- •
Cardiac magnetic resonance (CMR) allows imaging of the entire RV without interference of ribs or lungs.
- •
Because of high image quality and wide field-of-view, CMR imaging is the method of choice to assess the complex geometry and function of the RV.
- •
RV hypertrophy that results from increased loading conditions is accurately determined by CMR.
- •
CMR may support the diagnosis of ARVC/D by detecting RV dilatation and focal functional abnormalities of the RV wall.
- •
CMR techniques may help to characterize abnormal tissue composition of hypertrophic RV myocardium.
This first section shows images of a healthy patient to demonstrate normal right ventricular anatomy ( Figure 5-1 ).


Comments
The geometry of the right ventricle (RV) is more complex than of the left ventricle (LV). The LV can be compared with an elliptic cone with two valves (mitral and aortic valves) sharing the same anatomic plane. The RV cavity is wrapped around the left ventricle and can be divided into a posteroinferior inflow portion, containing the tricuspid valve, and an anterosuperior outflow portion, from which the pulmonary trunk originates. Because of this complex geometry, CMR has become the imaging technique of choice to precisely evaluate patients with congenital or acquired disease of the right ventricle.
This is a demonstration of Simpson or disk-area method for calculation of right ventricular end-systolic and end-diastolic volumes, and ejection fraction ( Figure 5-2 ).

Comments
Today, CMR is considered the gold standard for assessment of right ventricular volumes, mass, and function, for clinical as well as research purposes. It has been shown to have a good interstudy reproducibility of functional RV parameters in healthy subjects, and in patients with heart failure or hypertrophy. However, the reproducibility of the RV measurements is lower than for the LV.
A 77-year-old man presented for exertional dyspnea and atrial fibrillation for 5 months. A transthoracic echocardiogram showed a hypertrophic left ventricle with poor systolic and diastolic function. CMR was performed to retrieve the cause of the hypertrophy ( Figure 5-3 ).

Comments
Amyloidosis results from the deposition in tissues of fibrils formed from various proteins. Involvement of the heart is frequent, leads to restrictive cardiomyopathy, and progressive heart failure, and may finally lead to death. CMR imaging has been shown to correlate well with histologic findings, with areas of late contrast enhancement demonstrating the amyloid infiltration. When compared with endomyocardial biopsy, contrast-enhanced CMR has a sensitivity of 80% and a specificity of 94% for diagnosing cardiac amyloidosis. The distribution pattern of enhanced areas is highly variable and the extent of hyperenhancement correlates with ventricular dysfunction.
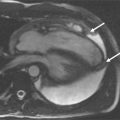
Follow-up examination 5 years after the initial diagnosis of idiopathic pulmonary hypertension ( Figure 5-4 ).

Comments
Severe pulmonary hypertension caused by diseases of the lung parenchyma and/or pulmonary vasculature can lead to cor pulmonale. Right ventricular hypertrophy develops to maintain a sufficient output against high pulmonary vascular impedance. Further elevation of the pulmonary pressure leads to dilation and systolic dysfunction of the right ventricle. CMR allows the exact determination of right ventricular mass, volume, and function in patients in whom echocardiographic diagnosis may be difficult because of poor image quality in the setting of chronic obstructive pulmonary disease. Moreover, the RV shape and position in the chest can make the calculation of RV volumes and ejection fraction by echocardiography unreliable.