provide unique information which can help direct management decisions. The other options are not appropriate indications for MRI because the information can be obtained with US. According to the ACR-SPR Practice Parameter for the Safe and Optimal Performance of Fetal Magnetic Resonance Imaging (MRI) published in 2015, fetal MRI is indicated in the following situations:
When an abnormality on ultrasound is not clearly defined and more information is sought in order to make a decision about therapy, delivery, or to advise a family about prognosis. Example: a potential anomaly in the setting of maternal obesity, oligohydramnios, or advanced gestational age.
When an abnormality is identified on ultrasonography and the treating physician desires MR-specific information in order to make decisions about care. Example: calculation of MR-derived fetal lung volumes in cases of congenital diaphragmatic hernia.
When a fetus is significantly at risk for abnormality that will affect prognosis even if no finding is discovered with ultrasound. Example: neurologic ischemia after laser ablation of placental anastomoses in twin-to-twin transfusion syndrome.
References: American College of Radiology. ACR-SPR Practice Parameter for the Safe and Optimal Performance of Fetal Magnetic Resonance Imaging (MRI). Philadelphia, PA: ACR, 2015.
Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:400-402.
6 Increasing power output during a fetal ultrasound would be appropriate for which of the following situations?
A. Use of a 12 MHz linear probe fails to visualize all of the fetal anatomy because of insufficient acoustic penetration.
B. Multiple horizontal echoes are noted within the amniotic fluid close to the probe.
C. Insufficient acoustic penetration prevents complete evaluation of the fetus. The lowest frequency probe is being used and the gain has been maximized.
D. To decrease the potential bioeffects.
View Answer
6 Answer C. In order to minimize the risk of potential bioeffects from ultrasound, power output and examination time should be minimized as much as possible. Power output determines the amplitude of the acoustic energy transmitted by the probe. Probe transmit frequency needs to be selected to optimize tissue penetration, and gain settings must be optimized before increasing power.
Parallel echoes seen within anechoic structures near the probe represent reverberation artifact. Reverberation artifact occurs when the beam encounters a highly reflective surface and reflects multiple times between the surface and the probe face, creating a number of artifactual parallel echoes deep to the original reflector.
Reference: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:10-13.
7 Which of the following maneuvers can improve signal without causing an increase in temperature in fetal tissue?
A. Increasing dwell time
B. Increasing power output
C. Increasing gain
D. Switching from B-mode to color Doppler
View Answer
7 Answer C. Increasing receiver gain improves signal without any effect on the output of the outgoing ultrasound beam. Therefore, it will not cause increase in temperature and is safe to manipulate.
Dwell time (choice A) is the actual scanning time/duration of exposure. The risk of tissue heating is increased with the dwell time. Increasing power output (choice B) will result in higher exposure of the patient to ultrasound energy. Temperature elevations become progressively greater from B-mode to color Doppler to spectral Doppler applications (choice D).
Reference: Rumack CM, Wilson SR, Charboneau WJ. Diagnostic ultrasound, 4th ed. Philadelphia, PA: Elsevier Health Sciences, 2011:41.
8a A 42-year-old female presents at 28 weeks of gestation with shortened cervix and multiple fetal anomalies diagnosed at an outside facility. Fetal ultrasound at the level of the stomach is shown.
|
Which of the following syndromes is associated with this abnormality?
A. Tuberous sclerosis
B. Neurofibromatosis type 1
C. Trisomy 21
D. Trisomy 13
View Answer
8a Answer C. Fetal ultrasound shows dilated stomach in the left upper abdomen and dilated duodenal bulb in the right mid abdomen consistent with a double-bubble sign. It is important to show communication between the two fluid-filled structures to confirm that they are in fact the stomach and duodenum. The presence of this finding should raise concern for duodenal atresia. Polyhydramnios is also frequently seen in fetuses with duodenal atresia.
Approximately one-third of fetuses with duodenal atresia have trisomy 21. Therefore, when the double-bubble sign is encountered, a detailed scan should be performed to evaluate for other sonographic markers of trisomy 21.
The other answer choices including tuberous sclerosis, neurofibromatosis type 1, and trisomy 13 may have gastrointestinal manifestations after birth. However, the presence of a double-bubble sign in utero due to duodenal atresia is unique to trisomy 21 (Down syndrome) and VACTERL (vertebral defects, anal atresia, cardiac defects, tracheoesophageal fistula, renal anomalies, and limb abnormalities) sequence.
8b The fetus was delivered by emergent C-section at 33 weeks because of nonreassuring fetal heart tracing. Abdominal radiograph on the first day of life is shown.
|
Which of the following is the appropriate definitive management for this patient?
A. Surgical repair
B. Gastric decompression
C. Parenteral nutrition
D. Medical therapy
View Answer
8b Answer A. Abdominal radiograph of the neonate shows dilated stomach and duodenal bulb along with lack of distal bowel gas. If the neonate presents with bilious emesis and decompressed stomach on abdominal radiograph, an upper GI contrast study may be needed to exclude malrotation with volvulus.
The definitive treatment for infants with duodenal atresia is surgery, with duodenoduodenostomy being the procedure of choice. Gastric decompression and parenteral nutrition may be required to stabilize the infant prior to surgery.
References: Hertzberg BS, Middleton WD. Ultrasound: the requisites, 3rd ed. Philadelphia, PA: Elsevier, 2016:408-411.
Juang D, Snyder CL. Neonatal bowel obstruction. Surg Clin North Am 2012;92(3):685-711.
9 Which of the following ultrasound modes has the highest thermal index and therefore should be avoided or used in moderation when imaging the embryo or fetus?
A. 3D/4D
B. Color/spectral Doppler
C. M-mode Doppler
D. Gray-scale cine
View Answer
9 Answer B. Absorption of sound waves may cause heating in tissue. The thermal index (TI) is a measure of an ultrasound beam’s thermal bioeffects. It provides an indication of the relative potential for increasing tissue temperature, but it is not meant to provide the actual temperature rise. It is often displayed on ultrasound screens, along with the mechanical index.
Temperature elevations become progressively greater from B-mode to color Doppler to spectral Doppler applications. Color and spectral Doppler imaging uses increased levels of ultrasound output power. Therefore, the use of color and spectral Doppler is discouraged when imaging an embryo.
Reference: Bigelow TA, Church CC, Sandstrom K, et al. The thermal index: its strengths, weaknesses, and proposed improvements. J Ultrasound Med 2011;30(5):714-734.
Official statement. http://www.aium.org/officialStatements/17. Accessed March 1, 2017.
10 The following are images from fetal ultrasound performed at 14 weeks of gestation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree