7
Small Bowel
Small Bowel Obstruction
Overview
 Most commonly due to adhesions (70%) or incarceration of bowel within a hernia
Most commonly due to adhesions (70%) or incarceration of bowel within a hernia
 Other etiologies include small bowel tumor, volvulus, intussusception, and strictures
Other etiologies include small bowel tumor, volvulus, intussusception, and strictures
 Obstruction may be partial or complete
Obstruction may be partial or complete
Signs and Symptoms
 Colicky periumbilical pain that may be relieved with bilious emesis
Colicky periumbilical pain that may be relieved with bilious emesis
 Abdominal distention, tenderness, and occasional high-pitched bowel sounds
Abdominal distention, tenderness, and occasional high-pitched bowel sounds
 Severe tenderness at the site of incarcerated hernia with possible overlying skin changes
Severe tenderness at the site of incarcerated hernia with possible overlying skin changes
 Patients with complete bowel obstruction will have absence of flatus or bowel movement, patients with partial bowel obstruction will present with abdominal distention with decreased passage of flatus
Patients with complete bowel obstruction will have absence of flatus or bowel movement, patients with partial bowel obstruction will present with abdominal distention with decreased passage of flatus
Diagnosis
 Abdominal x-rays will show multiple air–fluid levels with distended loops of small bowel
Abdominal x-rays will show multiple air–fluid levels with distended loops of small bowel
 CT scan with IV contrast may be obtained to assess for a transition point
CT scan with IV contrast may be obtained to assess for a transition point
Treatment/Management
 NPO for bowel rest, IV fluids, NG decompression; correct any underlying electrolyte abnormalities
NPO for bowel rest, IV fluids, NG decompression; correct any underlying electrolyte abnormalities
 Attempt to perform bedside reduction of any incarcerated hernia
Attempt to perform bedside reduction of any incarcerated hernia
 Patients with diffuse peritonitis or complete bowel obstruction should warrant surgical exploration
Patients with diffuse peritonitis or complete bowel obstruction should warrant surgical exploration
 Patients with partial bowel obstruction who do not improve with conservative management will require exploration and adhesiolysis with possible bowel resection
Patients with partial bowel obstruction who do not improve with conservative management will require exploration and adhesiolysis with possible bowel resection
 Patients without signs of incarcerated hernia and who have no previous abdominal surgeries should also be surgically explored
Patients without signs of incarcerated hernia and who have no previous abdominal surgeries should also be surgically explored
RADIOLOGY
 Plain film findings (Fig. 7.1)
Plain film findings (Fig. 7.1)
• Dilated small bowel loops with air fluid levels
 CT findings (Fig. 7.1)
CT findings (Fig. 7.1)
• Fluid-filled, dilated small bowel loops
• Closed-loop obstruction manifests as a C-shaped configuration of dilated bowel loops with mesenteric vessels converging toward the point of torsion
• Strangulation is characterized by bowel wall thickening, little or no contrast enhancement of the bowel wall, engorgement of mesenteric vasculature, and mesenteric edema
• Small bowel loops are dilated proximal to the obstruction, and decompressed distal to the obstruction
FIGURE 7.1 A–H

FIGURE 7.1 A
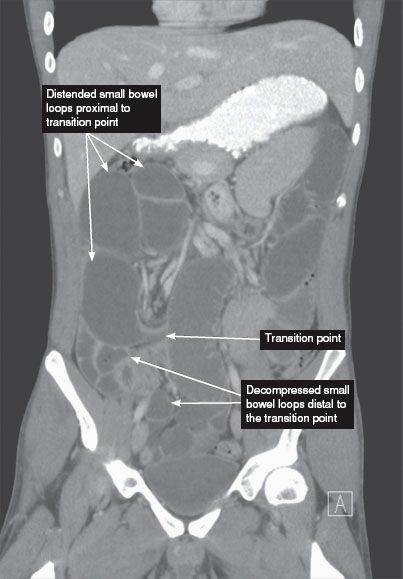
FIGURE 7.1 B
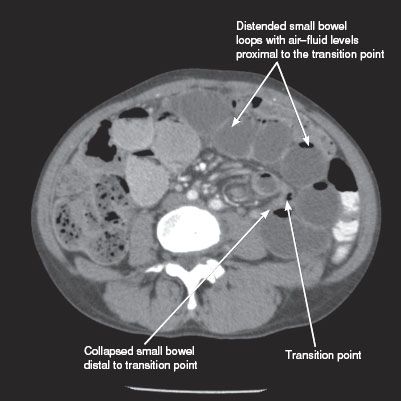
FIGURE 7.1 C
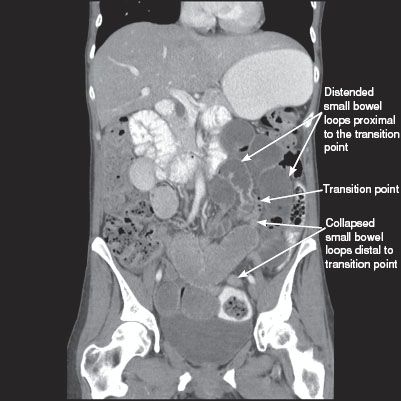
FIGURE 7.1 D
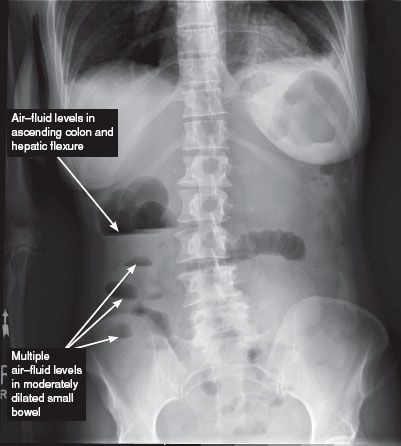
FIGURE 7.1 E
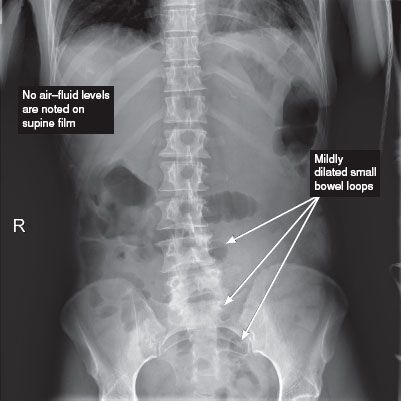
FIGURE 7.1 F
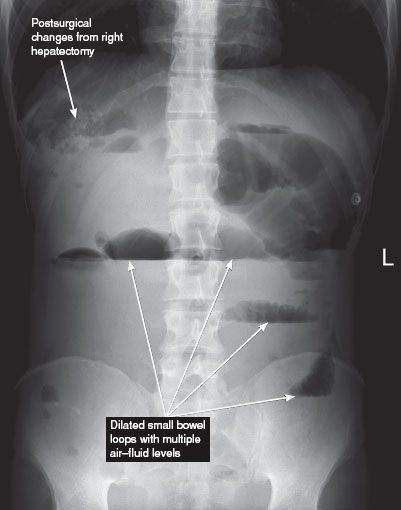
FIGURE 7.1 G

FIGURE 7.1 H
Ileus
Overview
 Lack of peristalsis or bowel function without a structural obstruction
Lack of peristalsis or bowel function without a structural obstruction
 Most commonly secondary to abdominal surgery
Most commonly secondary to abdominal surgery
 Other causes are electrolyte abnormalities, intra-abdominal abscess, systemic infection, hypothyroidism, or other medications such as anticholinergics
Other causes are electrolyte abnormalities, intra-abdominal abscess, systemic infection, hypothyroidism, or other medications such as anticholinergics
Signs and Symptoms
 Abdominal distension without flatus or bowel movements
Abdominal distension without flatus or bowel movements
 Bilious or feculent emesis
Bilious or feculent emesis
 Generalized abdominal distension associated with discomfort without diffuse peritonitis
Generalized abdominal distension associated with discomfort without diffuse peritonitis
Diagnosis
 Same as small bowel obstruction
Same as small bowel obstruction
Treatment/Management
 Same as small bowel obstruction
Same as small bowel obstruction
 May consider initiation of total parenteral nutrition (TPN) for patients who have prolonged ileus with underlying malnutrition
May consider initiation of total parenteral nutrition (TPN) for patients who have prolonged ileus with underlying malnutrition
RADIOLOGY
 Plain film findings (Fig. 7.2)
Plain film findings (Fig. 7.2)
• Distended small bowel loops with air fluid levels
• May be indistinguishable from SBO
• Distal air in the rectum may help differentiate ileus from SBO
FIGURE 7.2 A,B

FIGURE 7.2 A

FIGURE 7.2 B
Small Bowel Enterocutaneous Fistula
Overview
 A fistula is defined as an abnormal connection between two epithelized organs
A fistula is defined as an abnormal connection between two epithelized organs
 Small bowel enterocutaneous fistula is usually caused by unrecognized iatrogenic injury to the bowel, anastomotic leak, inflammatory bowel disease, or malignancy
Small bowel enterocutaneous fistula is usually caused by unrecognized iatrogenic injury to the bowel, anastomotic leak, inflammatory bowel disease, or malignancy
Signs and Symptoms
 Fever, leukocytosis, ileus, abdominal tenderness followed by drainage of enteric contents via the wound or skin
Fever, leukocytosis, ileus, abdominal tenderness followed by drainage of enteric contents via the wound or skin
 Factors that prevent fistula closure—(FRIEND)
Factors that prevent fistula closure—(FRIEND)
• Foreign body
• Radiation
• Inflammation/infection
• Epithelialization of the tract
• Neoplasm
• Distal obstruction
Diagnosis
 CT scan with enteric contrast will help identify any undrained abscess. It might help identify the origin of the fistula
CT scan with enteric contrast will help identify any undrained abscess. It might help identify the origin of the fistula
 Fistulogram or sinogram consists of contrast injection into the cutaneous end of the fistula to evaluate the tract and origin of the fistula
Fistulogram or sinogram consists of contrast injection into the cutaneous end of the fistula to evaluate the tract and origin of the fistula
Treatment/Management
 Usually treatment consists of making patient NPO, parenteral nutrition, possible octreotide to decrease the output from the fistula for easier wound management
Usually treatment consists of making patient NPO, parenteral nutrition, possible octreotide to decrease the output from the fistula for easier wound management
 Definitive treatment is surgery if spontaneous closure does not occur within 4 to 5 weeks’ time
Definitive treatment is surgery if spontaneous closure does not occur within 4 to 5 weeks’ time
RADIOLOGY
 Plain film findings
Plain film findings
• Contrast injection through the fistula can diagnose the tract between the skin and the small bowel lumen
 CT findings (Fig. 7.3)
CT findings (Fig. 7.3)
• CT can be performed in addition to a fistulogram to distinguish fluid collections from bowel loops, and also to guide percutaneous drainage of any abscesses
• A fistula between the small bowel and skin can sometimes be directly seen on CT
• Fat stranding and abscess formation may be seen around the fistula tract
FIGURE 7.3 A–C
A. Stomach
B. Descending colon
C. Portal vein
D. Liver
E. Mesenteric vessels
F. Psoas muscle
G. IVC
H. Common iliac artery
I. Small bowel loops
J. Vertebra
K. Kidney

FIGURE 7.3 A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree