Chapter Outline
SUBACROMIAL SUBDELTOID BURSITIS
Subacromial Subdeltoid Bursitis
Anatomy and Clinical
The subacromial subdeltoid (SASD) bursa is one of the largest bursae in the body and plays an important role in patients with subacromial impingement. It is likely that much of the discomfort felt during arm abduction in patients with this clinical problem is due to inflammation within the bursa. Arm abduction, particularly between 30 and 60°, typically reproduces pain that is often felt over the lateral aspect of the deltoid rather than over the supraspinatus tendon itself. Patients find themselves unable to lie on the affected shoulder and sleep is interrupted. A variety of clinical signs assist in the diagnosis of impingement but do not clearly differentiate between bursitis and tendon tears. It can sometimes be difficult to differentiate between impingement and neural compression originating from cervical spondylosis. Pain obliterated by injection of local anaesthetic into the bursal space can be very helpful diagnostically.
Ultrasound Appearances
On ultrasound, SASD bursal disease may take two forms. In some cases the bursa becomes filled with fluid. In others, thickening of the bursal lining is more apparent and there may be little in the way of free fluid.
Bursal Fluid
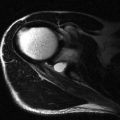
The normal bursa is a thin, low-reflective line surrounded by several layers of bright fat. It is generally no more than 1 mm in thickness but can occasionally be more. When fluid is present, there is separation of the fat layers and low-reflective fluid is detected. It is important not to press too hard with the ultrasound transducer or small quantities of fluid may be compressed out of the field of view and overlooked. If patients are examined in the seated position, it is important to look in the dependent area of the bursa to detect these small quantities of fluid. The probe should be passed around the margin of the deltoid so that the inferior part of the recess can be seen ( Fig. 3.1 ). Another useful place to find small quantities of bursal fluid is anterior to the biceps tendon ( Fig. 3.2 ). When fluid is detected around biceps, care needs to be taken to determine whether it lies within the biceps tendon sheath or within the SASD bursa. Fluid within the biceps tendon sheath extends more distally and surrounds the biceps tendon ( Fig. 3.3 ). Bursal fluid is limited by the lower limit of the bursal space anteriorly and cannot surround the tendon.



The presence of bursal fluid usually implies that bursitis is present, although a very tiny quantity could be considered normal. It does not mean that a rotator cuff tear is present, though the presence of a large quantity of fluid in both the bursa and joint is usually indicative of a full-thickness tear. Conversely, if there is a large quantity of fluid in the bursa and little, if any, glenohumeral joint fluid, a full-thickness rotator cuff tear is unlikely. Similarly, following a large volume bursal injection, if there is no increase in fluid in the glenohumeral joint or its extension into the biceps tendon sheath, communication between the bursa and glenohumeral joint indicating a full-thickness tear can also be considered unlikely.
Once fluid is detected, it is useful to try to make use of its presence to assess for supraspinatus tears. Fluid can be massaged by compression with the examiner’s free hand to the superior part of the bursa. Getting the patient to move the shoulder, particularly by elevating the arm, can force fluid into other areas of the bursa and outline abnormalities of the bursal surface of the tendon that may not otherwise have been apparent.
If particularly large amounts of fluid are present in the SASD bursa, especially when this is associated with marked thickening of the bursal lining ( Fig. 3.4 ), a cause other than impingement should be considered. Potential diagnoses include rheumatoid arthritis, crystal deposition disease, infection and haemorrhage. Crystal disease can be particularly painful and is suggested when multiple echogenic foci are identified within the thickened synovium and bursal fluid. This condition may progress to frozen shoulder. Haemorrhage within the bursa may also appear echogenic. This can be due to trauma, haemophilia or synovial angiomatous malformation. Less common causes include other synovial-based conditions, including infection, pigmented villo-nodular synovitis and synovial osteochondromatosis.

Bursal Thickening
The more common ultrasound finding in patients with SASD bursitis is thickening of the synovial lining rather than the presence of large quantities of fluid. It should also be appreciated that the bursa may appear normal in patients with painful bursal disease. In such cases, arthroscopy demonstrates a heavily injected but thin bursal lining. In most individuals, the normal bursa is represented by a thin, echo-poor line beneath brighter lines representing peribursal fat. Bursal thickening can be seen anywhere within the bursa, but the common locations to detect it are over the biceps tendon in long axis, around the anterior interval ( Fig. 3.5 ) and, most commonly, over the supraspinatus tendon in the coronal plane ( Fig. 3.6 ), where the bursa abuts the coracoacromial ligament.


The range of normal for bursal thickening is also quite large. In some it can be subtle and difficult to differentiate from normal. In others it is markedly thickened and may appear bunched up against the coracoacromial ligament. Just as some symptomatic patients have a normal or minimally enlarged bursa, some patients with obvious bursal thickening may be symptom-free. Focal bursal thickening or side to side difference of >2 mm may be more significant. As with the dynamic assessment of impingement, the patient’s symptoms underpin the diagnosis of impingement, and the diagnosis is unlikely in patients with full and pain-free shoulder abduction, regardless of the degree of bursal thickening.
Dynamic Assessment of Bursal Impingement
Detecting a minimally enlarged bursa is easier with arm movement. As has been described elsewhere, dynamic shoulder assessment is an important adjunct to the static examination and is used to detect more subtle manifestations of cuff and bursal disease. Changes in the configuration of the bursa should be sought during arm abduction as it impinges against either the lateral margin of the acromion or, more preferably, against the coracoacromial ligament ( Fig. 3.7 ).

The coracoacromial ligament is found by placing the probe in the axial plane over the anterior aspect of the shoulder so that the medial point overlies the bony coracoid. This bony landmark is easy to find with ultrasound, but if necessary, it can also be palpated. From this position, the lateral end of the probe is rotated upwards without moving the medial point. As the acromion comes into view, a ligamentous structure with an ordered homogeneous fibrillary pattern typical of ligaments is visualized ( Fig. 3.8 ). This is the coracoacromial ligament. The probe can then be rotated 90° keeping the ligament in view until it is seen in cross section. In short axis, the ligament is small, bright and oval shaped. With experience, the transverse image of the coracoacromial ligament can be quickly located without the need to find it in long axis. Just lateral to the ligament, the low-signal bursa is identified. The patient’s arm is then abducted and the bursa observed for thickening or bunching as it passes underneath the ligament. In some cases bursal bunching is quite dramatic and further abduction is blocked as the bursa cannot pass deep to the ligament. In others bursal bunching is more subtle and passage under the ligament is not obstructed. In a few patients, the bursa may initially be obstructed, but then passes underneath the ligament with an audible and palpable click. It is important not to press too heavily with the probe as this may impede the normal movement of the bursa or may prevent the bursa from clicking underneath the ligament.

The Biceps Tendon
Biceps Dislocation
Evaluation of the biceps and anterior interval begins with the probe in the axial plane overlying the bicipital groove: an easy to locate depression on the anterior aspect of the proximal humerus. The tendon should be located within the groove, usually surrounded by a small quantity of fluid. If the tendon is not present, it is either dislocated or ruptured. In such cases, the probe should be moved medially to see whether a displaced tendon can be found ( Fig. 3.9 ). The short head of biceps should be identified to ensure that this is not mistaken for a displaced long head. This differentiation is easy, as the short head tendon can be traced proximally to its origin from the coracoid.