Pediatric Head Trauma
5.1 Introduction
Pediatric head trauma is a major public health concern in the United States. It is a leading cause of acquired disability in children and accounts for more than 50,000 hospital admissions annually and a billion dollars in health care expenditure.1,2 The mechanism of head trauma varies by age; in those younger than 1 year, abusive head trauma is a major cause, and for those older than 1 year and less than 4 years, falls are the leading cause. Children older than 14 years are often the victims of motor-vehicle collisions.2,3 In the following sections, we identify and discuss issues related to radiologic evaluation of pediatric head trauma. We discuss general issues such as radiation dose, the identification of patients who need computed tomography (CT), broad issues such as birth trauma and nonaccidental trauma, and some more specific entities that are unique to children in the setting of trauma.
5.2 The Need for Head CT
After major head or multisystem trauma, noncontrast head CT is routinely used to evaluate for intracranial and calvarial injury. As in adults, head CT is considered the imaging study of choice in the acute phase after traumatic brain injury (TBI) to identify the presence and extent of structural damage. The head CT also provides essential diagnostic information for triage and cerebral resuscitation and generates immediate implications for surgical intervention.
For minor trauma, there is no widely accepted guideline in use. Efforts have been made with some success to define clinical decision-making guidelines. A guideline published in 2009 based on a large multicenter prospective patient population can be used to identify children at low risk for clinically significant injury.4 In children younger than 2 years, this low-risk group includes patients with Glasgow Coma Scale (GCS) 14 or 15; who do not have signs of basilar skull fracture; who do not have a history of loss of consciousness or vomiting, severe headache, or severe mechanism of injury. In children older than 2 years with a GCS of 14 or 15, no CT is recommended for those without palpable skull fracture, occipital or parietal scalp hematoma, less than 5 seconds’ loss of consciousness, or altered mental status.
The Canadian Assessment of Tomography for Childhood Head injuries (CATCH) guidelines were published in 2010 to identify signs or symptoms in children aged 0 to 16 years with a minor head injury who should get a CT and are undergoing prospective validation.5 CATCH comprises a list of seven entities, any of which should trigger a CT:
High risk (need for neurosurgical intervention):
GCS lower than 15 at 2 hours after injury
Suspected open or depressed skull fracture
Worsening headache
Irritability on examination.
Moderate risk (CT abnormality of brain injury):
Signs of basilar skull fracture (hemotympanum, “raccoon eyes,” CSF otorrhea or rhinorrhea)
Large boggy scalp hematoma
Dangerous mechanism (motor-vehicle collision, fall of more than 3 feet or more than five stairs, fall from bike without a helmet)
The first four criteria are high-risk factors and have a 100% sensitivity and 70% specificity for predicting the need for neurosurgical intervention. The last three criteria are moderate risk factors and have a 98% sensitivity and 50% specificity for predicting brain injury on CT.
5.3 Protocol and Dose
Because the head CT is the imaging study of choice for evaluating for TBI, the radiologist must be aware of the risk associated with pediatric radiation exposure. Children are inherently more sensitive to radiation than are adults, and radiation has greater potential to cause harm as children have more time to develop any delayed effects.6,7 Age is the most important factor when considering the effect of radiation exposure: children are up to 10 times more sensitive to radiation than adults, and the youngest neonates are more sensitive than the older child.8 The “as low as reasonably achievable,” or ALARA, principle (originally promulgated from the 1950s through the 1970s for nuclear reactor personnel safety9–11) has become a tenet of medical radiation safety: the lowest possible dose of radiation should be administered to achieve diagnostic results. In some cases, this means forgoing an examination altogether or substituting an examination without ionizing radiation such as ultrasound or magnetic resonance imaging (MRI). In the acute trauma setting, nonionizing alternatives are not always possible. At a minimum, however, doses should be minimized and monitored.
Most facilities now have pediatric protocols in place for higher radiation examinations, particularly CT. Decreasing the milliamperes and performing helical rather than pure axial CT (as is commonly used with the adult head CT) are examples of ways to reduce dose in the acute setting. Customizing protocols in conjunction with subspecialties should also be considered, such as using a half or quarter dose CT (by decreasing milliamperes) for routine follow-up of patients where fine anatomic detail is not imperative. Examples include examinations for evaluating ventriculoperitoneal shunt placement, revision, or malfunction; preoperative fiducial scans; or postcraniofacial distraction cases. Alternative image reconstruction methods to filtered back-projection are being developed and evaluated; such methods have the potential to significantly reduce dose for all CT examinations. A more complete review is beyond the scope of this paper, but Zachariah et al discuss pediatric specific and general factors, such as centered patient positioning, shielding, filtering, and others.12
5.4 Typical Traumatic Findings
Many findings in children who have suffered head trauma mirror the common findings in adults. In a recent evaluation of initial CT findings in pediatric TBI, parenchymal lesions (including contusion, hematoma, and hemorrhagic shear) were found to be most the common injuries.13
Subdural hematomas tend to be crescentic and do not respect sutures, but they do respect the midline (▶ Fig. 5.1). Epidural hematomas are usually convex and respect sutures, with a tendency to grow over the course of hours (▶ Fig. 5.2). An underlying fracture is present in almost all cases. Subarachnoid hemorrhage is often scattered or diffuse and seen within the cerebral sulci (▶ Fig. 5.3 and ▶ Fig. 5.4). Hemorrhagic contusions are often seen acutely, and the underlying damage is often greater in extent than that seen on initial imaging (▶ Fig. 5.5). Shear injury is often difficult to appreciate on CT, and MRI will often better detect small foci of injury, T2* and inversion recovery sequences being particularly sensitive (▶ Fig. 5.6).14 With more severe trauma, multiple findings are often present (▶ Fig. 5.7).
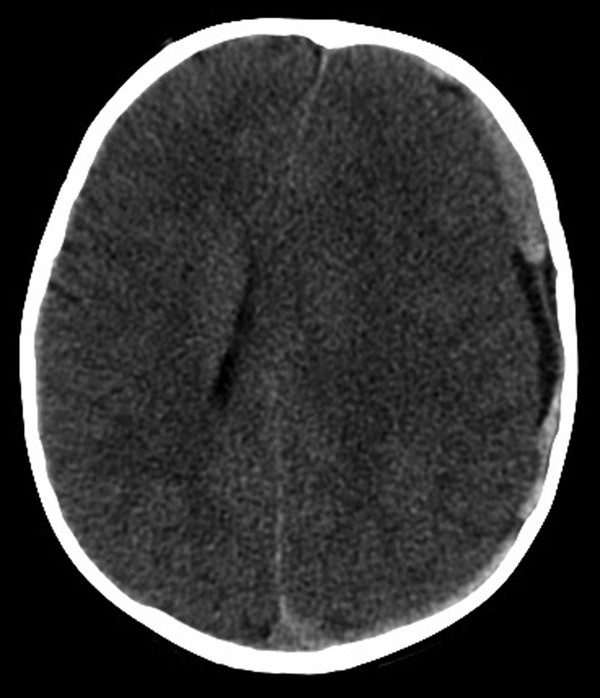
Fig. 5.1 Noncontrast axial computed tomography showing layering high-density material in a left holohemispheric distribution representing a subdural hemorrhage in a 21-month-old child after a fall. The midline shift is an important finding.
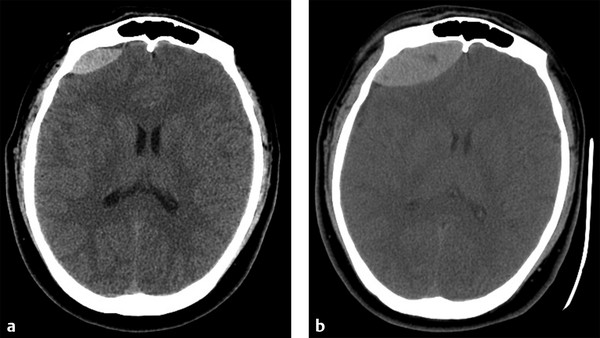
Fig. 5.2 (a) Axial image from noncontrast computed tomography (CT) showing lentiform high-density material in the right frontal area with some mass effect on the underlying gyri typical of an epidural hematoma in this adolescent after being hit in the head with a discus. (b) Three hours later, there is increasing size of the epidural hematoma with increased mass effect on the underlying parenchyma.
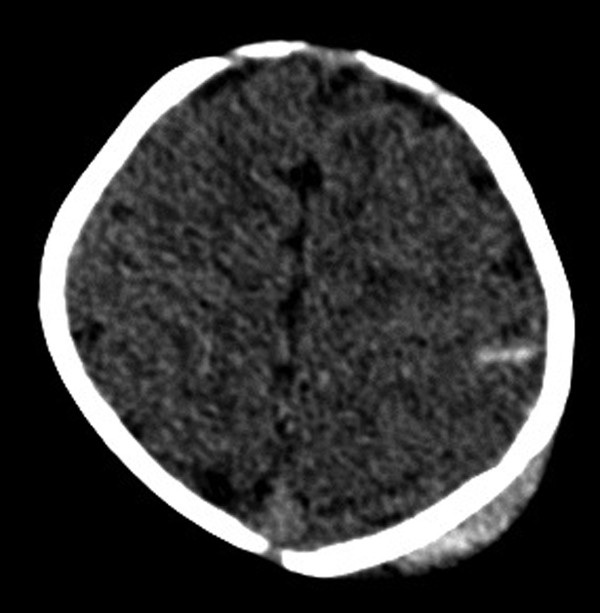
Fig. 5.3 Axial image from noncontrast computed tomography in a 4-week-old infant after being dropped 4 feet onto a hardwood floor. There is a single focus of high-density material in a left posterior frontal gyrus consistent with a small amount of subarachnoid blood.
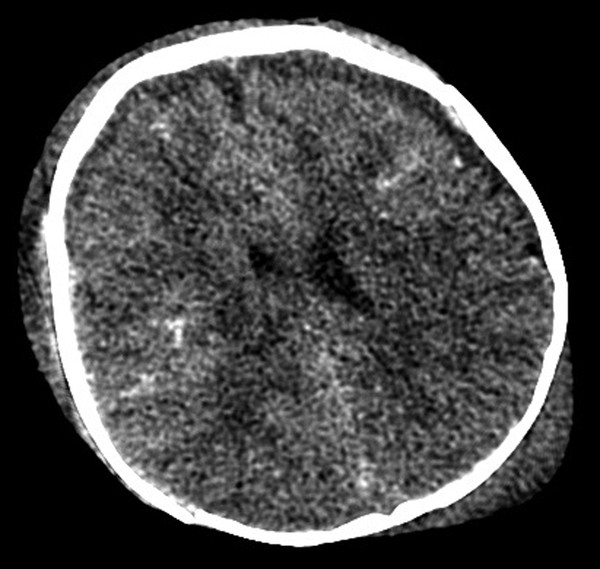
Fig. 5.4 Axial image from noncontrast computed tomography in a 5-month-old child dropped from 15 feet. Diffuse high-density material is seen within the sulci consistent with subarachnoid blood. Subdural fluid collections are also seen, along with scalp hematoma.
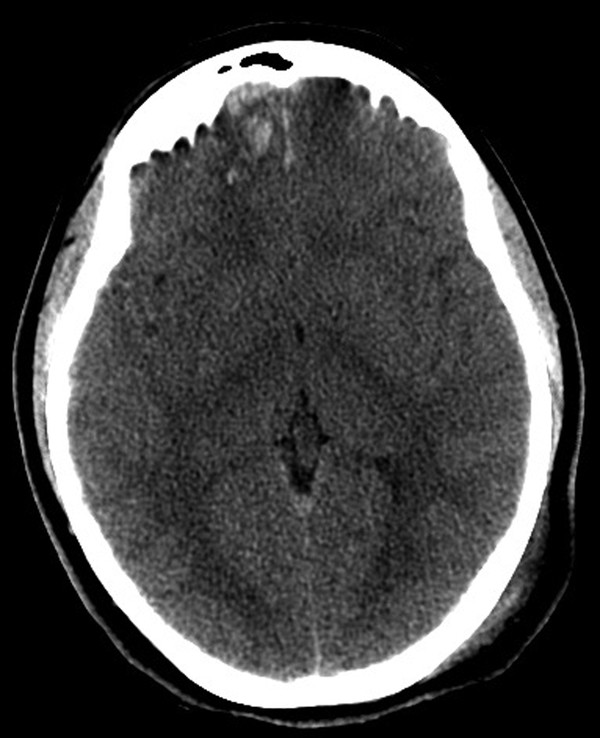
Fig. 5.5 Axial image from noncontrast computed tomography in an adolescent struck on the back of the head showing right frontal intraparenchymal blood consistent with hemorrhagic contusion from a coup-contrecoup mechanism.
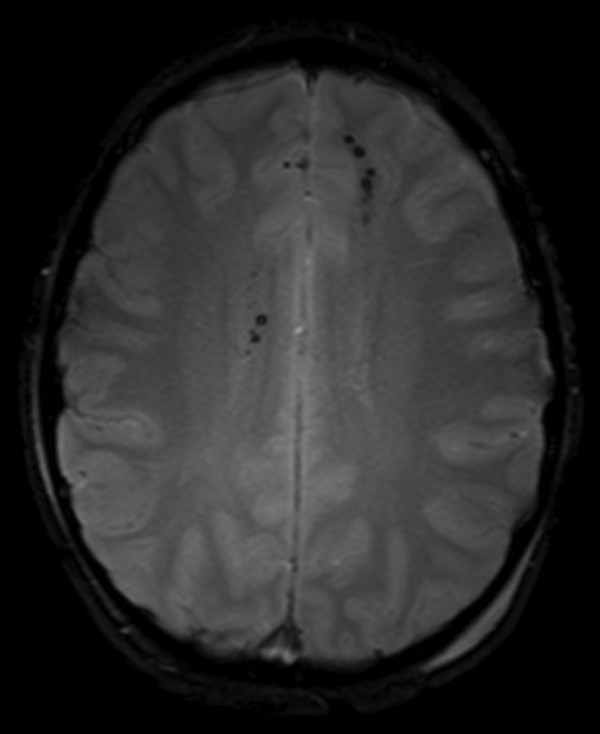
Fig. 5.6 Magnetic resonance imaging gradient recalled echo axial image in a 16-year-old trauma patient showing multiple punctuate foci of blooming signal dropout in the bilateral frontal and right corpus callosum. These are consistent with foci of hemorrhage and can be seen with diffuse axonal injury. Left posterior scalp swelling indicates the site of impact.
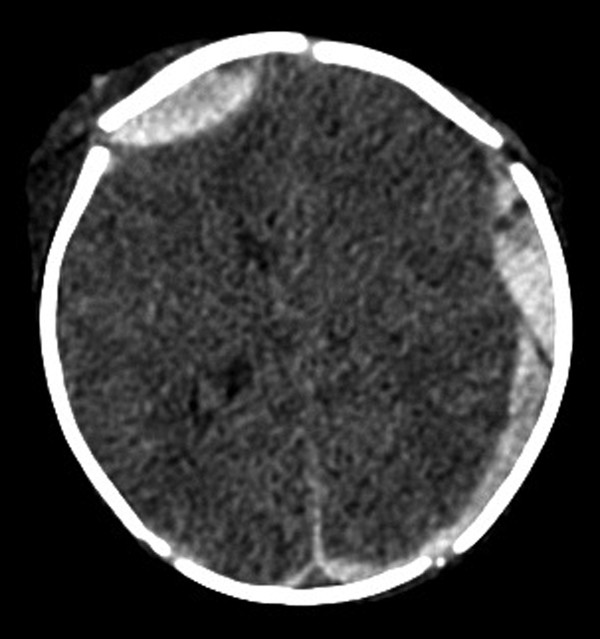
Fig. 5.7 Axial image from noncontrast computed tomography showing bilateral epidural high-density collections and posterior left subdural collection, as well as more subtle diffuse subarachnoid blood in a 1-day-old infant after a difficult forceps assisted delivery.
The presence of nonfused skull sutures in children adds some complexity to the evaluation of the injured child. CT is an excellent tool for fracture identification, and the ability to reconstruct images in a multitude of ways augments the examination significantly, particularly for fractures in axial plane. In addition to the standard axial bone and soft tissue reconstructions, volumetric or surface-rendered three-dimensional images can be useful (▶ Fig. 5.8). Multiplanar reformats and maxiumum intensity projection reconstructions have been shown to add accuracy.15
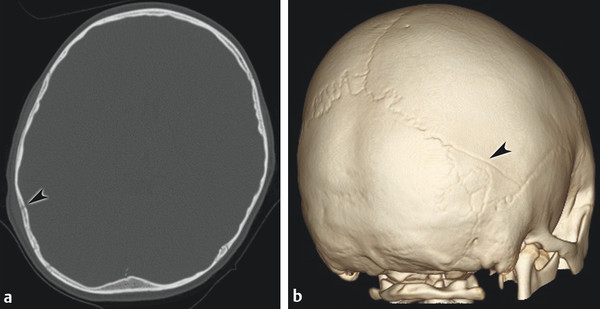
Fig. 5.8 (a) Axial bone reconstruction from noncontrast computed tomography in a 5-year-old boy who fell backward, hitting his head on concrete. There is a very subtle nondisplaced fracture of the posterior parietal bone (arrowhead) with overlying scalp swelling that is well seen on three-dimensional surface-rendering images (b) as a linear fracture extending obliquely from the midright lambdoidal suture to the squamosal suture (arrowhead). The fracture does not have the characteristic zigzag of normal suture and was not present on the contralateral side.
5.5 Pediatric Specific Traumatic Findings
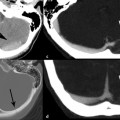
Although children are susceptible to the common types of head trauma seen in adults, some entities are seen exclusively in children. Incomplete or bowing-type fractures are called “ping-pong” fractures, as they have been likened to a dented table tennis ball (▶ Fig. 5.9).
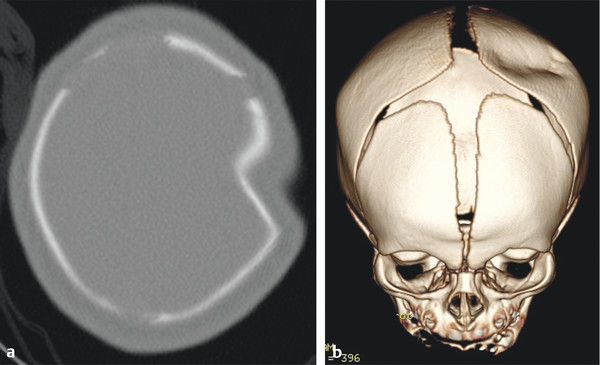
Fig. 5.9 (a) Axial noncontrast head computed tomographic image showing a prominent indentation but no cortical disruption of the left parietal bone in a 6-day-old infant. No history of trauma could be elicited, and the child was otherwise healthy. (b) Three-dimensional surface-rendered image shows the depression to advantage.
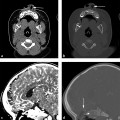
Growing skull fractures (▶ Fig. 5.10) are rare complications that develop after fracture or transdural surgery in the younger patient population, usually in those younger than 3 years.16 Approximately 1% of skull fracture cases will develop this complication.17 Also known as leptomeningeal cysts, they are thought to be due to transmission of cerebrospinal fluid (CSF) pulsations through a compromised dura.18 These can be purely cystic, containing only CSF, but often will contain herniated cerebral contents (pseudoencephalomeningocele).19 Underlying porencephaly or encephalomalacia is common. Depending on the extent of calvarial coverage, these patients can have a growing hard lump or a soft lump, which may pulsate. These lumps will enlarge over time, and surgical treatment is required to repair the calvarial defect and underlying dural defect.
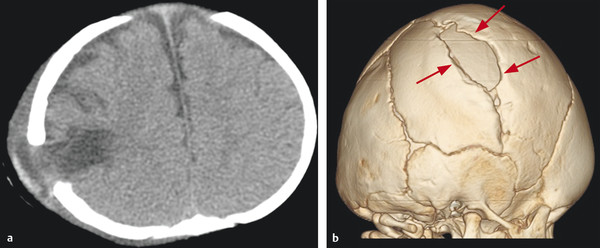
Fig. 5.10 This 5-month-old child was the victim of abusive head trauma at 2 months of age that resulted in a parietal skull fracture and parenchymal contusion (not shown). Follow-up axial noncontrast CT (a) shows an area of low-density encephalomalacia protruding through a prominent skull defect at the site of prior fracture. Surface-rendered three-dimensional image (b) shows the bone defect situated within the fracture line (arrows) consistent with a leptomeningeal cyst and pseudomyelomeningocele.
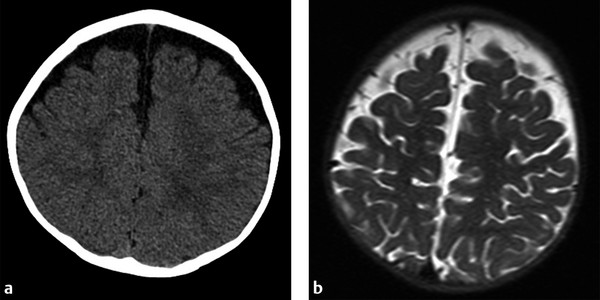
A common confounder in the evaluation of young children with head trauma is the relatively common finding of enlarged extra axial CSF spaces, often seen during the evaluation of macrocephaly. A variety of terms have been applied to this finding or similar findings, the most prevalent being benign external hydrocephalus and subdural hygroma, despite the subarachnoid location.20 The hallmark features are children less than 3 years with enlargement of subarachnoid CSF spaces seen usually in the frontal and intrahemispheric areas. Bridging veins can be seen on MRI or high frequency cranial ultrasound if the fontanelle is open (▶ Fig. 5.11). The fluid should follow the density or signal of CSF on all imaging modalities. This condition can be idiopathic, acquired, or familial. Benign familial macrocephaly is an autosomal dominant condition in families with incomplete penetrance. There is debate in the literature regarding whether these children are prone to subdural hemorrhage with minor or even no known trauma.20,21