SECTION XVI GENERAL RADIOLOGY IMAGING
Essentials 1
Questions
1. What is the most likely diagnosis?
A. Plantar fasciitis
B. Calcaneal fracture
C. Flexor hallucis longus tenosynovitis
D. Posterior tibialis tendon tear
E. Achilles tendon rupture
2. Which ONE of the following statements is correct for the test case injuries?
A. Acute Achilles tendon tears are most common in children and ballet dancers.
B. The most common location of an Achilles tendon tear is 2 to 6 cm above the calcaneal insertion.
C. On physical examination, patients are unable to dorsiflex the foot.
D. Human immunodeficiency virus and osteomyelitis are predisposing factors for Achilles tendon tears.
E. CT is superior to ultrasound and MRI in making the diagnosis.
3. What is the most common treatment for complete Achilles rupture tears?
A. No treatment necessary (as these are often asymptomatic)
B. Rest, stretching, and oral anti-inflammatory medications
C. Cast immobilization in plantarflexion
D. Surgical repair
Answers and Explanations
Question 1
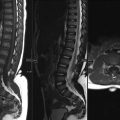
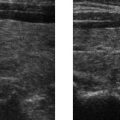
E. Correct! In this case, there is a tear of the Achilles in the midsubstance of the tendon. Fluid is seen filling the gap between the torn tendon ends.
Other choices and discussion
A. Plantar fasciitis is one of the most common causes of heel pain and is due to repetitive trauma. On imaging, there is thickening of the proximal plantar fascia (plantar thickness of > 4 mm), which extends to the calcaneal plantar fascial insertion. Ultrasound or magnetic resonance imaging (MRI) can be used to diagnose plantar fasciitis.
B. Intra-articular calcaneal fractures are caused by an axialloading mechanism and usually from a fall from height. This is the most commonly fractured bone found in this scenario. On radiographs, there can be a decrease of Bohler angle, which is normally 20 to 40 degrees. MRI can detect radiographically occult stress fractures, which manifest as linear T1-hypointense signal in the medullary space extending to the cortex with associated T2-hyperintense edema and hemorrhage. Calcaneal fractures can also be detected and characterized very accurately on computed tomography (CT). Of particular importance is the characterization of a calcaneal fracture into either an intra- or extra-articular category, as this is essential in guiding management and prognosis.
C. The flexor hallucis longus runs along the posteromedial ankle just deep to the posterior tibialis tendon and can cause posteromedial heel pain, if injured. Tenosynovitis, in general, is characterized by synovial fluid distending the tendinous sheath, which manifests on MRI as T1-hypointense and T2-hyperintense signal surrounding a low signal intensity tendon.
D. Posterior tibialis tendon rupture most commonly presents with flat foot and medial hind foot pain. MRI is the imaging modality of choice. Tears can be seen as enlarged tendons with fluid between the fibers, partially torn fibers with focal tendon thinning, or tendon discontinuity. Full-thickness tears typically occur > 1 cm from the navicular insertion.
Question 2
B. Correct! The blood supply of the Achilles tendon is the posterior tibial artery, and tendon tears commonly occur in the watershed zone, which is 2 to 6 cm above the calcaneal insertion. The relatively sparse vascular supply at this site increases the risk of tear.
Other choices and discussion
A. Achilles tendon tears typically occur in males between 30 and 50 years of age and are predominantly sports-related. The classic example is the unfit “weekend warrior” who participates in the occasional sporting activity. An audible snap is heard during forceful dorsiflexion of the foot.
C. Patients with full Achilles tendon tears are unable to plantarflex the foot.
D. Although most acute traumatic Achilles rupture cases occur in healthy men without heel or calf pain, there are some predisposing factors, which include chronic steroid injections, systemic inflammatory illnesses, fluoroquinolone use, gout, connective tissue disorders, and diabetes mellitus.
E. CT can detect a full-thickness tear, but ultrasound and MRI are superior to CT in diagnosing partial thickness Achilles tendon tears and tendinosis.
Question 3
D. Correct! Complete tears are usually surgically treated, as conservative treatment is unsuccessful if the tendon edges are not opposed. For < 3 cm of separation, end-to-end anastomosis is usually successful, and for > 3 cm separation, a tendon graft is often required.
It should be noted that more recently, there has been debate surrounding the issue of whether medical or surgical therapy is more appropriate for this type of injury.
Other choices and discussion
A. Injury is painful and can lead to loss of function. Some treatment is necessary for Achilles tendon pathology, particularly Achilles rupture tears.
B. Tendinopathy of the Achilles tendon is usually treated with rest, stretching, and anti-inflammatory medications.
C. Partial-thickness tears may be treated conservatively with cast immobilization. Surgical repair is indicated when conservative options fail.
Suggested Readings
Narvaez JA, Narvaez J, Ortega R, et al. Painful heel: MR imaging findings. Radiographics 2000;20:333–352 Schweitzer ME, Karasick D. MR imaging disorders of the Achilles tendon. Am J Roentgenol 2000;175:613–625Top Tips
Complete Achilles tendon ruptures usually occur in “weekend warrior” males 30 to 50 years of age. An audible snap is heard with forceful dorsiflexion of the foot.
Tears usually occur 2 to 6 cm proximal to the calcaneal insertion.
Axial and sagittal MRI can be helpful in differentiating partial from complete tears, and accurate measurement of the gap between the tendon edges is useful information for the surgeon.
Essentials 2
Case
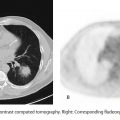
A 22-year-old man with a history of a recent motor vehicle accident (5 days prior) presents for follow up of a descending thoracic aortic injury.

Questions
1. Which ONE of the following is the best diagnosis?
A. Pericardial fluid
B. Paralyzed diaphragm
C. Flail chest
D. Traumatic left diaphragmatic rupture
E. Congenital diaphragmatic hernia
2. Which ONE of the following is correct regarding the test case diagnosis?
A. Surgical intervention is indicated in all cases, regardless of size.
B. Small diaphragmatic injuries will spontaneously heal.
C. Most cases will not result in herniation of abdominal contents into the chest.
D. The morbidity and mortality are lower if abdominal contents do not herniate at the time of presentation.
E. Traumatic diaphragmatic ruptures account for 25% of all diaphragmatic hernias.
3. Which ONE of the following best describes the location for traumatic diaphragmatic ruptures?
A. Anteromedial diaphragm, more commonly on the left
B. Posterolateral diaphragm, more commonly on the left
C. Apex of the diaphragm
D. Midline at the aortic hiatus
E. Midline at the esophageal hiatus
Answers and Explanations
Question 1
D. Correct! This patient has a traumatic left diaphragmatic rupture. A total of 75% of traumatic diaphragmatic ruptures are due to blunt trauma, and 25% are due to penetrating trauma. There is a high association with multiorgan trauma and concurrent life-threatening injuries. Imaging appearances range from discontinuity of the diaphragm with a focal defect to herniation of abdominal contents through a larger defect. The “dangling diaphragm” sign is present when the diaphragm curls inward on an axial image. The “collar” sign is a waist-like narrowing of the herniated viscus.
Other choices and discussion
A. Pericardial fluid is contained within the fibroelastic sac surrounding the heart. This can be important clinically when large pericardial effusions or scarred/inelastic pericardium result in pericardial compressive syndromes.
B. A paralyzed diaphragm remains intact, but fails to contract, resulting in asymmetric elevation of the affected diaphragm. There is typically no history of trauma.
C. A flail chest is defined as three or more segmental rib fractures or more than five adjacent rib fractures. There is paradoxical motion with respiration of the flail segment.
E. Bochdalek hernias occur in the posteromedial diaphragm, and Morgagni hernias occur in the anteromedial diaphragm. There is typically no history of trauma.
Question 2
A. Correct! Earlier diagnosis and repair leads to a better prognosis, as abdominal contents eventually herniate into the chest, if left unrepaired. Surgical treatment is indicated for all diaphragmatic injuries to decrease potential complications including ischemia of herniated bowel, central venous obstruction secondary to mass effect, devascularization, torsion, and ischemia of herniated solid abdominal organs.
Other choices and discussion
B. Traumatic diaphragmatic injuries do not spontaneously heal.
C. Due to negative intrapleural pressure, 80% of cases will eventually develop herniation of abdominal contents into the chest.
D. Patients are susceptible to the same complications regardless of whether the herniation of abdominal contents is present initially or only later.
E. Diaphragmatic ruptures account for only 5% of all diaphragmatic hernias. Congenital Bochdalek and Morgagni hernias, as well as hiatal hernias, are much more common.
Question 3
B. Correct! The most common location (90 to 98%) for traumatic diaphragmatic ruptures is the posterolateral aspect of the left hemidiaphragm, where there are weaker pleuroperitoneal membranes. The right hemidiaphragm is protected by the liver.
Other choices and discussion
The other choices are incorrect. Morgagni hernias are congenital diaphragmatic hernias that commonly occur in the anteromedial diaphragm. Hiatal hernias, both sliding and esophageal, occur near the midline at the esophageal hiatus. No diaphragmatic hernia has a predilection for the apex or the aortic hiatus of the diaphragm.
Suggested Readings
Desir A, Ghaye B. CT of blunt diaphragmatic rupture. Radiographics 2012;32:477–498 Dreizin D, Berqquist PJ, Taner AT, et al. Evolving concepts in MDCT diagnosis of penetrating diaphragmatic injury. Emerg Radiol 2015;22:149–156Top Tips
Most traumatic diaphragmatic ruptures occur in the posterolateral aspect of the left hemidiaphragm (90 to 98%).
Traumatic diaphragmatic ruptures have the best prognosis when diagnosed and repaired early.
Surgical treatment is indicated in all cases of traumatic diaphragmatic rupture.
Essentials 3
Case
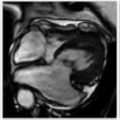
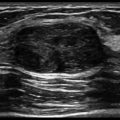
A 33-year-old woman presents to the emergency department with painful swelling of the right knee. No history of trauma.

Questions
1. Which ONE of the following is the correct diagnosis?
A. Pyrophosphate arthropathy
B. Cystic adventitial disease of the popliteal artery
C. Pes anserine bursitis
D. Popliteal cyst
E. Parameniscal cyst
2. Regarding this diagnosis, which ONE of the following is correct?
A. More commonly seen anteriorly when found in the medial compartment
B. Often seen in association with bucket handle meniscal tears
C. Often seen in association with horizontal meniscal tears
D. Usually cured with cyst aspiration
E. Best assessed with ultrasound
3. Which ONE of the following best describes the anatomic location for a popliteal cyst?
A. Extrasynovial structure in the anterior aspect of the knee that lies below the patella, posterior to the patellar tendon, and anterior to the femorotibial articulation
B. Medial aspect of the knee between the conjoined distal tendons of the sartorius, gracilis, and semitendinosus muscles, and the tibial insertion of the medial collateral ligament (tibial condyle)
C. Between the semimembranosus tendon and the medial collateral ligament (with a deeper portion extending between the semimembranosus tendon and the medial tibial condyle)
D. Between the medial head of the gastrocnemius muscle and the semimembranosus tendon
E. Para-articular cyst communicating with a meniscus
Answers and Explanations
Question 1
E. Correct! Parameniscal cysts represent encapsulated mass lesions that contain synovial-like fluid and are continuous with a meniscus. In the test case, this communication is demonstrated on the sagittal magnetic resonance imaging. On the plain film, there is lobulated soft tissue swelling medially.
Other choices and discussion
A. Pyrophosphate arthropathy occurs secondary to calcium pyrophosphate dihydrate deposition in soft tissues and cartilage. On plain film, there is typically associated calcification (or chondrocalcinosis).
B. Cystic adventitial disease is a rare vascular disorder characterized by focal cystic accumulation of mucinous fluid in arterial adventitia. Clinically, there may be sudden onset of intermittent claudication in a young male patient.
C. The pes anserine bursa is located between the conjoined distal tendons of the sartorius, gracilis, and semitendinosus muscles (pes anserinus) at the medial aspect of the knee.
D. The most frequent cause of a popliteal cyst in adults is degenerative arthritis.
Question 2
C. Correct! Parameniscal cysts are invariably associated with horizontal meniscal tears.
Other choices and discussion
A. Posterior horn tears (and their parameniscal cysts) are more common than anterior horn tears in the medial meniscus. The most common location for a lateral parameniscal cyst is adjacent to the anterior horn or body of the lateral meniscus.
B. Bucket handle meniscal tears are a type of vertical tear. Parameniscal cysts are invariably seen with horizontal meniscal tears.
D. Aspiration of the cyst is a temporary measure, and the cysts tend to recur. The diagnosis and treatment of the underlying meniscal tear is important.
E. Magnetic resonance imaging is the imaging study of choice. Ultrasound can show a partially cystic and sometimes septated mass bulging into the para-articular space. Protrusion of an abnormal meniscus into the cyst is sometimes seen. Demonstration of the meniscal tear, however, is not possible in most cases. Magnetic resonance imaging is helpful in assessing the meniscal tear and in characterizing important ancillary findings, such as the degree of underlying chondromalacia.
Question 3
D. Correct! A popliteal or Baker cyst extends from the knee joint posteriorly and medially, interposed between the tendons of the medial head of the gastrocnemius and the semimembranosus tendon.
Other choices and discussion
A. This is the location of a Hoffa fat pad ganglion.
B. This is the location for pes anserine bursitis.
C. This is the location for semimembranosus-tibial collateral ligament bursitis.
E. This describes a parameniscal cyst.
Suggested Readings
Perdikakis E, Skiadas V. MRI characteristics of cysts and “cyst-like” lesions in and around the knee: what the radiologist needs to know. Insights Imaging 2013;4:257–272 Steinbach LS, Stevens KF. Imaging of cysts and bursae about the knee. Radiol Clin North Am 2013;51:433–454Top Tips
Cysts and cystic-appearing soft tissue lesions in the medial compartment of the knee are common, and the differential considerations include popliteal cyst, parameniscal cyst, pes anserinus bursitis, and semimembranosus-tibial collateral ligament bursitis. Specific location is often diagnostic.
Parameniscal cysts are invariably associated with horizontal meniscal tears.
Diagnosis and treatment of the underlying meniscal tear is important with parameniscal cysts, as the cysts frequently recur if the meniscal tear is not also treated.
Essentials 4
Case
A 34-year-old woman presents with intermittent abdominal pain for several months, worse for the past 8 days. Her gallbladder was removed 6 years ago, and her current symptoms are reportedly similar to those that prompted the cholecystectomy.

Questions
1. What is the MOST likely diagnosis?
A. Surgicel
B. Postcholecystectomy bile leak/biloma
C. Spillage of gallstones
D. Stump cholecystitis
E. Normal postcholecystectomy appearance
2. Regarding imaging of a postcholecystectomy patient, which ONE of the following statements is true?
A. Biliary dilatation usually suggests bile duct obstruction and warrants further work up with magnetic resonance cholangiopancreatography.
B. The computed tomography appearance of Surgicel is often confused with a retained surgical swab.
C. Postcholecystectomy bile duct injury is the most common type of injury after this procedure.
D. Biliary complications are more common after open cholecystectomy than after laparoscopic cholecystectomy.
E. Cholecystectomy-related vascular injuries are usually due to bile leakage and subsequent infection.
3. Choose the MOST appropriate statement regarding stump cholecystitis.
A. Stump cholecystitis is more commonly seen after elective cholecystectomy than after emergent cholecystectomy.
B. Reported incidence of stump cholecystitis is around 15 to 20%.
C. Stump cholecystitis is usually diagnosed promptly after onset of symptoms because of the classic clinical presentation.
D. The definitive treatment is often surgical to excise the gallbladder remnant and perform completion cholecystectomy.
E. Once the diagnosis is confirmed, the definitive treatment is usually conservative and mainly reassurance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree