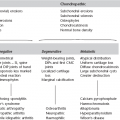
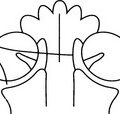
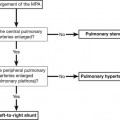
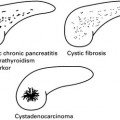
12 12.1 Acute arterial infarct: CT 1. Initial appearances often normal in first few hours. Larger infarcts more conspicuous. (a) Low density with reduced grey/white differentiation (cell and tissue swelling): wedge shaped, involving grey and white matter; ‘insular ribbon sign’ (loss of grey/white differentiation in perisylvian region; loss of normal anatomical differentiation of basal ganglia). (b) Mass effect – local (sulcal effacement). (c) Hyperdense vessels due to thrombus (luminal/mural); usually middle cerebral or basilar arteries (mural calcification may mimic hyperdense artery [string] sign). (a) More extensive area of low attenuation or progressive decreased attenuation. (b) Generalized mass effect (ventricular or basal cistern effacement ± midline shift [subfalcine herniation] or other herniation syndromes: uncal, transtentorial). (c) Secondary haemorrhagic transformation (usually occurs after a few days unless anticoagulated; reperfusion injury) if haemorrhage from outset consider embolus or venous stroke. 4. Contrast enhancement usually unhelpful and often confusing; simply reflects breakdown of blood–brain barrier. Any enhancement pattern possible. 5. CT perfusion study may demonstrate decreased perfusion in wider area of brain (ischaemic penumbra) suggesting further tissue at risk. 6. CT angiography can demonstrate dissection/stenosis/occlusion (embolic or thrombotic). 12.2 Acute arterial infarct: MRI 1. More sensitive than CT but signs similar (reduced attenuation on CT = increased T2 signal on MRI). Wedge shaped; grey and white matter involvement; often initially cortical change). Signal change usually (but not always) evident within 3–6 hours (within minutes on DWI). Increased T2 signal due to cytotoxic oedema (cell swelling; restricted diffusion). 2. Acute infarcts show increased DWI signal and low ADC. Low ADC signal ‘pseudonormalizes’, i.e. becomes bright from around 5–10 days postinfarct. 3. Mass effect – local and/or general as on CT. 4. Absent flow voids in affected major vessels; increased signal on T2 and FLAIR; most often seen in MCA (check carotid canal at skull base) or basilar. 5. Contrast enhancement may be confusing as on CT; prolonged transit time of contrast through distal or collateral vessels may be seen on postgadolinium T1 sequences. 6. Perfusion-weighted imaging may show poor perfusion in wider territory than changes on standard sequences: diffusion/perfusion mismatch may demonstrate ischaemic penumbra representing potentially salvageable brain tissue. 7. MR angiography may show vessel stenosis/occlusion in extracranial or intracranial vessels. 12.3 Venous infarcts 1. Usually secondary to venous sinus thrombosis: (a) CT – hyperdense and expanded sinus precontrast; peripheral enhancement around luminal thrombus postcontrast (delta sign). (b) MRI – absence of normal flow void: acute thrombus high signal on T1 (methaemoglobin); variable signal on T2 (beware normal variation in venous sinus anatomy with areas of hypoplasia). (c) Check for evidence of underlying cause on scans (mastoid infection, paranasal sinus infection, etc.). 2. If an area of infarction is seen which is not in arterial distribution, consider sinus thrombosis. 3. Venous infarction often haemorrhagic (but this is not a contraindication to anticoagulation; aim of anticoagulation is to stop propagation of thrombus). 4. Beware symmetrical low attenuation in deep grey matter structures (especially thalami); suggests involvement of deep cerebral veins which may not otherwise be seen on scans. 12.4 Indications for CT and MRI in acute stroke 1. If CT normal but clinical suspicion high, MRI more sensitive for early detection. 2. Assessment of diffusion/perfusion mismatch and suitability for thrombolysis. 3. Detection of stroke in distribution not well seen on CT (vertebrobasilar circulation in posterior fossa especially). 4. Detection of underlying cause such as arterial dissection or thrombosis (absent flow voids on standard sequences; narrowing/occlusion on MR angiography). 5. Assessment of intracranial and extracranial vessels by MR angiography. 12.5 Differentiation between infarct and tumour 1. Clinical history – abrupt vs gradual onset and development of symptoms. 2. Distribution – tumours not confined to vascular territory. 3. Shape – infarcts usually wedge shaped with base at periphery; tumours tend to be spherical/ovoid. 4. Tissue involvement – infarcts involve grey and white matter; most metastases or higher-grade gliomas involve white matter primarily; lower-grade primary tumours may involve grey matter. 5. Advanced imaging techniques such as DWI or MR spectroscopy may be useful in cases that remain unclear on standard sequences. 12.6 Appearances of blood on scans 1. Acute = higher attenuation than underlying brain (soon after episode of bleeding for up to 7–10 days). 2. Subacute = similar attenuation to underlying brain (transition usually occurs between 1 and 2 weeks). 3. Chronic = lower attenuation than underlying brain (suggests at least 2–3 weeks old but could be older). 1. Oxyhaemoglobin – iso/hypointense T1; hyperintense T2 (less than 24 hours approx.). 2. Deoxyhaemoglobin – iso/hypointense T1; hypointense T2 (1–3 days approx.). 3. Intracellular methaemoglobin – hyperintense T1; hypointense T2 (3–7 days approx.). 4. Extracellular methaemoglobin – hyperintense T1; hyperintense T2 (1–2+ weeks approx.). 5. Haemosiderin – isointense/hypointense T1; hypointense T2. 12.7 Subarachnoid haemorrhage 1. Ruptured intracranial aneurysm (75%): potentially devastating condition with 50% immediate mortality and high long-term morbidity. 2. Bleeding from vascular malformation (cerebral or spinal) (5%). 3. Trauma – tends to have peripheral distribution in sulci rather than concentrated in basal cisterns. 4. Extension from parenchymal haematoma (often hypertensive bleed) (5%). 5. Perimesencephalic haemorrhage – low pressure probable venous haemorrhage; few symptoms and signs and good prognosis. 1. CT – most sensitive in first few days (98% on day 1, only 50% positive by 7 days). Check review areas on scans: anterior interhemispheric fissure, sylvian fissure, posterior horns of lateral ventricles, third ventricle, basal cisterns, foramen magnum. CT angiography may be performed. 2. Lumbar puncture – negative CT scan does not exclude SAH, especially if scan performed days after ictus; therefore lumbar puncture mandatory if CT negative. 3. Late MRI more sensitive than CT – proton density, gradient echo T2 and FLAIR sequences most sensitive. 4. Catheter angiography now used less often in initial work-up as CT angiography often used at time of diagnosis of aneurysmal SAH and for planning therapy (neurointerventional vs surgical). 12.8 Intracranial aneurysms 1. Sudden onset of severe headache ± neurological signs ± reduced level of consciousness with scan findings of: (b) Parenchymal haemorrhage (usually with associated SAH). (c) Intraventricular haemorrhage (most often secondary to bleeding in the general subarachnoid space, occasionally primary). Incidence in general population ~2–3%. Overall risk of rupture = 0.5–1.5% per annum: variable according to size and position of aneurysm, sex, smoking, etc. 1. CT and CT angiography – extra-axial mass in subarachnoid space; enhances if patent; may be thrombosed and/or have calcification (especially giant aneurysms). CT angiography demonstrates site and morphology of aneurysm and may allow planning of treatment (neurointervention vs surgery) without need for catheter angiography. 2. MR and MR angiography – patent aneurysm will show flow void; giant or partially thrombosed aneurysms can show complex flow patterns with heterogeneous signals on standard sequences. Not reliable for treatment planning. 3. Catheter angiography – invasive with 0.1–0.5% inherent stroke risk. Still considered gold standard but may soon be superseded by CT angiography. 12.9 Vascular malformations Two main types: those with arteriovenous shunts and those without shunts. 1. Arteriovenous malformations – present in young to middle-aged adults with one or combination of haemorrhage (40%), seizures (30%), neurological deficit or headache (20%). Annual cumulative rupture risk ~3% per year. Consist of one or more arterial pedicles draining directly to enlarged draining veins through nidus. Multiple lesions in various syndromes: e.g. Osler–Weber–Rendu and Wyburn–Mason. (a) CT – hyperdense enlarged serpiginous vessels; often speckled calcification; enhance strongly. (b) MRI – serpiginous flow voids; may be evidence of local atrophy and gliosis or previous haemorrhage. (c) Catheter angiography – gold standard for assessment of morphology and nidal architecture including presence of associated arterial or venous aneurysms, varices and stenoses. 2. Dural arteriovenous fistulae – acquired lesions presenting in older population (50–70 years) compared to AVMs (20–40 years). Occur following damage to venous structures (post-thrombosis, surgery, trauma). Symptoms and signs secondary to arterialization of venous system: bruit, venous hypertension, pulsatile tinnitus (if primary involvement is sinuses); haemorrhage, focal neurology, seizures (if primary or major secondary involvement of cortical veins). Caroticocavernous fistula may give rise to proptosis and chemosis. (a) CT – often normal unless complications, e.g. haemorrhage; enlargement of cavernous sinus and superior ophthalmic veins if caroticocavernous fistula. (b) MRI – standard sequences often normal unless complication; dynamic subtraction angiography demonstrates lesions well. (c) Catheter angiography – still gold standard for diagnosis and demonstration of morphology on which classification and treatment planning based. 1. Cavernous angioma (cavernoma) – sinusoidal spaces lined with endothelium; occur anywhere in CNS, commonest pons. Present with small haemorrhages (usually not associated with large haemorrhages) or seizures; often incidental findings. Multiple cavernomas may be familial. (a) CT – iso/hyperdense lesion, often calcification. (b) MRI – characteristic appearance is heterogeneous signal centre with low T2 signal (haemosiderin) rim. Gradient echo most sensitive sequence for detection. 2. Developmental venous anomaly (venous angioma) – probably due to persistent embryonic veins which drain normal brain. Not thought to have increased haemorrhage risk. 12.10 CNS infection 1. Bacterial meningitis – CT usually normal. May see generalized brain swelling and/or focal or generalized ischaemia. Scanning only postcontrast may mask pathology. If contrast to be used, precontrast and postcontrast scans should be obtained. Lack of enhancement does not exclude meningitis. Hydrocephalus may be communicating and/or obstructive. 2. Subdural effusion or empyema – low attenuation extra-axial collection ± rim enhancement. 3. Cerebritis – diffuse area of parenchymal low attenuation which may develop into abscess. 4. Abscess – thin-walled rim-enhancing lesion; may be very little systemic disturbance. 1. CT – less sensitive than MRI, often normal in early HSV encephalitis; low attenuation in medial temporal lobes, later usually unilateral; may be haemorrhagic. 2. MRI – increased T2 signal in medial temporal lobes, insula, cingulate gyrus; usually bilateral but asymmetrical. Atrophy, gliosis and encephalomalacia long term. 1. Subacute sclerosing panencephalitis (SSPE) – progressive increased T2 signal and atrophy several years after primary measles infection. 2. Rasmussen’s encephalitis – progressive neurological deficits and intractable seizures in children; increased T2 signal and atrophy in one cerebral hemisphere. 1. Sporadic CJD – rapidly progressive dementing illness associated with myoclonus, ataxia, pyramidal and extrapyramidal signs, cortical blindness. MRI – increased T2 and FLAIR signal in caudate and putamen (corpus striatum); less often signal change in thalamus, globus pallidus and periaqueductal grey. 2. Variant CJD – sensory disturbances, depression, abnormal eye movements and involuntary movements. Encephalitis and encephalitis-like disorders Aiken, A. H. Central nervous system infection. Neuroimaging Clin N Am. 2010; 20(4):557–580. Foerster, B. R., Thurnher, M. M., Malani, P. N., et al. Intracranial infections: clinical and imaging characteristics. Acta Radiol. 2007; 48(8):875–893. Hughes, D. C., Raghavan, A., Mordekar, S. R., et al. Role of imaging in the diagnosis of acute bacterial meningitis and its complications. Postgrad Med J. 2010; 86(1018):478–485. 12.11 HIV and the brain 1. HIV – progressive dementia and atrophy due to subacute encephalitis. (a) CT – diffuse white matter low attenuation. (b) MRI – diffuse/patchy white matter high T2 signal, may involve basal ganglia. Mass effect and contrast enhancement usually absent. 2. Cytomegalovirus – typically signal abnormalities seen in periventricular distribution. 3. Progressive multifocal leukencephalopathy; papovavirus infection. 12.12 Congenital CNS infections 1. CMV – damages germinal matrix causing periventricular calcification. Earlier infection leads to more extensive damage. 2. Toxoplasmosis – focal areas of calcification more widespread than with CMV and involve basal ganglia, periventricular regions and cortex. 3. Rubella – microcephaly, parenchymal calcification and atrophy. 4. HIV – diffuse cerebral atrophy; may cause calcification of basal ganglia after first year. 12.13 Head injury 1. Fracture – impact head injury; commonest = linear; complex fractures (diastatic, stellate, depressed) tend to occur with mechanisms involving greater degrees of force; skull base fractures may be occult (look for secondary clues such as fluid in sphenoid sinus or mastoid air cells; pneumocephalus); facial nerve palsy or ossicular disruption in temporal fractures. 2. Extradural haemorrhage – usually arterial bleed (middle meningeal); biconvex lentiform haematoma (limited by coronal and lambdoid sutures as inner layer of dura bound to sutures but may cross sagittal suture); mixed attenuation haematoma may mean ongoing bleeding. 3. Subdural haemorrhage – usually venous low-pressure bleed; crescentic biconcave collection over cerebral hemisphere (can cross coronal and lambdoid but not usually sagittal sutures). 4. Subarachnoid haemorrhage – post-traumatic SAH usually low-volume scattered bleeds; peripheral distribution. 5. Contusions – larger mixed attenuation (CT) or signal (MRI) intra-axial lesions; tend to occur in inferior frontal and anterior temporal lobes (impact against bony anterior walls of anterior and middle cranial fossae); usually surrounding oedema adding to mass effect. 6. Diffuse axonal injury – smaller lesions than contusions; shearing injury secondary to rotational or acceleration/deceleration forces; tend to be widespread occurring at grey–white junction, corpus callosum, internal capsule and brainstem. 1. Cerebral oedema and ischaemia – may lead to cerebral herniation syndromes. 2. Subfalcine – midline shift which can give rise to ischaemia in distribution of anterior cerebral artery; contralateral hydrocephalus with obstruction at foramen of Monro. 3. Uncal – medial aspect of medial temporal lobe presses on third nerve (fixed dilated pupil). 4. Transtentorial – descending transtentorial herniation causes brainstem distortion and ischaemia in distribution of posterior cerebral artery. 1. Atrophy – focal (following contusion, etc.); generalized (following DAI or large extra-axial haematomas which required surgical evacuation). 2. CSF leak – secondary to fractures of frontal sinus, anterior cranial fossa, sphenoid sinus, temporal bone (secondary meningitis). 3. Arteriovenous fistula – direct caroticocavernous fistula. 4. Pseudoaneurysm – following arterial wall tear. 5. Leptomeningeal cyst – dura trapped within fracture line, CSF pulsation prevents fracture healing, leading to ‘growing fracture’. Kemp, A. M., Jaspan, T., Griffiths, J., et al. Neuroimaging: what neuroradiological features distinguish abusive from non-abusive head trauma? A systematic review. Arch Dis Child. 2011; 96(12):1103–1112. Kubal, W. S. Updated imaging of traumatic brain injury. Radiol Clin North Am. 2012; 50(1):15–41. 12.14 Hydrocephalus 1. Commensurate enlargement of temporal horns. 2. Ventricles disproportionately enlarged compared to sulci. 3. Effacement of third ventricular recesses. Increased CSF volume may be due to: 12.15 Pneumocephalus 1. Trauma – compound fractures of vault, fractures involving paranasal sinuses or mastoid air cells. 3. Osteoma of paranasal sinus (especially ethmoid) may erode through sinus wall. 4. Other sinus or skull base erosive tumours. 5. Empty sella – rare complication = development of communication between sella and sphenoid sinus. 12.16 CT attenuation of cerebral masses Relative to normal brain (masses with variable appearances not included). 12.17 Differential diagnosis of a solitary intracerebral mass 1. Primary brain tumour – high-grade tumours tend to have most mass effect (tumour and surrounding oedema), heterogeneous with areas of necrosis (glioblastoma); may infiltrate and involve/cross corpus callosum; variable enhancement but tends to increase with increased grade. 2. Metastasis – appearance variable on scans depending on primary; often considerable associated oedema (vasogenic, white matter), multiple/solitary, often located grey–white junction. 3. Arterial infarct – developing low attenuation (CT), high T2 signal (MRI) wedge-shaped lesion with variable mass effect; various enhancement patterns if contrast given. 4. Venous infarct – area of low attenuation (CT), high signal (MRI) not in arterial distribution, often associated mass, often haemorrhagic. 5. Abscess – homogeneous, thin enhancing rim, usually considerable vasogenic oedema. 6. Acute demyelinating plaque – may be very large with minimal clinical signs; low attenuation (CT) and high T2 signal (MRI); variable enhancement. 7. Haematoma – subacute to chronic. 8. Cerebritis/encephalitis – poorly defined area of low attenuation (CT); HSV predilection for limbic system; variable enhancement. 9. Aneurysm – may give rise to mass effect by itself but also often associated oedema in surrounding brain; appearance varies according to whether patent or associated intramural thrombus ± calcification. Essig, M., Anzalone, N., Combs, S. E., et al. MR imaging of neoplastic central nervous system lesions: review and recommendations for current practice. AJNR Am J Neuroradiol. 2012; 33:803–817. Omuro, A. M., Leite, C. C., Mokhtari, K., et al. Pitfalls in the diagnosis of brain tumours. Lancet Neurol. 2006; 5(11):937–948. Tang, Y. Z., Booth, T. C., Bhogal, P., et al. Imaging of primary central nervous system lymphoma. Clin Radiol. 2011; 66:768–777.
Skull and brain
Indications for MRI in suspected stroke
CT
MRI
Causes
Diagnosis and investigation
Presentation
Diagnosis
Malformations with AV shunts
Malformations without AV shunts
Meningitis
Encephalitis and encephalitis-like disorders
Slow viruses
Prion diseases
Infections
Viral
Primary effects
Secondary effects
Delayed effects
Hyperdense
Skull and brain