Epidemiology of Traumatic Brain Injuries in the United States
1.1 Overall Incidence
Traumatic brain injury (TBI) is one of the leading causes of injury-related mortality and morbidity worldwide.1–3 In the United States, more than 1.7 million people sustain a TBI each year.2 Of those, 1.4 million are treated and released from the emergency department (ED), more than 270,000 are hospitalized, and more than 53,000 die as a result of their injury.1–3 In Europe, 235 per 100,000 individuals sustain TBI annually.4 The World Health Organization estimates that by the year 2020, more than 10 million people will incur TBI annually worldwide.5 Between 2002 and 2006, an average of 100 million ED visits and 37 million admissions were reported each year, of which 3 and 5% were TBI related, respectively. During the same period, 30% of injury-related deaths in the United States were attributable to TBIs.5
Although no recent studies have evaluated the incidence of TBIs, Faul and Langlois demonstrated an increasing trend in the incidence of TBI-related ED visits and hospital admissions in the United States from 2002 through 2006.5,6 The incidence of TBI-related ED visits increased from 401 to 468 per 100,000, and the hospitalization rate increased from 86 to 94 per 100,000.5,6
1.1.1 Children
For the pediatric population, TBIs are of special importance because of their high incidence compared with other disabling diseases as well as their lifetime consequences.7 In the United States, each year, more than 600,000 emergency department visits, 60,000 hospitalizations, and 6000 fatalities in patients aged 0 to 20 years are attributed to TBIs. 5,8,9 ▶ Fig. 1.1 summarizes the TBI-related ED visits, hospitalizations, and deaths from 2002 to 2006 according to age group based on the study performed by Faul and colleagues.5
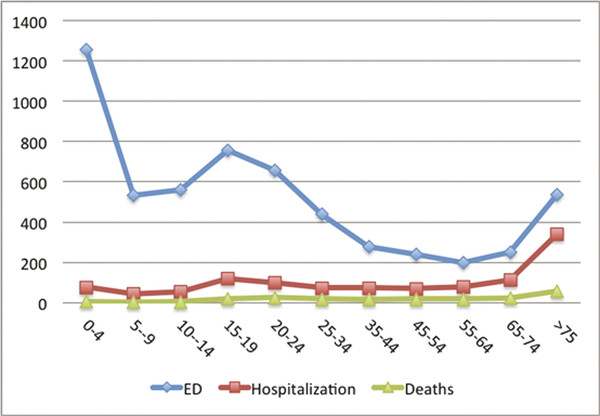
Fig. 1.1 Estimated average annual rates of traumatic brain injury–related emergency department (ED) visits, hospitalizations, and deaths by age group using the U.S. population in 2000 as the baseline for rate calculation, United States, 2002–2006.
(Used with permission from Faul MXL, Wald MM, Coronado VG. Traumatic Brain Injury in the United States, Emergency Department Visits, Hospitalizations and Deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.)
1.1.2 Older Adults
Whereas recent studies suggest that the incidence of TBIs in children and young adults has decreased as a result of the implementation of injury-prevention programs, the opposite is true for older adults.10 The aging of the population, the growing number of senior drivers, multidrug use by seniors, and the risk of drug-related falls are among the factors contributing to the increasing incidence of TBIs in the older adult population.11,12 Besides being at higher risk for TBIs compared with younger patients, older adults are more susceptible to detrimental consequences of TBI, such as longer hospital stays, a higher rate of intensive care unit admissions, higher mortality rates, and poorer functional status at discharge after a moderate to severe TBI.13–17
1.1.3 War Veterans
It is well known that military personnel are susceptible to TBI, but since the September 11, 2001, attacks, the types of TBIs among soldiers have changed. A large number of U.S. soldiers in the Afghanistan and Iraq Wars have been exposed to new generations of explosives.18 Because of advances in body-armor technology, faster evacuations from the scene of injury, and improvements in surgical care, the “at-scene” fatality rate has decreased, but the number of soldiers surviving disastrous TBIs while sustaining substantial disabilities has increased.18–21 Because of the high frequency of TBIs in recent wars, they are considered the “signature injury of modern military operations.” The Departments of Defense and Veterans Affairs have adopted special strategies to screen for TBIs, especially for veterans of the Afghanistan and Iraq Wars.18,22
1.2 Risk Factors
Among adults in the United States, alcohol is the most important modifiable risk factor for injuries, including TBIs.23 The incidence of alcohol-related injuries has not decreased significantly in the past two decades, although alcohol-related driver fatalities remained relatively unchanged between 1999 and 2006, as reported by Roudsari et al.23
In recent years, the use of mobile devices has become an increasingly significant contributor to road-traffic crashes resulting in TBI.24 A large study conducted in the United States and Europe revealed that among drivers 18 to 64 years of age, the prevalence of talking on a cell phone or using a mobile device for texting and e-mail while driving at least once in the past 30 days ranged from 21% in the United Kingdom to 69% in the United States. Distracted driving has become one of the most significant risk factors for TBI. Similarly, the use of mobile devices contributes to an increased incidence of pedestrian injuries.25 When pedestrians use the Internet on a mobile device, their behaviors become significantly higher risk.
In the United States, the three major nonmodifiable risk factors for TBIs are age, sex, and race or ethnicity. Overall, children younger than 5 years are at the highest risk of TBI, followed by adolescents (i.e., 15 to 19 years) and adults 75 years and older.5 Older adults (both men and women) are at higher risk for TBI-related mortality.5 Similar to other types of injuries, men are at greater risk for TBI than women; in fact, about 60% of all TBIs are suffered by males.5 ▶ Fig. 1.2 illustrates TBI-related ED visits (▶ Fig. 1.2a), hospitalization (▶ Fig. 1.2b), and deaths (▶ Fig. 1.2c) based on age group and sex in the United States between 2002 and 2006.5
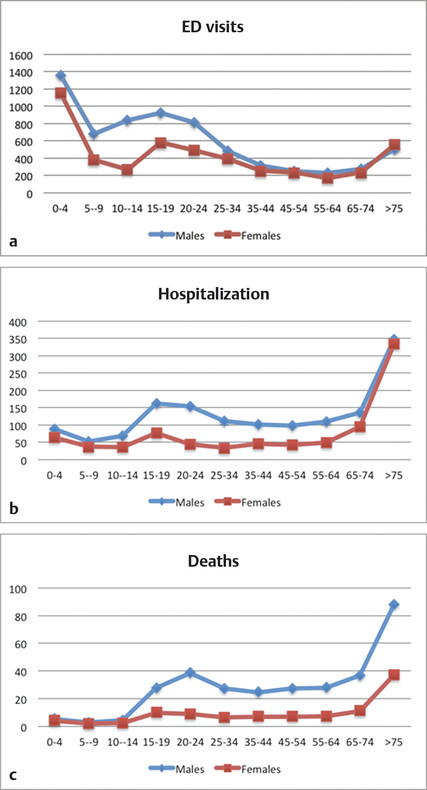
Fig. 1.2 Unadjusted emergency department (ED) visits (a), hospitalization (b), and mortality rates (c) per 100,000 for traumatic brain injuries in the United States, 2002–2006, categorized based on age group and sex using the U.S. population in 2000 as the baseline for the rate calculations.
From 2002 through 2006, African Americans had the highest unadjusted ED visit and hospitalization rates compared with whites and American Indians, Alaska Natives, and Asians (▶ Fig. 1.3) but slightly lower TBI-related mortality rates (16.7 in 100,000) than whites (18.2 in 100,000). American Indians, Alaska Natives, and Asians had the lowest TBI-related mortality rates (10.1 in 100,000).5
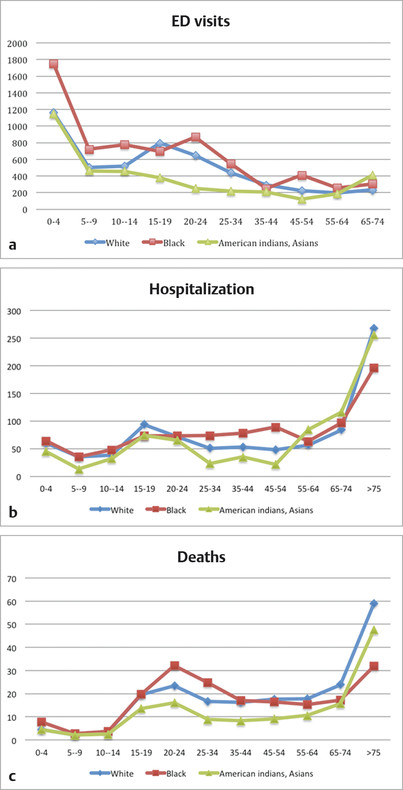
Fig. 1.3 Unadjusted emergency department (ED) visits (a), hospitalization (b), and mortality rates (c) for traumatic brain injury in the United States, 2002–2006, categorized based on age group and race or ethnicity using the U.S. population in 2000 as the baseline for the rate calculations.
1.3 Underlying Causes of Traumatic Brain Injury
The underlying cause of TBIs depends largely on the age group involved. For children and older adults, falls are the most common mechanism of TBI. For young and middle-aged adults, motor-vehicle or motorcycle collisions and assault are more prominent.5 Concussion, or so-called mild TBI (mTBI), is the most common cause of TBI among young athletes. Concussion proves increasingly complex to deal with and may not be “mild” as the name implies.26 This topic is discussed in detail in Chapter ▶ 12.
1.4 Short- and Long-Term Consequences of Traumatic Brain Injury
1.4.1 Mortality Rate
Most studies that have evaluated the effectiveness of preventive strategies for TBI have considered the mortality rate the main outcome of interest.27 Mortality is easy to measure and has a minimal chance of misclassification; therefore, it is an appealing target for most injury-prevention programs. Studies conducted by the Centers for Disease Control and Prevention have demonstrated that between 1989 and 2007, the TBI-related mortality rate declined from 21.9 in 100,000 to 17.8 in 100,000.2,28 However, not all age groups have experienced the same declining trend in mortality rates. Coronado and colleagues found that between 1997 and 2007, the mortality rate for TBIs decreased significantly among patients 0 to 44 years old but increased significantly among patients 75 and older.2 Recent analyses have shown men to be three times more likely to die of TBI-related causes (28.8 in 100,000) than women (9.1 in 100,000).2
1.4.2 Children
Multiple studies have discussed the neuropsychological consequences of TBIs among children.29–36 Previous studies suggested that reorganization of the brain after a TBI can minimize the short- and long-term consequences in a child’s “flexible” brain. However, new findings indicate that childhood injury could have more detrimental consequences than previously expected, not only because of damage to the available brain tissue, but also because of disruption of developmental milestones, which could interrupt the process of acquiring new skills at a developmentally appropriate rate.27,29,37–39 Pediatric neuropsychological impairments after a TBI can be categorized into two major categories: educational impairments and social or behavioral impairments.35,40,41 Studies have estimated that up to one third of children might require support into their adolescence and adulthood because of social and educational impairments.29
A number of studies have demonstrated that the severity of injury is likely the most important factor in predicting future functional impairment.31,37,42,43 The association between the severity of injury and functional impairments among mTBI patients remains open to debate. Although the vast majority of mTBI patients recover from injury, 15 to 20% suffer from reduced intellectual capabilities, attention disorder, memory impairment, linguistic problems, and academic failure in the postinjury years.30,36,37,42,44,45 Fewer longitudinal studies have expanded our knowledge in regard to the long-term consequences of TBI on child development. Rivara and colleagues followed up on 729 pediatric patients with moderate to severe TBIs for 2 years.27 They found that “the quality of life for children with moderate or severe TBI was lower at all follow-up times compared with baseline, but there was some improvement during the first 2 years after injury.”27
Anderson and colleagues conducted one of the few long-term follow-up studies of TBI patients.29 They found that after 10 years, the relationship between injury severity and cognitive impairment was most significant in the acute postinjury phase and much less evident 10 years later. Reports have conflicting conclusions about whether younger age at occurrence of the trauma is associated with poorer outcomes.29,43,46
1.4.3 Older Adults and Falls
Several studies have demonstrated higher mortality rates, longer hospital stays, and poorer functional outcomes in older adults compared with younger patients suffering from TBI.14,47–50 Older patients also need more intense rehabilitation to recover their functional status and prevent permanent disability after injury.50 Previous studies identified several risk factors for poor outcomes among older post-TBI patients, including but not limited to age,14,47,50 male sex, minority status,51 injury severity, comorbidities, and taking anticoagulation medication at the time of TBI.49
1.4.4 Other Long-Term Consequences
Quality of Life
Although objective measures such as length of hospital or intensive care unit stay and hospital expenses are easy to measure, they do not reflect the actual burden of TBIs on patients and their families. One factor often ignored in outcome studies is the quality of life after a TBI.52–54 Pagulayan and colleagues evaluated the quality of life of TBI patients at 1 month, 3 years, and 5 years after TBI by using the Quality of Life (QoL) Questionnaire.54
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree