Penetrating Traumatic Brain Injury
8.1 Introduction
The remarkable Phineas Gage, a railroad foreman in 1848, was fortunate to survive an accidental transcranial impalement with his tamping iron, a metal bar more than an inch in diameter and about 3.5 feet long (used to compact sand over a rock-breaking explosive charge). The accidental missile entered lateral to Mr. Gage’s face and exited through his superior cranium. The case is notable for, among other things, how improbable his survival was. Even in the modern setting, penetrating traumatic brain injuries are frequently catastrophic. Modern computed tomography (CT) has become an essential tool for characterizing similar injuries (the first radiograph would not be invented until decades after Mr. Gage’s death in 1860, although Ratiu and Talos recently redemonstrated the injury quite well).1 Both acute and follow-up imaging of such injuries is standard of care for diagnosis, assessment of the need for intervention, prognosis, and related complications. Considerations for imaging after penetrating traumatic brain injury are discussed here, including special consideration of gunshot wounds (GSWs) to the head and wood impalement, the latter because of the significant risk of misdiagnosis with CT imaging.
8.2 Acute Imaging
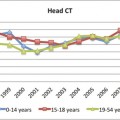
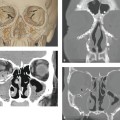
As with all head trauma, the initial imaging study of choice for a penetrating injury is a noncontrast CT of the head.2–4 This evaluation should include evaluation of the frontal and lateral scout views (▶ Fig. 8.1). Scouts are particularly important in the case of GSW because they provide general orientation to the injury and localization of metallic fragments. Plain radiographs of the head are of limited usefulness.4,5
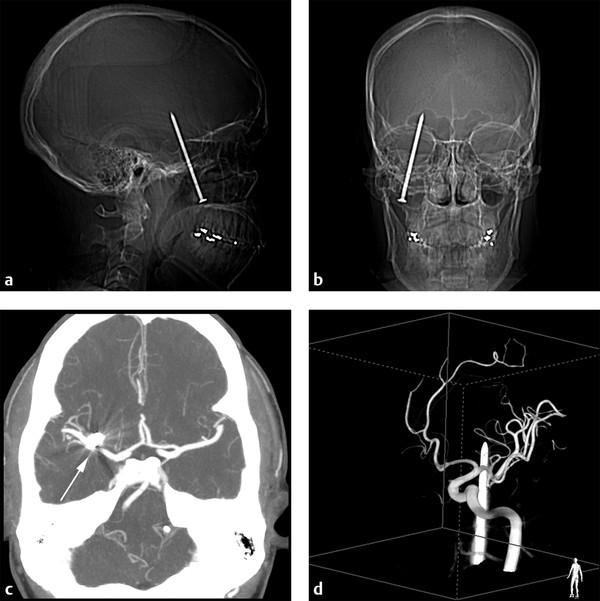
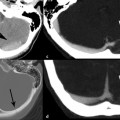
Fig. 8.1 Severe jaw pain and normal neurologic examination 24 hours after an unsuspected injury sustained while using a nail gun: (a,b) Scout images from the computed tomography (CT) show the nail that entered under his zygoma, passed through the mouth, and penetrated the brain. (c) The nail is visible immediately anterior to the right M1 segment (arrow) on the CT angiogram maximum intensity reconstruction. (d) Three-dimensional rotational angiographic reconstruction from the right posterior oblique view shows the nail passing in close proximity to the M1 segment of the middle cerebral artery. Vascular structures were also normal on follow-up angiography following removal of the nail.
In assessing penetrating injury, regardless of cause, the location of all large bone fragments and foreign material should be noted.6 Any superficial injuries with possible intracranial extension should be assessed carefully for the presence of pneumocephalus.3 Intracranial injuries may include herniation (uncal, subfalcine, upward and downward transtentorial), cisternal effacement, ventricular compression, and parenchymal injury. Identification of hemorrhage in any intracranial space is important for both the possible mass effect and the identification of any significant vascular injury (▶ Fig. 8.2).7
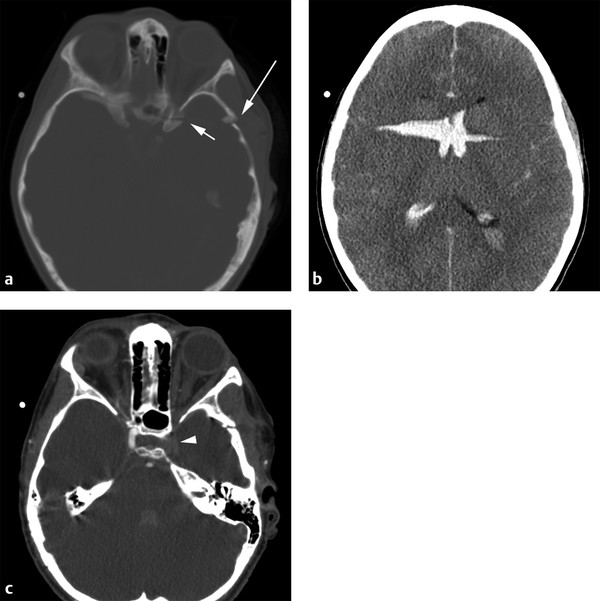
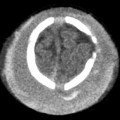
Fig. 8.2 Seven-year-old boy with a penetrating knife wound to the head: (a) There was disruption of the squamosal portion of the left temporal bone (long arrow) and fracture of the left anterior clinoid (short arrow). (b) Axial noncontrast computed tomography (CT) shows diffuse brain edema and diminished gray-white differentiation. Blood was present in the wound tract and passed through both lateral ventricles. (c) CT angiogram revealed no flow in the left cavernous internal carotid artery (arrowhead). The patient had no spontaneous movement, and care was withdrawn.
With penetrating head trauma, computed tomography angiography (CTA) of the head and neck is frequently valuable, particularly when the suspected injury is close to cervical or intracranial vasculatures. It is considered by the American College of Radiology that the appropriate criteria is as “usually appropriate,” at seven of nine on a nine-point scale of appropriateness. By comparison, the noncontrast head CT has a nine in nine recommendation strength.4 If the CTA is not obtained at the time of original imaging, recommendation for CTA or conventional angiography should be made when there appears to be risk of injury to any major vessels.3,5–8 This is true when the bullet, nail, knife, umbrella, chopstick, or other object passes through or adjacent to the skull base, the carotid siphons, or any of the named intracranial vessels, including the dural venous sinuses.5,6 The CTA is essential for preoperative planning before any attempted removal of an impaled object or missile.
The CTA may also be recommended at subsequent intervals to assess for arterial vasospasm.7 In a series of 33 patients with penetrating gunshot wounds to the head, 14 demonstrated evidence of middle cerebral artery vasospasm by transcranial Doppler criteria (performed 0 to 33 days after injury). These findings were also significantly associated with the presence of subarachnoid hemorrhage on the initial head CT evaluation.9
Skull-base injuries have a high likelihood of vascular injury, of cranial nerve injury, and of cerebrospinal fluid (CSF) leak. In Shindo and coleagues’ series of 43 patients with GSW to the head involving the temporal bone, 51% demonstrated facial nerve injury, and 33% demonstrated vascular injury. Six of 43 patients (14%) also suffered a CSF leak.10 A CSF leak is important to identify for a number of reasons, including the increased risk of infection: as high as 31% in patients with a known post-traumatic CSF leak.11 CT cisternography may be the most appropriate and sensitive technique for identifying a fistula or leak,5,12 although the utility of radionuclide cisternography has also been demonstrated.13 Magnetic resonance (MR) cisternography is difficult in the acute penetrating trauma patient because MR imaging may be contraindicated if the retained metallic object is ferromagnetic.
In the acute setting of penetrating injury, MR imaging is rarely used. It is certainly to be avoided whenever any part of the penetrating object(s) may contain ferromagnetic material, given the risk of significant migration of metal fragments while the patient is within the magnet. Although most bullets in civilian penetrating brain injury do not contain ferromagnetic material, the inevitable lack of certainty about this limits MR use.5 MR can be more sensitive than CT for retained wood,14,15 although this may depend on how long the wood has been present. At the time of initial injury, wood is usually near air density. Wood may become hydrated with increasing time in place, making its identification with either CT or MR easier.16
Conventional angiography is the gold standard for assessment of vascular injury, both for acute vascular injury and for late-developing complications. It is essential in the diagnosis and characterization of traumatic intracranial aneurysms and arteriovenous fistulae (▶ Fig. 8.3 and ▶ Fig. 8.4). This modality is also superior to CT in the presence of metal because of the presence of streak artifact on CT. Additional indications for conventional angiography include evidence of arterial extravasation and unexpected delayed hemorrhage.7,8
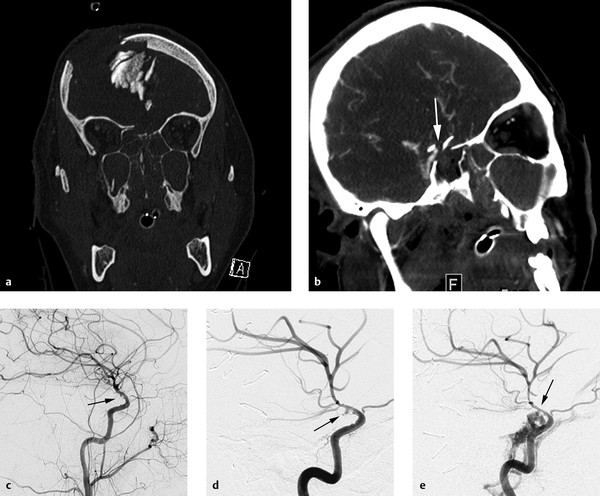
Fig. 8.3 An 18-year-old patient after a high-speed motor-vehicle collision with complex skull-base fractures, depressed frontal bone fractures and right internal carotid artery (RICA) injury: (a) Initial coronal computed tomography (CT) reformation demonstrates a fracture of the planum sphenoidale with upward displacement of the bone as well as massive inward displacement of the frontal bone into the cranial cavity. (b) Oblique coronal maximum-intensity projection from the initial CT angiogram shows the anatomic proximity of the fracture in the planum sphenoidale to the RICA (white arrow). (c) RICA injection from the catheter angiogram on admission demonstrates a narrowed and irregular supraclinoid segment of the RICA consistent with a dissection (black arrow). The irregularity was concerning for a pseudoaneurysm. (d) RICA injection from a catheter angiogram 2 weeks after admission shows enlargement of the pseudoaneurysm in the supraclinoid RICA (black arrow). (e) RICA injection from a catheter angiogram 1 week later now demonstrates a carotid-cavernous fistula arising from the RICA (black arrow). In the studies at 2 weeks (d) and 3 (e) weeks after injury, the right anterior cerebral artery no longer filled from the RICA.
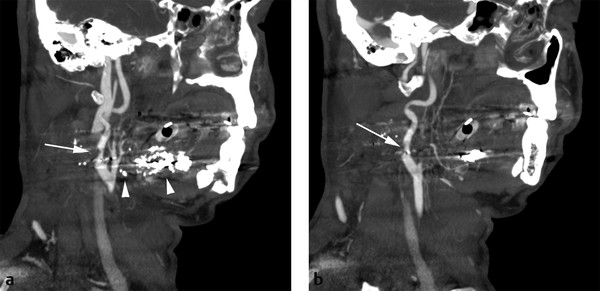
Fig. 8.4 Gunshot wound (GSW) to the neck. (a,b) These are two oblique maximum-intensity projection images through the right common internal carotid artery (ICA) bifurcation. Bullet fragments were present (arrowheads), as well as an injury to the proximal right ICA (arrows). This appears equivalent to a Biffl type II injury, although the Biffl classification was created in the setting of blunt, and not penetrating, trauma. The more proximal common carotid artery is patent but not present on these slices.
8.3 Gunshot Wounds to the Head
In the trauma literature, GSWs to the head are frequently separated into civilian and military injuries. One of the major reasons for this is their significantly different ballistics and mortality rates. Penetrating brain injuries in the military setting are also frequently collections of all penetrating missiles, artillery shrapnel, bullets, and such, and these injuries have lower mortality rates. In one case series of 964 patients involved in the Iran-Iraq War of the 1980s, overall mortality was just 14% (133 patients).17 Multiple series from urban settings in the United States have very different results. These have demonstrated that most civilian GSW to the head are fatal and never reach trauma centers for evaluation or care,18 and many that do reach trauma centers are not survivable. In one series of 250 cases of GSW to the head from Maryland, 71% died at the scene, and the total mortality was 89%.7 Of the patients who reach trauma centers, most have a Glasgow Coma Scale score of 8 or lower,7 limiting physical examination and increasing the relative importance of diagnostic imaging.
8.3.1 Ballistics
Bullets entering the scalp frequently devitalize the adjacent soft tissue. If the gun barrel is very near the scalp, propellant gas may be demonstrated in layers of the scalp near the entrance wound. Despite the heat of a fired bullet, the wounds are frequently contaminated by skin, hair, fabric, and superficial flora. Prophylactic antibiosis is the standard of care. The offending bacteria in subsequent intracranial infections have been frequently identified as contaminating skin flora.7
Cranial fracture and fragmentation are highly variable. Small-bore entrance fractures can be seen as well as large stellate fracture patterns involving much of the cranial hemisphere. If the bullet exits the cranium, the exit wounds tend to be larger than the entrance wounds. The beveled edge of the cranium frequently indicates the direction of bullet passage. That is, the wider opening of the bevel at the inner table of the skull facing the intracranial compartment is suggestive of the entrance wound (▶ Fig. 8.5).6
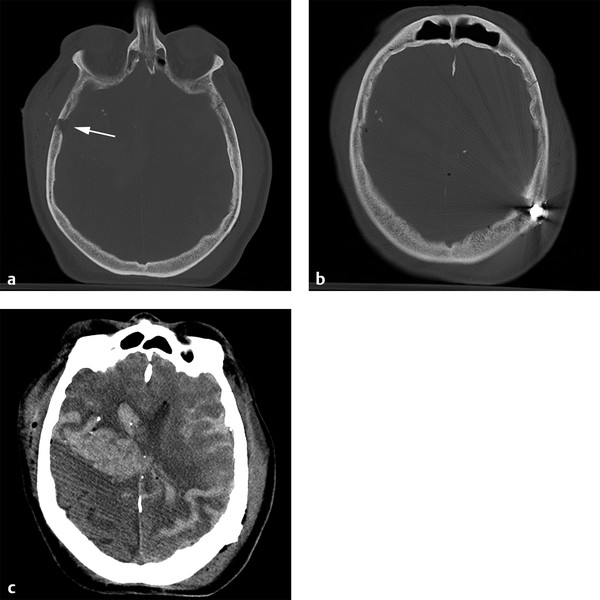
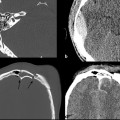
Fig. 8.5 Self-inflicted gunshot wound with 0.22-caliber bullet: (a) Computed tomography with bone kernel shows typical beveling of the entrance wound in the right temporal bone (arrow) and (b) the retained bullet fragment at the contralateral parietal cranium. (c) The bullet tract crosses the midline in the midcoronal plane with intraventricular hemorrhage. Patients with injury of this extent and pattern of intracranial involvement have little chance of survival.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree