Fig. 15.1
CTA VR reformat of the left pelvic side. Type A bifurcation of the internal iliac artery (IIA). Posterior division with the superior gluteal artery (black arrow). Anterior division with the common gluteal-pudendal trunk bifurcating into inferior gluteal (white arrow) and internal pudendal (white dashed arrow) arteries. Only 1 prostate artery (PA) is seen (black arrowhead) arising from the common gluteal-pudendal trunk. The black dashed arrow marks an aberrant obturator artery arising from the inferior epigastric artery (external iliac artery)
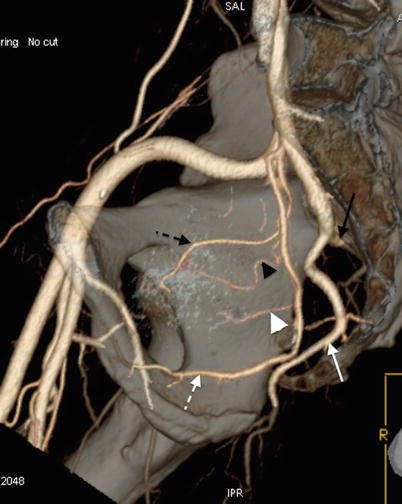
Fig. 15.2
CTA VR reformat of the right pelvic side. Type B bifurcation of the IIA. Posterior division with the superior gluteal (black arrow) and inferior gluteal (white arrow) arteries. Anterior division with the internal pudendal artery (white dashed arrow). Two PAs are seen arising from the internal pudendal artery. The black arrowhead marks the central gland PA, while the white arrowhead marks the peripheral gland PA. The black dashed arrow marks the obturator artery arising from the internal pudendal artery
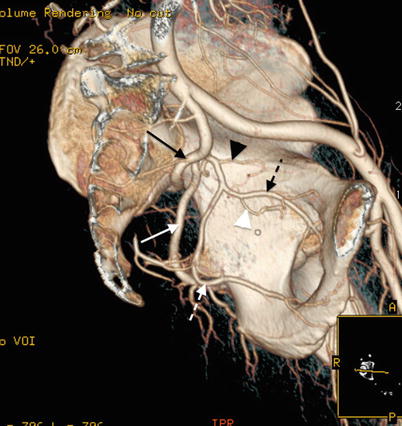
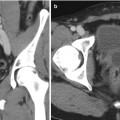
Fig. 15.3
CTA VR reformat of the left pelvic side. Type C bifurcation of the IIA. The superior gluteal artery (black arrow), the inferior gluteal artery (white arrow), and internal pudendal artery (white dashed arrow) arise simultaneously. Only 1 PA (white arrowhead) is seen arising from the obturator artery (black dashed arrow) that arises from the internal pudendal artery. The black arrowhead marks the superior vesical artery arising proximally from the anterior division of the IIA
Knowledge of the radiological anatomy of all these major branches may help during PAE and facilitate the identification of the PAs [8, 9]. CTA is a valuable pre-procedural tool to help plan the procedure and study the vascular anatomy of the male pelvic arteries [10]. The prostate has a dual vascular supply with a central gland artery and a peripheral gland artery [11]. The central gland PA has a horizontal trajectory underneath the bladder neck (thus, also called vesico-prostatic artery) and penetrates the prostate capsule in the anterior-lateral quadrants (thus, also called anterior-lateral or medial PA). The peripheral gland PA has an oblique trajectory downward, forward, and inward and runs in the fat behind the prostate, in front of the rectum. The peripheral gland PA penetrates the prostate capsule in the posterior-lateral quadrants (thus, also called posterior-lateral or lateral PA) and frequently shares common origins or anastomoses with rectal branches. The central gland PA feeds most of the upper half and central gland of the prostate and may give rise to inferior vesical branches to the bladder neck or vesiculo-deferential branches to the seminal glands along its trajectory. The peripheral gland PA feeds most of the lower half, apex, and peripheral prostate and frequently gives rise to rectal branches along its trajectory [11, 12].
The central gland and peripheral gland PAs may arise from one PA (Figs. 15.4, 15.5, 15.6, and 15.7) that bifurcates (60 % of pelvis) or from two independent PAs (40 % of pelvis) (Figs. 15.8, 15.9, 15.10, 15.11, 15.12, 15.13, 15.14, 15.15, 15.16, and 15.17). The PAs are larger when just 1 PA is present with approximately 2 mm in diameter, while PAs are smaller, approximately 1 mm in diameter, when two independent PAs are present. Prostate volume and PA diameter do not correlate, and patients with large prostates may have smaller PAs than patients with smaller prostates due to different number of PAs. PAs may arise from any of the IIA branches and even from outside the pelvic arteries [13]. The most frequent origins are the internal pudendal artery (30 %), superior vesical artery (20 %), and common gluteal-pudendal trunk (15 %). These origins are the “standard” anatomy representing up to 70 % of pelvis. The less frequent origins (20 %) are the obturator artery (12 %) and prostato-rectal trunks (8 %). Rare origins (<10 %) are the inferior (4 %) and superior (2 %) gluteal arteries, accessory pudendal arteries (2 %), and accessory obturator arteries (from the external iliac or inferior epigastric arteries, 2 %).

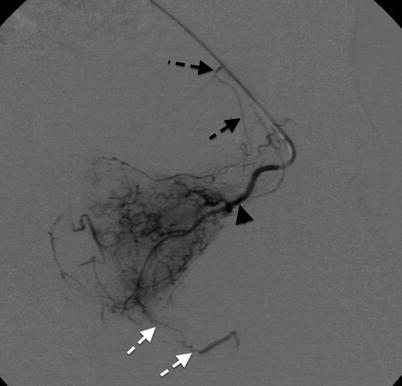
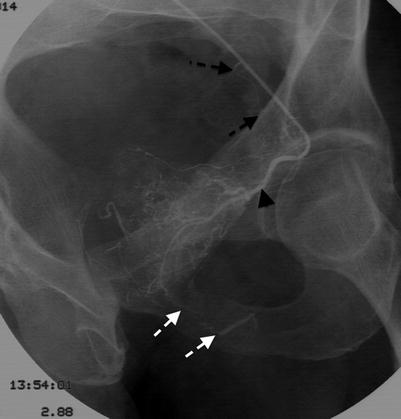
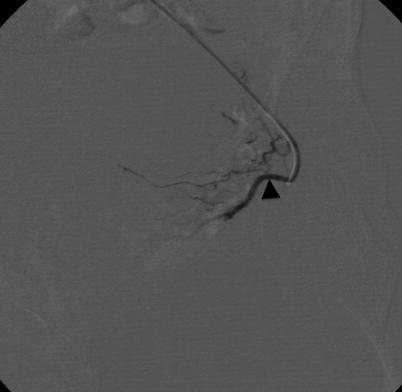

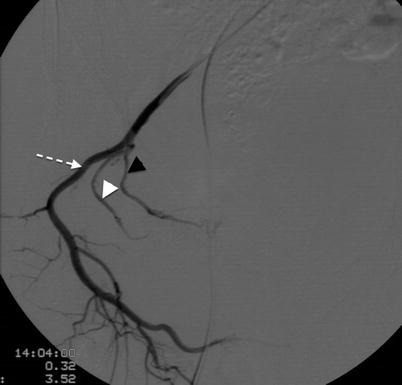
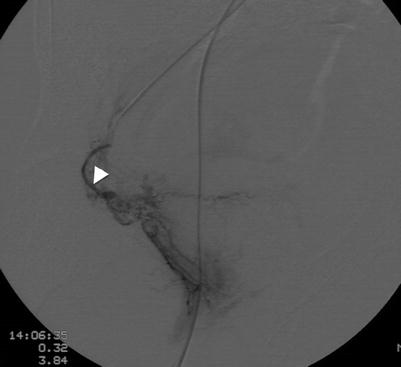

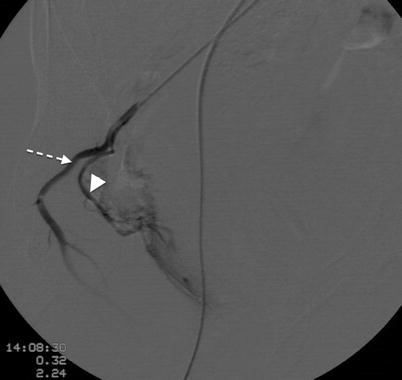
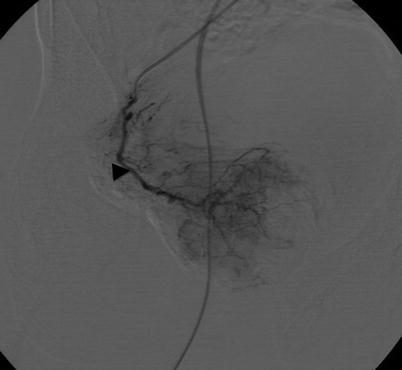
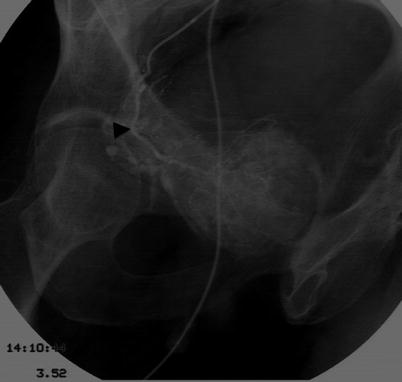

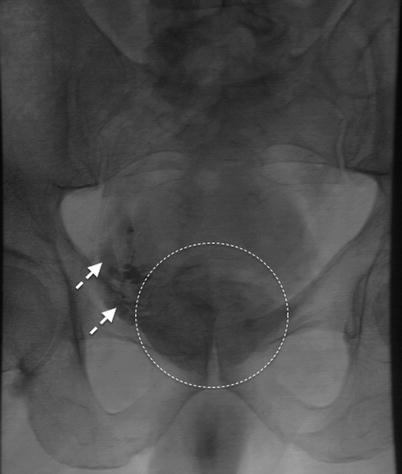
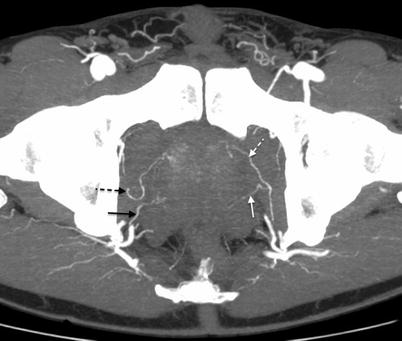

Fig. 15.4
CTA sagittal-oblique MIP reformat of the left pelvic side (same patient from Fig. 15.1). Type A bifurcation of the IIA. Posterior division with the superior gluteal artery (black arrow). Anterior division with the common gluteal-pudendal trunk bifurcating into inferior gluteal (white arrow) and internal pudendal (white dashed arrow) arteries. Only 1 PA is seen (black arrowhead) arising from the common gluteal-pudendal trunk. The black dashed arrows mark the superior vesical artery branches feeding the bladder
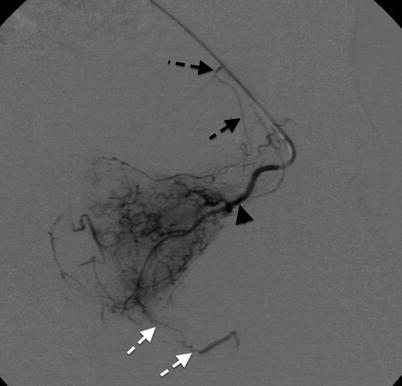
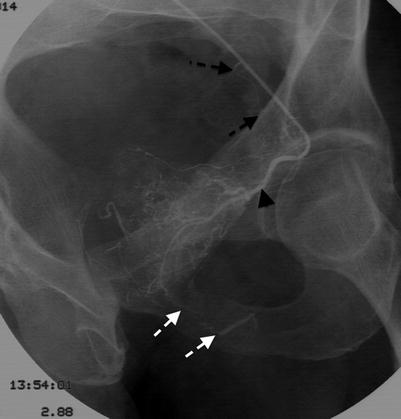
Fig. 15.6
Inverted image of Fig. 15.5 better depicting the vascularization of the central gland of the left hemiprostate. Anastomoses to the internal pudendal artery (white dashed arrows) and to the superior vesical artery (black dashed arrows) are seen
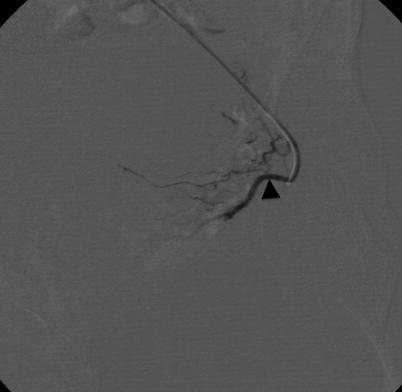

Fig. 15.8
CTA sagittal-oblique MIP reformat of the right pelvic side (same patient from Fig. 15.2). Posterior division with the inferior gluteal artery (white arrow). Anterior division with the internal pudendal artery (white dashed arrow). Two PAs are seen arising from the internal pudendal artery. The black arrowhead marks the central gland PA, while the white arrowhead marks the peripheral gland PA
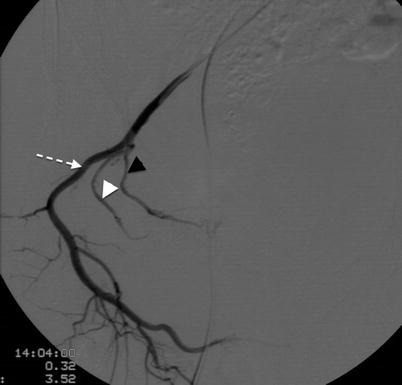
Fig. 15.9
DSA of the right internal pudendal artery (white dashed arrow) in ipsilateral anterior oblique projection (35°) and caudal-cranial angulation (−10°) of the same patient from Figs. 15.2 and 15.8. Two PAs are seen arising from the internal pudendal artery. The black arrowhead marks the central gland PA, while the white arrowhead marks the peripheral gland PA
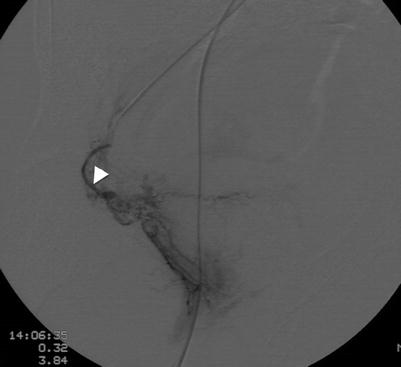

Fig. 15.11
Inverted image of Fig. 15.10 better depicting the vascularization of the peripheral gland of the right hemiprostate. Right peripheral gland PA (white arrowhead)
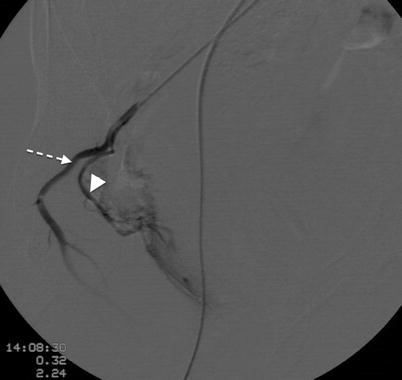
Fig. 15.12
Control angiogram after embolization of right peripheral gland PA (white arrowhead) seen in Fig. 15.10. Occlusion of the artery with no filling of the peripheral gland of the prostate and reflux into the internal pudendal artery (white dashed arrow)
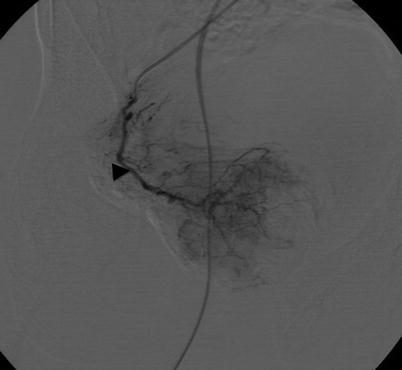
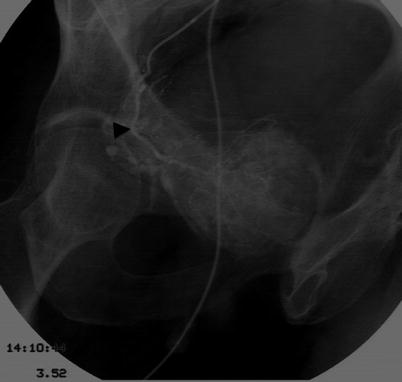
Fig. 15.14
Inverted image of Fig. 15.13 better depicting the vascularization of the central gland of the right hemiprostate. Right central gland PA (black arrowhead)

Fig. 15.15
Control angiogram after embolization of right central gland PA (black arrowhead) seen in Fig. 15.13. Occlusion of the artery with no filling of the central gland of the prostate and reflux into the internal pudendal artery (white dashed arrow)
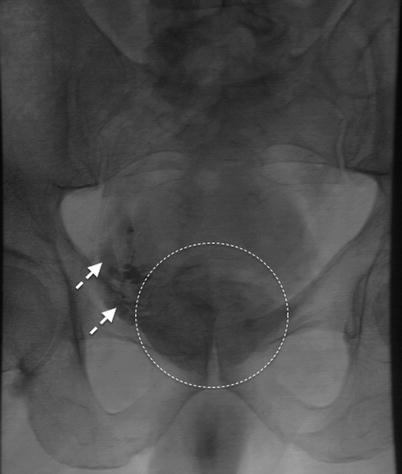
Fig. 15.16
Prostate staining with contrast after bilateral embolization (inside circle). Opacification of the right periprostatic venous plexus is depicted (white dashed arrows)
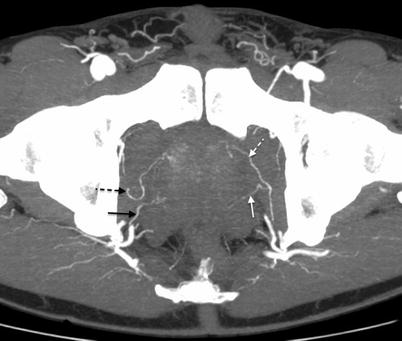
Fig. 15.17
CTA axial-oblique MIP reformat of the same patient from Figs. 15.1–15.16. Two independent PAs are seen on the right pelvic side, the central gland PA (black dashed arrow) and the peripheral gland PA (black arrow). On the left pelvic side, only one PA is seen bifurcating into central gland PA (white dashed arrow) and peripheral gland PA (white arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree