Skull-Base Trauma
9.1 Introduction
Skull-base trauma is an important cause of long-term neurologic sequelae, permanent disability, and death. Because of the complex anatomy at the skull base, the initial injury can result in various complications, ranging from cranial nerve deficits to devastating vascular injury.1 Recent advances in medical imaging have allowed for increased detection of subtle injuries in a rapid, noninvasive manner.
Fractures of the skull are reported in 3.5 to 24% of patients with head injury.2 Of patients with facial trauma, the overall frequency of skull-base trauma is 25%.3 In patients with trauma to the upper cervical spine, 23% will also have a fracture of the skull base.4 Hence, the presence of spinal or maxillofacial trauma predicts a higher likelihood of a skull-base fracture.
Computed tomography (CT) is the mainstay imaging modality in the initial assessment of patients with suspected skull-base trauma. Imaging of the skull base requires high-resolution axial images with coronal and sagittal reformats. The need for additional imaging is determined by the clinical scenario and the presence of injury. This may include a CT angiogram of the head and neck or magnetic resonance imaging (MRI) of the craniocervical junction to look for associated complications. MRI may also detect associated injuries, for example, spinal trauma or subtle intracranial injuries that are poorly delineated by CT, including diffuse axonal injury, brainstem trauma, and small cortical contusions. MRI is also useful for evaluation of long-term post-traumatic sequelae such as cranial nerve injury.
Conventional angiography plays a limited role in the immediate assessment of skull-base trauma, but it may be helpful after initial imaging has been obtained to evaluate for traumatic vascular injury, especially if computed tomographic angiography (CTA) is limited or equivocal. Vascular complications, such as an arteriovenous fistula, are often best evaluated on conventional angiography with the potential for immediate endovascular intervention. Skull x-rays play a limited role in evaluation for trauma at the skull base.5 Underlying brain parenchymal injury or vascular injury is not evaluated on skull x-rays, and the presence or absence of a skull fracture does not adequately predict concomitant injuries.
9.2 Imaging Technique
For the diagnosis of skull-base trauma, CT is the mainstay modality. In addition to a routine head CT (5-mm axial slices), high-resolution images through the skull base are needed to evaluate skull-base injury (1- to 3-mm axial slices). Coronal reformations are helpful to further evaluate 1 to 2-mm subtle fracture lines and are especially helpful in evaluating the superior orbital roof and petrous bone. If there is clinical suggestion of a temporal bone fracture or suspicious findings on standard CT (such as mastoid fluid in the setting of trauma), dedicated images through the temporal bone in thin sections (1- to 2-mm-thick axial slices with coronal and sagittal reformations) with a reduced field of view using bone reconstruction algorithms are necessary. Contrast is not necessary for evaluation of osseous trauma.
Often, CTA is obtained after noncontrast imaging to evaluate for vascular injury. The use of both coronal and sagittal reformations is important, as subtle injury can be missed in one imaging plane but better appreciated on another.
9.3 Clinical Presentation
Depending on the underlying injury, patients may exhibit various signs on physical examination. Some clinical signs suggest the location of the skull fracture. Fractures of the anterior skull base may initially manifest as rhinorrhea, raccoon eyes (periorbital ecchymosis), anosmia, and visual changes. Fractures of the middle skull base, particularly those involving the petrous temporal bones, can manifest as hemotympanum (blood in the middle ear), blood in the external auditory canal, vestibular changes, Battle’s sign (retroauricular hematoma), facial paralysis, CSF otorrhea, or strabismus. Fractures of the clivus and posterior skull base may present as craniocervical dissociation or brainstem dysfunction. Involvement of any aspect of the skull base can result in a cranial nerve deficit or vascular injury (especially of the petrous and cavernous portions of the internal carotid artery).
In cases of depressed skull fractures, a palpable abnormality may be felt at the site of the depressed fracture fragment. In open skull fractures involving the skin, there will be a visible soft tissue laceration.
9.4 Normal Anatomy
9.4.1 Cranial Fossae
The skull base anatomy is notably complex, comprising the ethmoid, sphenoid, frontal, temporal, and occipital bones.6 These bones each have a complex shape, and it is often easier to consider them together based on overall structure. One way to consider the skull base is as a cradle for the intracranial components. This cradle can be divided also into three regions: the anterior, middle, and posterior cranial fossae. This terminology is helpful to describe the location of an extra-axial hematoma, for example:
Anterior cranial fossa: Bounded anteriorly by the inner table of the frontal sinus, posteriorly by the anterior clinoid processes and the planum sphenoidale, and laterally by the frontal bone.
Middle cranial fossa: Bounded anteriorly by the anterior clinoid processes and posterior margin of the lesser wing of the sphenoid; posteriorly by the superior margin of the petrous temporal bone and dorsum sellae of the sphenoid bone; and laterally by the squamous temporal bone, parietal bone, and greater wing of the sphenoid.
Posterior cranial fossa: Composed mainly of the occipital bone; bounded anteriorly by the dorsum sellae and clivus, and laterally by the posterior aspect of the petrous temporal bone and the lateral aspect of the occipital bone. Some classification systems separate the clivus as the central skull base, as is done in this chapter.
Because fractures do not respect the anatomic borders of the cranial fossa, another way to consider the skull base when evaluating the results of trauma, particularly skull-base fractures, is to divide the skull base into four parts: the anterior, middle, central, and posterior skull base. Although fractures may involve more than one of these areas, traumatic injury can be categorized based on which of these four areas is primarily affected.
9.4.2 Anterior Skull Base
The anterior skull base consists of the crista galli, cribriform plate, fovea ethmoidalis (the roof of the ethmoid sinus), and orbital roofs.7 The cribriform plate is an important aspect of the anterior skull base, as it is the most inferiorly positioned aspect of the floor of the anterior skull base, and is not covered by dura. Thus, fractures of the cribriform plate may lead to development of a cerebrospinal fluid (CSF) leak. Immediately adjacent to the anterior skull base are the upper paranasal sinuses (sphenoid sinus, posterior walls of the frontal sinus, and roof of the ethmoid sinus).
9.4.3 Middle Skull Base
The middle skull base consists of the sella turcica and the floor of the middle cranial fossa. Major foramina within the middle skull base are the superior orbital fissure, foramen ovale, foramen rotundum, foramen spinosum, foramen lacerum, and the pterygoid (vidian) canal.
9.4.4 Central Skull Base
The central skull base consists of the clivus, which is formed by the basisphenoid and basiocciput.
9.4.5 Posterior Skull Base
The posterior skull base consists of the occiput and bilateral petrous ridges. Major foramina of the posterior skull base include the foramen magnum, hypoglossal canal, jugular foramen, carotid canal, and internal auditory canal.
9.5 Normal Fissures and Sutures
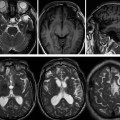
Cranial sutures consist of fibrous bands of tissue uniting the skull bones together.8 They are important sites of bone growth. Knowledge of the various sutures and their appearance on CT imaging is vital to avoid mistaking these normal structures for a nondisplaced fracture. Important sutures to consider include the following (▶ Fig. 9.1):
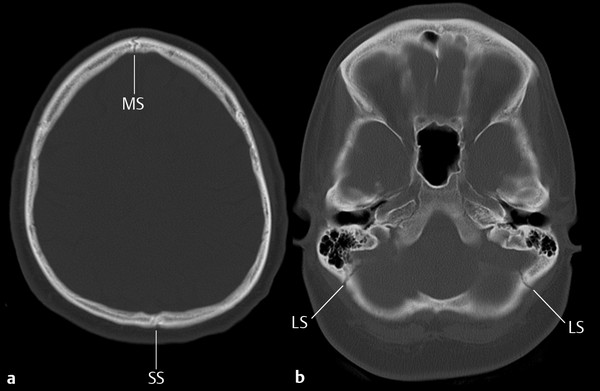
Fig. 9.1 Cranial sutures. Axial computed tomography of the skull (a) showing the metopic suture (MS), sagittal suture (SS), and (b), the lambdoid suture (LS).
Metopic suture: Interfrontal suture between the two frontal bones that usually fuses in childhood
Sagittal suture: Between the parietal bones
Coronal sutures (paired): Between the two frontal and two parietal bones
Lambdoid sutures (paired): Between the occipital and parietal bones
Squamosal sutures (paired): Between the parietal, temporal and sphenoid bones
Sphenosquamous suture: Between the posterolateral margin of the greater wing of the sphenoid and the anterior border of the squamous temporal bone
Occiptomastoid suture: Between the lateral aspect of the occipital bone and the superior mastoid part of the temporal bone
Cranial fissures are also an important aspect of skull base anatomy and may be mistaken for skull fractures. These include the petrosphenoidal and petro-occipital fissures.
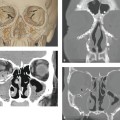
Skull-base trauma can involve the skull-base foramina (▶ Fig. 9.2). Patients can initially show various cranial nerve palsies. Knowledge of the various foramina and their location and contents is important to predict cranial nerve injury (▶ Table 9.1).
| Foramen | Contents |
| Optic canal | Cranial nerve (CN) II (optic) Ophthalmic artery |
| Superior orbital fissure | CN III, IV, V1, VI (oculomotor, trochlear, ophthalmic and abducens) Superior ophthalmic vein |
| Foramen rotundum | CN V2 (maxillary) |
| Foramen ovale | CN V3 (mandibular) Lesser petrosal nerve |
| Foramen spinosum | Middle meningeal artery |
| Vidian canal | Greater superficial and deep petrosal nerves (vidian nerve) |
| Jugular foramen | CN IX, X, XI (glossopharyngeal, vagus, spinal accessory, sympathetic nerve) |
| Internal acoustic meatus | CN VII, VIII (facial, vestibulocochlear) |
| Hypoglossal canal | CN XII (hypoglossal) |
| Foramen magnum | Brainstem Vertebral arteries |
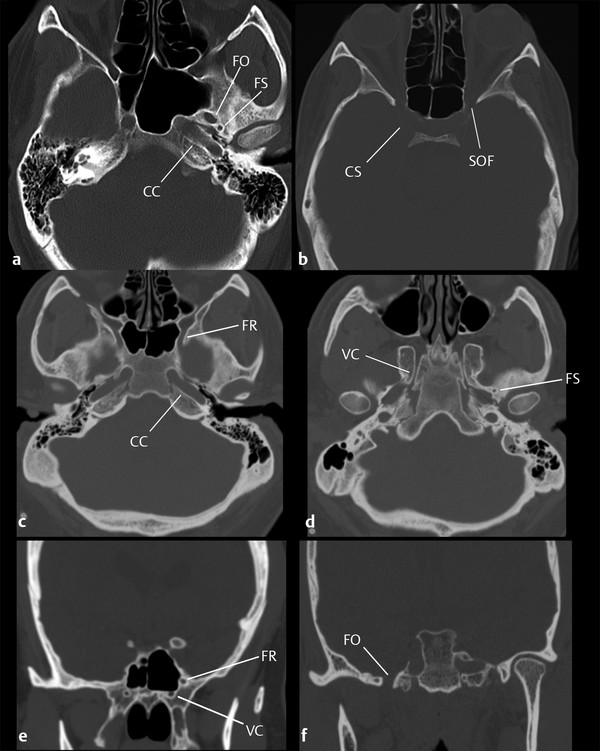
Fig. 9.2 Skull base foramina on computed tomography (CT). Axial CT images (a–d) and coronal reformat (e,f) demonstrate the foramen ovale (FO), foramen spinosum (FS), carotid canal (CC), superior orbital fissure (SOF) cavernous sinus (CS), foramen rotundum (FR), vidian canal (VC)
In pediatric patients, the appearance of developing bones and unfused cranial sutures may be confused with a fracture, and knowledge of these normal age-related variations is crucial to avoid misdiagnosis. Most of the skull-base forms by endochondral ossification.9 Ossification begins in the occipital bones and continues anteriorly.10 Evaluating symmetry often aids in determining whether a finding is a true fracture versus normal ossification of the cartilaginous skull base.
The skull base of an infant contains many synchondroses (▶ Fig. 9.3). The major synchondroses are the intersphenoid, spheno-occipital, frontosphenoidal, and posterior occipital. Accessory synchondroses are also possible along cranial sutures. In addition, the newborn and young infant skull contains fontanelles (anterior, posterior, and lateral).
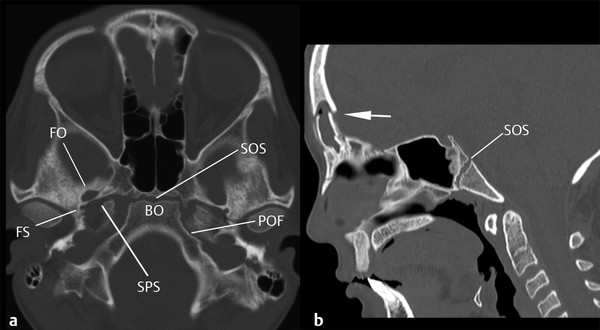
Fig. 9.3 Pediatric skull. Axial computed tomography of the skull base (a) with sagittal reformat (b) in a child with frontal sinus fractures (arrow) demonstrates the spheno-occipital synchondrosis (SOS), basiocciput (BO), petrooccipital fissure (POF), foramen ovale (FO), foramen spinosum (FS), and the sphenopetrosal synchondrosis (SPS).
In the evaluation of skull-base trauma, it is important to recognize the spheno-occipital synchondrosis, located at the junction of the sphenoid and occipital bones. It usually fuses by age 18 years.11 Closure occurs from above, and a thin sclerotic scar often persists into adulthood. Incomplete closure of the spheno-occipital synchondrosis is possible and is a site of weakness with a higher predisposition to fracture.
9.6 Fractures of the Anterior Skull Base
Fractures of the anterior skull base are often associated with maxillofacial trauma. Fractures may involve the cribriform plate, fovea ethmoidalis (▶ Fig. 9.4), sphenoid sinus (▶ Fig. 9.5), and the orbital plate of the frontal bone or the walls of the frontal sinuses (▶ Fig. 9.6). Frontal sinus fractures are described more fully in Chapter ▶ 10, Maxillofacial Trauma, of this book. Evaluation for associated orbital injury, either intraconal, extraconal, or involving the globe, is key, as is detecting involvement of the optic canal. Orbital injuries are more fully described in Chapter ▶ 11, Traumatic Orbital Injury.
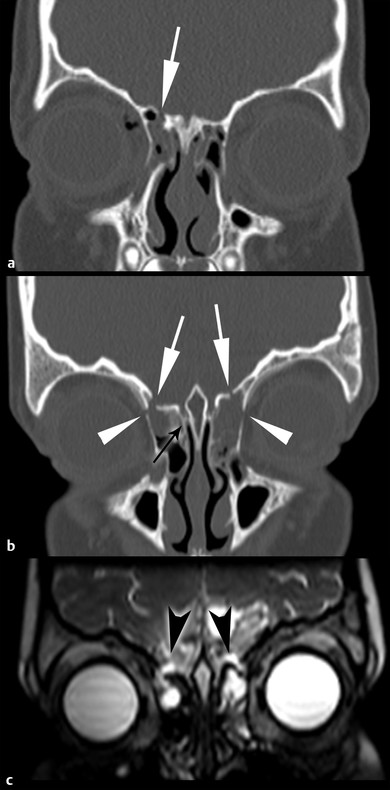
Fig. 9.4 Fractures of the fovea ethmoidalis. Coronal computed tomography (CT) (a) shows a fracture through the roof of the right ethmoid sinus (fovea ethmoidalis, white arrow) associated with a right orbital roof fracture (not shown). Coronal CT in a different patient (b) shows bilateral fractures of the fovea ethmoidalis (white arrows) associated with fractures of the medial orbital walls (white arrowheads). Note that the cribiform plate is spared (black arrow). High-resolution T2-weighted image (c) demonstrates cerebrospinal fluid (CSF) leaks (black arrowheads), manifested as T2 hyperintense CSF on either side of the fracture lines.
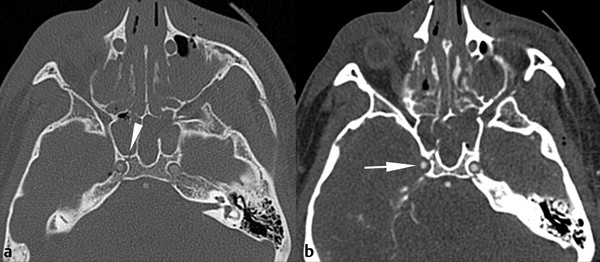
Fig. 9.5 Fractures of the sphenoid sinus. (a) Axial computed tomography (CT) shows a fracture through the posterior wall of the right sphenoid sinus extending through the anterior wall of the adjacent carotid canal (arrowhead). Additional maxillofacial injuries are present. CT angiography at the same level (b) demonstrates slight narrowing of the right internal carotid artery compared with the left (arrow), consistent with a Denver grade I injury.
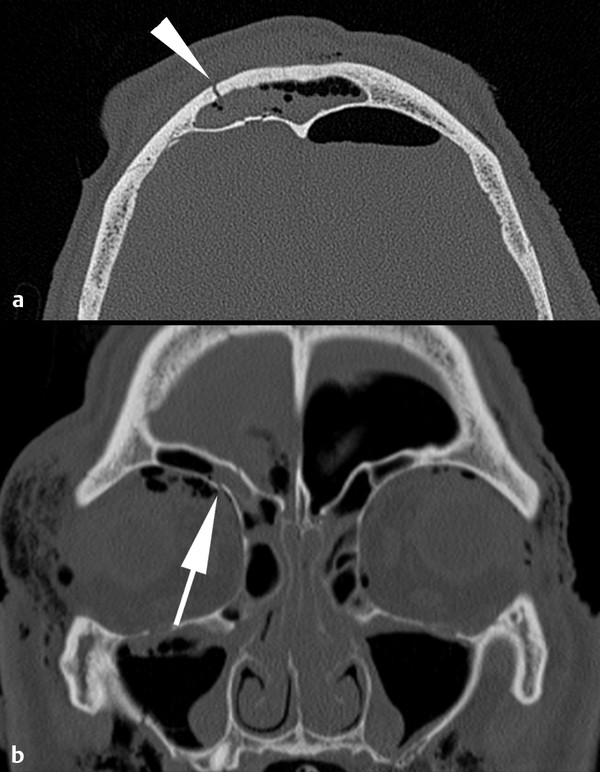
Fig. 9.6 Fractures of the anterior skull base with orbital involvement. (a) Axial computed tomography demonstrates fractures of the inner and outer table of the frontal sinus (arrowhead) with pneumocephalus. Coronal reformat (b) shows extension into the right orbital roof (arrow), in addition to other sinus fractures and extensive subcutaneous and orbital emphysema.
9.6.1 Classification
Reporting fractures of the anterior skull base is best done in a descriptive manner, describing the specific bones involved and extent of injury. In the neurosurgical literature, Sakas et al have described a classification system that is helpful in understanding the various types of injuries that may affect the anterior skull base. Although fractures of the anterior skull base are not usually classified radiographically by this system, it provides a framework on which to consider anterior skull-base fractures. Four fracture types are described:12
Type I: Cribriform fracture. This fracture extends through the cribriform plate but does not involve the ethmoid or frontal sinuses.
Type II: Frontoethmoidal fracture. This fracture extends through the walls of the ethmoid or medial walls of the frontal sinus and involves the medial portion of the anterior skull base.
Type III: Lateral frontal fracture. This fracture extends through the lateral aspect of the frontal sinus through the superomedial aspect of the orbit.
Type IV: Complex fracture. This type of fracture describes a complex injury involving any of the injuries classified in types I through III (▶ Fig. 9.7).
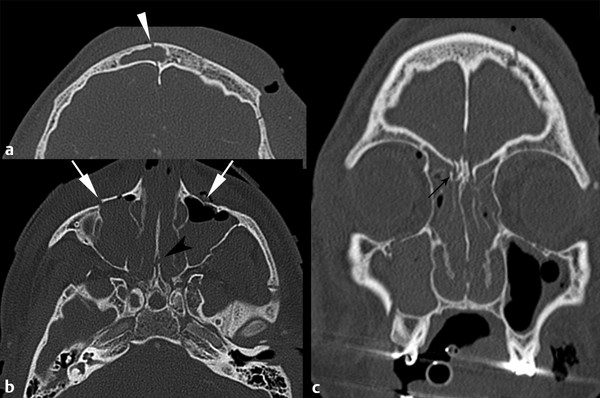
Fig. 9.7 Complex anterior skull base fractures. Axial images (a,b) demonstrate fractures through the frontal bones with involvement of the inner and outer tables of the frontal sinus (arrowhead) (a), with fractures through the bilateral maxillary sinuses (arrow) (b) and nasal septum (arrowhead) (b). Coronal reformat (c) shows fracture line through the right cribriform plate (black arrow).
9.6.2 Associated Injuries
When evaluating anterior skull-base fractures, always consider what secondary injuries may be present. For example, extension of a fracture into the petrous carotid canal necessitates evaluation of the carotid artery for injury (▶ Fig. 9.5). Fractures extending into the orbit require careful assessment of orbital complications (▶ Fig. 9.6). Certain anterior skull-base fractures, particularly those of the cribriform plate and fovea ethmoidalis, are associated with CSF leaks (▶ Fig. 9.4). Fractures involving both the inner and outer table of the frontal sinus may result in a CSF leak. Additionally, inner-table fractures may require surgical evaluation and treatment resulting from communication between the paranasal sinuses and the intracranial compartment, with a potential for intracranial infection, intracranial hemorrhage, and delayed mucocele formation. This topic is discussed further in Chapter ▶ 10, Maxillofacial Trauma. With significant fractures, even without direct petrous carotid canal involvement, vascular injury is an important entity to exclude (▶ Fig. 9.8).
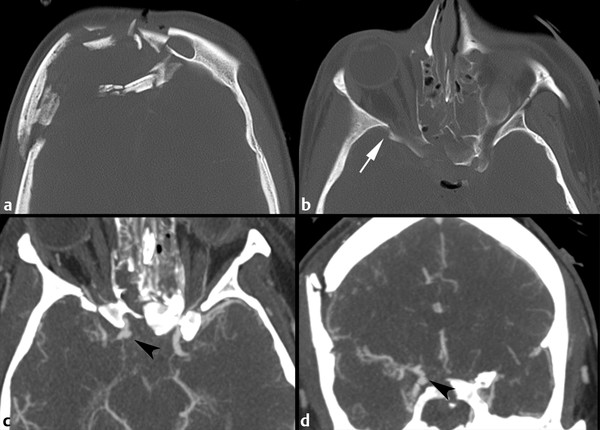
Fig. 9.8 Vascular injury associated with fractures of the anterior skull base. (a) Axial computed tomography (CT) shows a severely depressed comminuted fracture of the right frontal bone. The fracture extended into the right greater wing of the sphenoid (arrow) (b) and involved the ethmoid and sphenoid sinus walls. Axial CT angiography (c) with and coronal reformats (d) shows a traumatic right internal carotid artery pseudoaneurysm (arrowheads), which subsequently continued to enlarge and ultimately required obliteration.
9.6.3 Treatment
Treatment of fractures of the anterior cranial fossa depends on the extent of injury. Emergent surgery may be indicated for open or significantly depressed fracture, foreign bodies, or to decompress the optic canal.13 Dural repair may be needed to avoid or close a post-traumatic CSF leak and to prevent intracranial infection. CSF leaks sometimes close without direct repair after ventricular drainage, such as with a lumboperitoneal shunt. Vascular injuries may require endovascular or surgical care. Cosmesis is an important consideration in long-term management.
9.7 Fractures of the Central Skull Base
9.7.1 Clival Fractures
Detection of clival fractures has increased with the use of CT and improved image resolution. These fractures are often associated with other craniofacial trauma. Neurologic prognosis in patients with clival fractures is poor, and the mortality rate is high, up to 24%.14 Fracture of the clivus indicates a severe mechanism of injury, and clinical outcome is correlated to the patient’s initial Glasgow Coma Scale score and associated injuries.15
Classification
Clival fractures can be classified into three types, depending on the orientation:
Longitudinal fractures extend from the sphenoid body to the foramen magnum in the anteroposterior direction.
Transverse fractures extend from right to left (usually one carotid canal to the other).
Oblique fractures extend at an angle through the clivus, traversing the lateral aspect of the dorsum sellae toward the contralateral petroclival fissure (▶ Fig. 9.9).
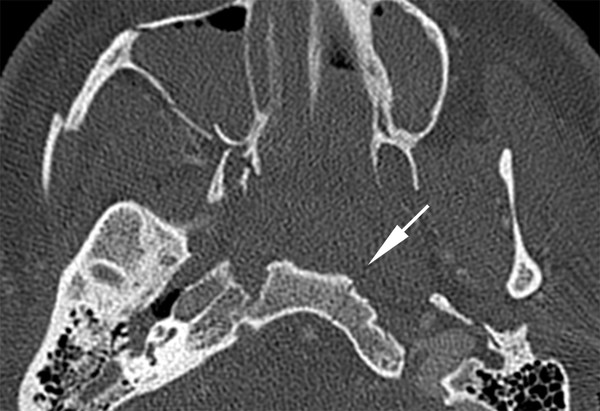
Fig. 9.9 Fractures of the clivus. Axial computed tomography angiography image demonstrates nondisplaced oblique fracture through the left aspect of the clivus (arrow). Associated craniofacial fractures (right medial pterygoid plate, right zygomatic arch, and walls of the right maxillary sinus) are also present.
Associated Injuries
Fractures of the clivus are associated with significant morbidity and mortality owing to the proximity of important neurovascular structures. Longitudinal fractures have the highest rate of mortality from associated injuries. Vascular injuries, including dissection and pseudoaneurysm, may affect the vertebrobasilar system (longitudinal fractures) or carotid circulation (transverse fractures), with a reported incidence of up to 46%.16 A traumatic carotid-cavernous fistula may develop acutely or in a delayed fashion. Although rare, longitudinal fractures of the clivus can result in incarceration of the basilar artery.17
Additional injuries associated with clivus fractures include pituitary dysfunction, injury to the brainstem, CSF leaks, and cranial nerve deficits. The sixth cranial nerves in particular are susceptible to injury, as they are fixed by their course through Dorello’s canal in the clivus. Cranial nerves III, IV, V, and VII may also be injured in association with clivus fractures because of their close proximity.
Treatment
Fractures of the clivus are often associated with other injuries and are associated with various complications. Treatment is best achieved via a multidisciplinary approach that initially targets life-threatening complications such as vascular injury.
9.8 Fractures of the Posterior Skull Base
9.8.1 Fractures of the Occipital Bone
Fractures of the occipital bone can be nondisplaced, displaced, or comminuted; they can also be classified as closed or open (▶ Fig. 9.10). A ring fracture of the skull base is a specific type of occipital skull fracture that is particularly associated with motorcycle accidents.18 The fracture is orientated in the transverse plane and encircles the foramen magnum. This injury is important because it can result in severe vascular and parenchymal injury.
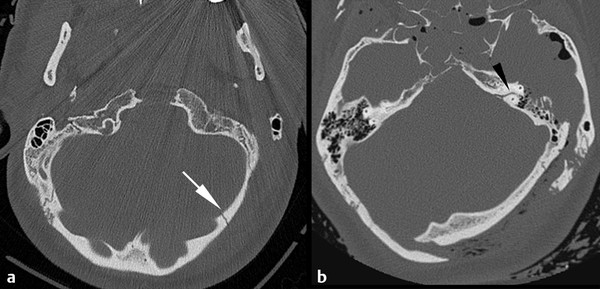
Fig. 9.10 Spectrum of occipital bone fractures. Axial computed tomography (CT) through the posterior fossa (a) demonstrates a nondisplaced left occipital bone fracture (arrow). This patient had no other intracranial injuries. Axial CT in a second patient (b) demonstrates markedly depressed fracture of the left occipital bone extending into the petrous left temporal bone. Venous injury and otic capsule fracture (arrowhead) are of high concern and must be evaluated.
Associated Injuries
Some fractures of the occipital bone are isolated injuries. Others are associated with other osseous trauma, including occipital condyle fractures, cervical spine fractures, and central skull-base trauma. Careful evaluation for an underlying extra-axial hematoma is key. If the fracture is near a venous sinus, dural venous sinus thrombosis or injury must be excluded (▶ Fig. 9.11).
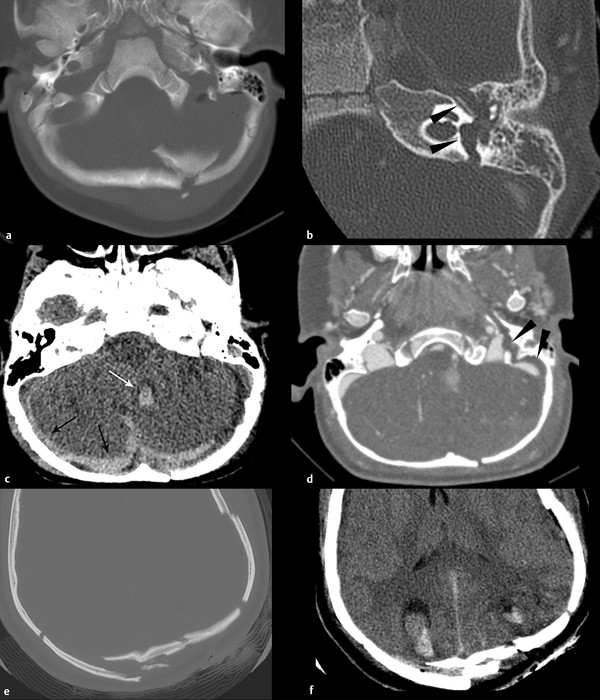
Fig. 9.11 Complications of occipital bone fractures. Axial computed tomography (a) shows a comminuted occipital bone fracture. Associated injuries included (b) transverse fracture of the left temporal bone (black arrowheads), (c) parenchymal hemorrhage (white arrow) and subdural hemorrhage (black arrow). There is extrinsic compression of the left sigmoid sinus (d) (black arrowheads). In a different patient, comminuted and depressed fractures of the occipital bones (e) are associated with underlying hemorrhagic contusions (f).
Extra-axial hematomas may result in compression of an adjacent dural venous sinus. CT venography is helpful to exclude extrinsic dural venous sinus compression and direct venous injury. Magnetic resonance venography may also be considered if the patient is clinically stable to undergo MRI scan. Parenchymal and extra-axial hemorrhages may result in sufficient mass effect to cause tonsillar herniation or upward tentorial herniation. If associated brainstem compression is severe, decompressive surgery may be required. Additionally, if there is significant mass effect on the fourth ventricle, hydrocephalus may develop.
Contrecoup frontotemporal injury accounts for significant mortality and morbidity associated with fractures of the occipital bone (▶ Fig. 9.12). Careful attention to areas of potential contrecoup injury is required to find subtle injuries, including contrecoup parenchymal hematomas and extra-axial hemorrhages. Sites of involvement include the medial subfrontal and anterior temporal locations.
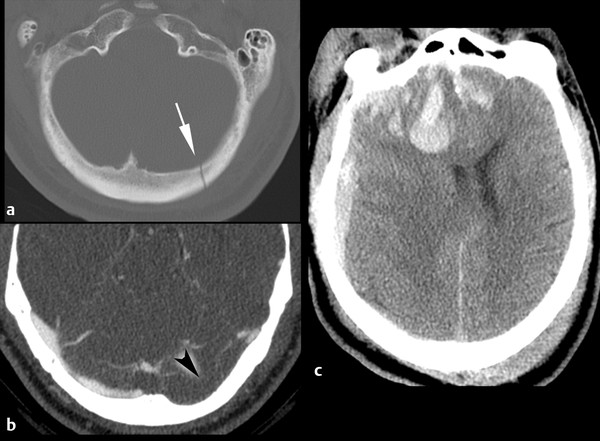
Fig. 9.12 Frontotemporal contrecoup injury after occipital bone fracture. Noncontrast computed tomography (CT) demonstrates nondisplaced fracture of the left occipital bone (a) (arrow
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree