Skeletal Trauma
Ramesh S. Iyer, MD
LEARNING OBJECTIVES
1. Describe three types of incomplete fractures.
2. List the Salter-Harris classification system (types I through V) for physeal fractures.
3. List the six ossification centers in the elbow in order of appearance, and approximate age when each ossifies.
4. Describe the use of the following landmarks on elbow radiographs: anterior humeral line, radial head-capitellar line, and the “fat pad” sign.
5. Identify three common acute elbow fractures.
6. Recognize the normal physis in the proximal humerus.
7. Recognize the typical appearance of a toddler’s fracture.
8. Identify two physeal fractures of the distal tibia in early teenagers.
9. Describe the components of a radiographic skeletal survey for nonaccidental trauma.
10. Identify a classic metaphyseal lesion on radiography, and discuss its significance.
INTRODUCTION
The normal radiographic appearance of the growing skeleton is very different than that of adults. This is most pronounced in areas of bone growth (physes) and separate ossification centers (apophyses). Developing bones have different biomechanical responses to injury than mature bones because they are more pliable and have a greater cartilaginous component. Physeal trauma is unique to children and has characteristic patterns on imaging. The radiologist who is familiar with developmental anatomy and common pediatric fractures is more effective at directing care in the emergency department.
INCOMPLETE FRACTURES
Pediatric long bones are more elastic than are adult bones, rendering them more susceptible to bowing deformities and other incomplete fractures. These injuries are most common in the forearm, tibia, and fibula. Bowing or plastic deformities occur when the bone is smoothly bent without cortical disruption (Fig. 25.1). They are caused by longitudinal stresses, such as a FOOSH injury (fall on outstretched hand), where the force applied exceeds elastic recoil of the bone but is not enough to cause cortical failure. Plastic deformities are treated with closed reduction and casting.1,2
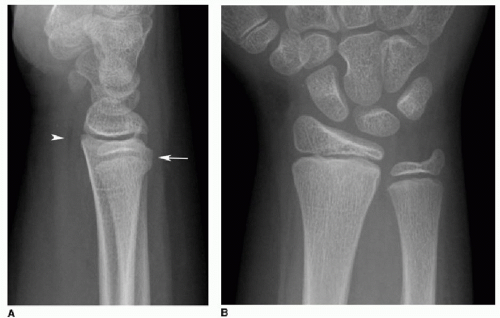
Torus fractures, or buckle fractures, refer to buckling or bulging of a single cortex as a result of an axial load to a long bone. The word torus means swelling or protuberance and describes the
convex molding at the base of classic Greek columns. The affected cortex is on the compression side, while the cortex on the tension side is intact (Fig. 25.2). The fractures are often located in the dorsal cortex of the distal radius or ulna, 2 to 3 cm proximal to the physis. The cortical buckling is often subtle and may only be visible on one projection. Torus fractures are managed with splint immobilization.1,2
convex molding at the base of classic Greek columns. The affected cortex is on the compression side, while the cortex on the tension side is intact (Fig. 25.2). The fractures are often located in the dorsal cortex of the distal radius or ulna, 2 to 3 cm proximal to the physis. The cortical buckling is often subtle and may only be visible on one projection. Torus fractures are managed with splint immobilization.1,2
 FIG. 25.1 • Plastic deformity of the radius in a 6-year-old male. AP forearm radiograph shows mild smooth, lateral convex bowing of the radius (arrows), along with a midshaft ulnar fracture. |
Greenstick fractures occur when a force is applied perpendicular to the shaft of the long bone. The cortex opposite to the bending force fractures, while the cortex on the same side of the force bends (Fig. 25.3). “Greenstick” refers to the appearance of a branch or sapling as it partially breaks under a similar bending force. These fractures are effectively treated with closed reduction and casting.1,2
PHYSEAL FRACTURES
The physis, or growth plate, is a cartilaginous zone located between the epiphysis and metaphysis that provides longitudinal bone growth through endochondral ossification. About 15% of all pediatric fractures involve the physis. In the growing skeleton, the physis is weaker than are surrounding ligaments or tendons. The same injury that causes a ligamentous tear or joint dislocation in an adult may instead cause a growth plate injury in a child. The physis is also more susceptible to shear or tension forces compared to adjacent bone. This fragility is increased during times of rapid growth. Physeal injuries can produce irreversible damage to growing cells, potentially resulting in growth disturbance, angular deformity, altered joint mechanics, and long-term disability.3,4
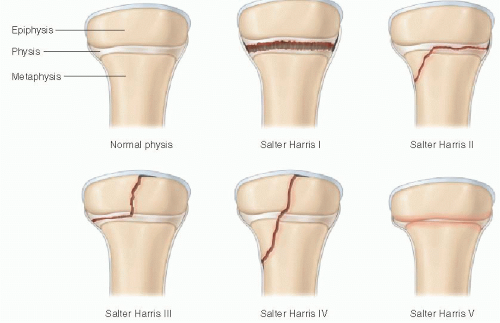
The most widely used method for characterizing physeal fractures is the Salter-Harris classification system (Fig. 25.4). Type I injuries involve only the physis. They usually occur in children under 5 years and are often subtle on radiography. Type II fractures are the most common, constituting 75% of Salter-Harris injuries. These involve both the physis and the metaphysis, often producing a triangular fracture fragment. Type III fractures involve the physis and the distal epiphysis and are intra-articular. One common example of this injury is the Tillaux fracture of the distal tibia. Type IV fractures involve the metaphysis, physis, and epiphysis. An example of this is the triplane fracture of the distal tibia. Type V fractures are crush injuries to the growth plate and are uncommon. Higher-grade Salter-Harris fractures are more likely to cause premature physeal fusion. One method to remember this classification scheme is the acronym “SALTR”:
S: Slipped, separated, or straight across the physis
A: Above—fracture extends above the physis (metaphysis)
L: Lower—fracture extends below the physis (epiphysis)
T: Through—fracture involves the metaphysis, physis, and epiphysis (e.g., triplane)
R: Ruined—crush injury to the physis
ACUTE ELBOW TRAUMA
Elbow fractures are among the most frequent injuries in children. Fracture patterns are different between children and adults— while radial neck fractures are common in adults, supracondylar humeral injuries are by far the most common in pediatric patients. Familiarity with radiographic landmarks and the ossification sequence is critical for image interpretation. Basic radiographic evaluation begins with well-positioned AP and lateral projections.
The six ossification centers of the elbow appear in a predictable fashion: capitellum (1 to 2 years), radial head (2 to 4 years), medial (internal) epicondyle (4 to 6 years), trochlea (9 to 10 years), olecranon (9 to 11 years), and lateral (external) epicondyle (9.5 to 11.5 years) (Fig. 25.5).5,6 These can be remembered by the acronym CRITOE (Table 25.1). The ossification sequence may also be remembered by using the odd numbers from 1 through 11 years. For example, the capitellum ossifies at 1 year, followed by the radial head at 3 years, and so forth.6
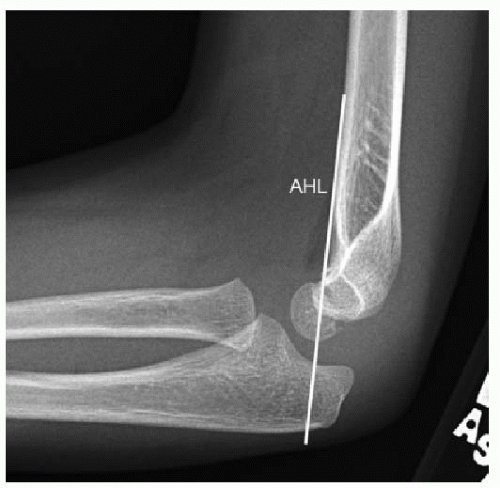
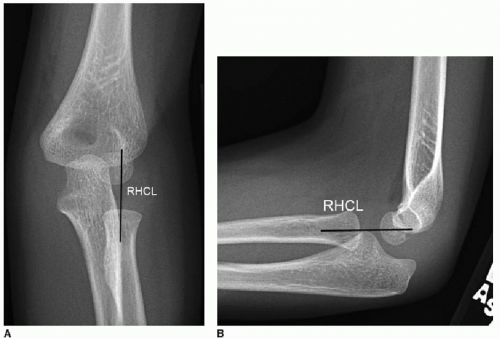
The anterior humeral line and radial head-capitellar lines are useful for assessing normal radiographic alignment. On the lateral projection, a line drawn along the anterior humeral cortex should bisect the middle third of the ossified capitellum (Fig. 25.6). In children 3 years and younger, where a larger portion of the capitellum has not yet ossified, the anterior humeral line may intersect the anterior or middle thirds. In all children, a line parallel to and bisecting the radial head and neck should intersect the capitellum on all projections (Fig. 25.7). If the integrity of one or both of these lines is compromised, then fracture and/or dislocation should be suspected.7, 8 and 9
Detecting an elbow joint effusion (“fat pad” sign) is strong evidence for the presence of a fracture. Similarly, the lack of a joint effusion excludes a fracture in over 90% of cases. The posterior humeral fat pad is usually not visible on the lateral projection. The anterior fat pad is normally visible as a thin lucent arc abutting the distal humerus (Fig. 25.8A). When there is a joint effusion, the posterior fat pad is displaced from the intercondylar depression and becomes visible, while the anterior fat pad becomes bulbous or sail-like (“sail sign”) in appearance (Fig. 25.8B).5,7 Usually, the offending fracture is obvious. In more subtle cases, close attention to the supracondylar humerus, proximal radius, and olecranon process may reveal minimally displaced fractures. The management for patients with elbow joint effusions with or without subtle fractures detected is typically the same—splinting the elbow and reimaging with radiographs in 1 to 2 weeks to evaluate for fracture healing.
Supracondylar distal humeral fractures account for twothirds of acute elbow injuries in children.10 They usually occur in
children aged 3 to 10 years after a FOOSH injury. The vast majority (95%) of supracondylar fractures result from elbow hyperextension, where the olecranon process of the ulna serves as a fulcrum to fracture the distal humerus. Most supracondylar fractures are best shown on the lateral elbow radiograph. The distal fragment is displaced and angulated posteriorly, with the anterior humeral line now passing anterior to the middle third of the capitellum (Fig. 25.9). A joint effusion is nearly always present. The Gartland classification (types I to III) may be used to characterize supracondylar fractures (Table 25.2). Fracture displacement greater than 2 mm and/or compromise of the posterior humeral cortex is an indication for surgical pinning.7,11,12
children aged 3 to 10 years after a FOOSH injury. The vast majority (95%) of supracondylar fractures result from elbow hyperextension, where the olecranon process of the ulna serves as a fulcrum to fracture the distal humerus. Most supracondylar fractures are best shown on the lateral elbow radiograph. The distal fragment is displaced and angulated posteriorly, with the anterior humeral line now passing anterior to the middle third of the capitellum (Fig. 25.9). A joint effusion is nearly always present. The Gartland classification (types I to III) may be used to characterize supracondylar fractures (Table 25.2). Fracture displacement greater than 2 mm and/or compromise of the posterior humeral cortex is an indication for surgical pinning.7,11,12
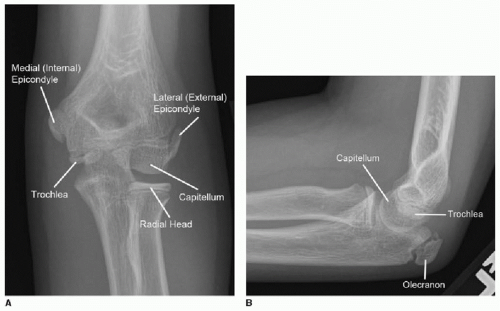 FIG. 25.5 • Normal elbow ossification centers in a 10-year-old female, AP (A) and lateral (B) radiographs. |
Lateral condylar fractures are the second most common acute elbow fracture in children (10% to 20% of such fractures). Elbow hyperextension with varus stress is the mechanism of injury. They are generally regarded as Salter-Harris type IV fractures (Fig. 25.10). In addition to standard AP and lateral radiographs, an internal oblique projection may show lateral condyle fractures to greater advantage. Fractures with less than 2 mm of displacement are managed with cast immobilization, while greater fragment displacement necessitates surgical fixation. Most orthopedic surgeons have a lower threshold to treat lateral condyle fractures operatively than supracondylar injuries. This is because most lateral condylar fractures have physeal and intra-articular involvement and are more prone to growth arrest and osteoarthritis if inadequately treated.5,13,14
Table 25.1 SIX OSSIFICATION CENTERS OF THE ELBOW, “CRITOE” | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree