Fig. 11.1
Graf standard plane. (a) Schematic drawing of relevant structures, lines and angles for hip US according to Graf. (b) Typical corresponding US image (standardised projection – upright position, always projected as right sided)
Transducer placed over major trochanter in cranio-caudal coronal direction.
Then carefully move to parallel sections and rotate on acetabular axis without tilting for imaging the standard plane to be used for diagnosis and measurements.
Structures to identify on adequate view of acetabular mid portion: lower limb of bony ilium in depth of acetabular fossa representing physis, middle of acetabular roof with straight iliac bone line and acetabular labrum (three obligatory landmarks); additionally brief overview of entire joint space should be performed.
Dynamic Assessment
Advisable (normal-appearing hips can be mobile due to laxity of joint capsule after birth – elastic whipping in normal joint):
Particularly if suspicious findings on standard section – mandatory dynamic assessment.
Push and pull softly on leg for assessment of stability (femoral head stays well positioned within joint).
Instability – displacement of femoral head out of (dysplastic) joint fossa (e.g. OEGUM/DEGUM recommendation – see: www.OEGUM.at/content/view/506/210 download “Standard dokumentation der Sonografie der Neugeborenen- und Säuglingshüfte”):
In displaced or luxated hips: check for repositionability by respective manoeuvres under US surveillance.
Documentation
Two individually acquired images per hip joint in standard plane:
One of them must contain measurements (see below, Fig. 11.2).
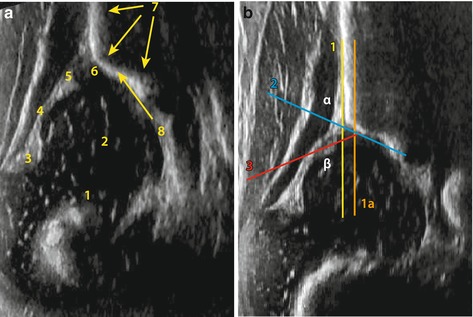
Fig. 11.2
Relevant structures, one image without (a) and one with (b) angle measurements. Patient identification and side mandatory, (gestational) age helpful. (a) 1 transition zone of osseous to cartilaginous part, 2 femoral head, 3 fold, 4 capsule, 5 cartilaginous labrum, 6 cartilaginous roof, 7 osseous contour of ilium bone, 8 bony rim. (b) 1 base line, 1a auxiliary line, 2 bony roof line, 3 cartilaginous coverage line, α (between line 1 and 2) 65°, β (between 1 and 3) 59°
In instable hips, a series of images or video clip showing respective changes during stress manoeuvres needs to be documented.
11.1.2.2 Modified Graf Classification (Rosendahl)
Objective: classify hip morphology and stability separately.
Technique: hip morphology (α-angle) assessed in standard coronal view (Graf) with centred femoral head:
If hip decentering, eccentric or dislocated hips (Graf 2c, D, 3, 4): femoral head relocated by mild traction, then thereafter reassess hip morphology.
Irreducible hip – morphology assessed with dislocated femoral head.
NOTE: Always additional Barlow manoeuvre to assess for coexisting instability even in morphologically normal hips.
Stability classification as above.
11.1.2.3 Hip US According to Harcke
Objective: classify hip stability.
Technique: infant lying supine, transducer positioned over lateral aspect of hip.
Coronal images with hip neutral and in flexion, plus posterior lip view.
Transverse images with hip flexed with passive abduction and adduction, followed by transverse images with stress to evaluate hip stability.
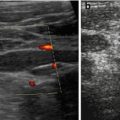
Images must document findings and need to be labeled appropriately (Fig. 11.3a).
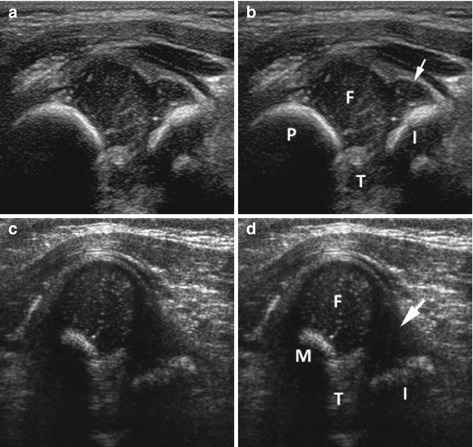
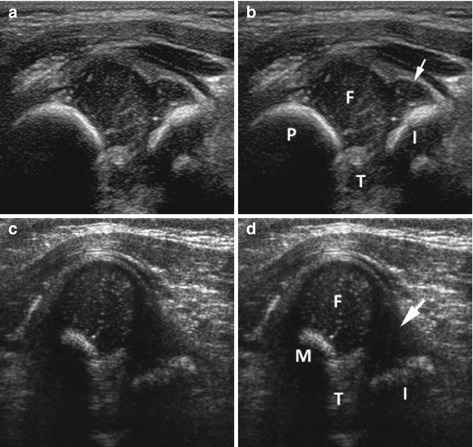
Fig. 11.3
Harcke hip US (image and image with labels). (a, b) Normal hip: normal position of femoral head on this transverse view. Notice cup-like appearance formed by metaphysis and ischium. No change with stress manoeuvre. (c, d) Abnormal hip: transverse view of hip with stress showing subluxation of femoral head from its normal position and disruption of cup-like configuration. This hip was reducible. Abbreviations: F femoral head, M femoral metaphysic, I ischium, T triradiate cartilage, Arrow cartilaginous labrum
11.1.2.4 Femoral Head Coverage According to Morin (and Modified Morin – Terjesen)
Assesses degree of lateralisation of femoral head based on Harcke’s coronal flexion view.
Two lines drawn paralleling Graf’s baseline:
One tangent to lateral part of femoral head.
One tangent to medial junction of head and acetabular fossa.
Measure distance between medial and iliac lines and between medial and lateral lines.
Calculate ratio multiplied by 100 = % of femoral head covered by bony acetabulum.
Modified Morin (Terjesen): instead of iliac line, use line through lateral bony rim of acetabulum parallel to long axis of transducer measuring “bony rim percentage”, later named “femoral head coverage”.
11.1.2.5 Assessment of Joint Effusion, Capsular Thickening, Perthes, Arthritis and Others
US performed in supine position leaving leg in spontaneous position:
Support of knees helpful to relax – less painful.
Transducer positioned anteriorly along femoral neck; usually slightly lateral to course of femoral vessels sagittal and parasagittal sections acquired – cross sections rarely helpful but can be acquired.
11.1.3 Normal Anatomy
Typically femoral head is roundish, in neonates cartilaginous – later central echogenic ossification centre appears, varying size depending on age.
Additionally: ossified femoral neck, border zone between cartilaginous and ossified parts, joint capsule – tracking from femoral neck to acetabulum.
11.1.3.1 US Criteria in Graf
Good definition of bony rim.
Undisplaced cartilaginous roof triangle.
Normal position of well-covered femoral head in acetabular fossa.
Iliac bone seen as straight line with clear border to cartilaginous acetabular labrum – good osseous definition.
Bony angle (α) >60°, cartilaginous angle (β) <55° (defined below):
Values can be present at birth but must be reached by 3 months.
NOTE: Correct section through joint with sufficient depiction of all three landmarks mandatory for judging hip maturity and for performing angle measurements – if section taken angulated or too ventral or dorsal (usually recognised by bent shape of iliac line or incorrect/missing identification of bony fossa definition), measurements always wrong and diagnostically useless.
11.1.3.2 Rosendahl Modification
No essential difference from Graf technique with addition of compulsory stress test (similar to Graf’s “dynamic examination”).
Angle Measurements – Measured Between three Lines.
1.
First line (baseline) from osseous rim of iliac bone in straight line paralleling osseous iliac contour (Fig. 11.4a).
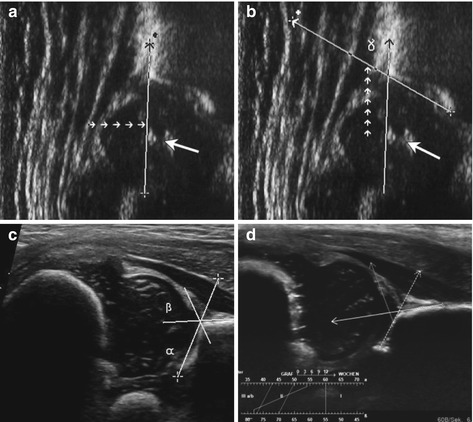
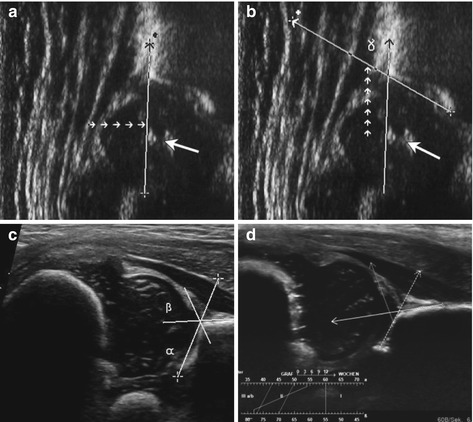
Fig. 11.4
Hip angle measurements and lines (a–d). (a) How the baseline is defined. (b) Definition of acetabular roof line. (c) Cartilaginous roof line added, with normal angle α and β – not an upright standardised view, increasingly used for practicability and device restrictions; left hand image is cranial. (d) Hip US with integrated sonometer software: the software automatically indicates angles (α 54°, β 78°) and thus hip type (full line) after manual definition of respective lines (immature type II hip, suboptimal coverage, dynamic assessment shows elastic whipping) not an upright standardised view, increasingly used for practicability and device restrictions; left hand side on image is cranial
2.
Second line (“bony roof line – acetabular roof line”) from inferior rim of iliac bone as pivot point tangential to bony roof (Fig. 11.4b).
3.
Third line (“cartilage roof line”) from centre of labrum to bony rim, defined as point where convexity changes into concavity of acetabulum (Fig. 11.4c).
Bony angle α: defined between first and second line, shows osseous coverage:
If normal = good (e.g. more than 50 %) (Fig. 11.4d).
Cartilaginous angle β: measured between first and third line, defines site and configuration of cartilaginous roof:
If roof flat = high β angle – risk of instability (Fig. 11.4e).
NOTE: Angle measurements only valid in correctly performed exams.
Small α angle always indicates dysplasia and poor coverage and at least immaturity.
11.1.3.3 Normal Findings During Harcke Investigation
Cartilaginous femoral head positioned in acetabulum as defined by triradiate cartilage centrally and posterior ischium, with femoral metaphysis seen anteriorly.
No displacement seen with stress – image remains the same, with head centred in fossa (see Fig. 11.3a).
11.1.3.4 Anatomic Landmarks and Normal Limits for Measuring Femoral Coverage
Lateral part of femoral head, medial junction of head, acetabular fossa.
Lower normal limits: boys – 47 %, girls – 44 %.
11.1.3.5 Hip US in Older Children
Applications and queries: Perthes disease, infection, proximal femoral deficiency, slipped capital femoral epiphysis, trauma, joint effusion.
Normal US findings:
Typically longitudinal section, frontal sagittal view.
Ossified head, neck connected by non-ossified physis – anechoic line.
Minimal fluid within joint space.
Capsule small, sometimes difficult to delineate.
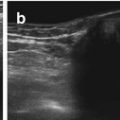
Visible contours of acetabulum and femoral head and neck – continuous, without disruption, smooth and clearly defined surface (Fig. 11.5a).
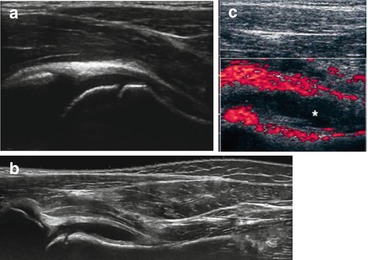
Fig. 11.5
Normal hip (a) in older children – as opposed to hip effusion (b) and septic hip (c). (a) Normal longitudinal hip US in an older child; normal joint capsule (synovium) appears prominent, as both layers are collapsed. (b) Simple hip effusion (transient synovitis, extended field of view): echo-free fluid in widened joint space, thickened capsule. (c) Power Doppler in septic arthritis: note impressive hypervascularity of thickened synovium, complex fluid in widened joint space
11.1.4 Pathologic Findings
11.1.4.1 Developmental Dysplasia of the Hip (DDH)
Criteria vary depending on method applied (Graf, Harcke, adapted Graf, femoral head coverage, femoral distance).
Remark/Comment: early detection and treatment = only way for non-invasive management – important to early recognise DDH to avoid long-term sequelae, immense healthcare costs, individual morbidity, e.g. by repeated surgery. The debate of role of screening ongoing in Anglo-American literature; in most of middle Europe some screening established.
NOTE: Hip US for dysplasia – “final” investigation (if you miss an endangered hip, the patient will only come back after years or decades when symptomatic) – strict and consistent adherence to all quality criteria is essential. As with mammography, clinical investigation and anamnestic data are mandatory part of every examination.
DDH According to Graf
Strict classification that differentiates between immaturity, dysplasia, instability and luxation (Table 11.1).
Immaturity – Type II
Consider age: depending on subtype, defined by sufficient to poor ossification, with some rounding of bony rim:
Cartilaginous acetabulum usually still covering hip but much wider than osseous acetabulum:
Due to ossification deficit – covering > half of femoral head.
Potentially delayed ossification.
Subtypes:
II A +: physiological immaturity.
II A–: maturation deficit during first 3 months.
II B: after third month of life, α ≤ 60°.
II C: developmentally dysplastic hip – definitely endangered, needs treatment:
Dynamic stress manoeuvres are mandatory.
(II) D – usually unstable hip with beginning decentering:
Dynamic stress manoeuvres mandatory.
Very rounded bony rim.
Initially displaced cartilaginous acetabulum.
α = 43°–49°, β > 77°.
Only treatment option – fixation.
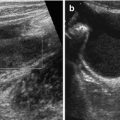
Decentered Hip – Type III (Fig. 11.6)
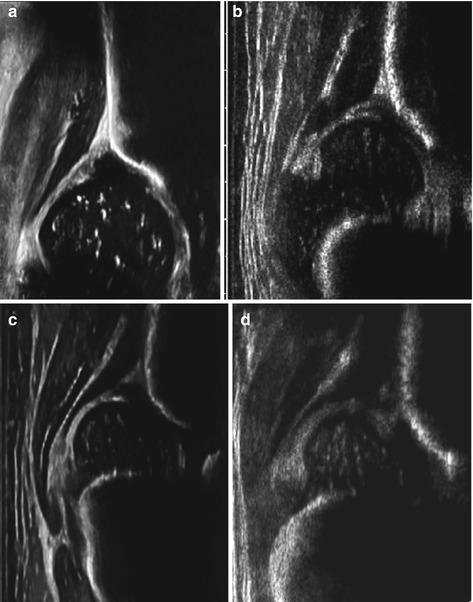
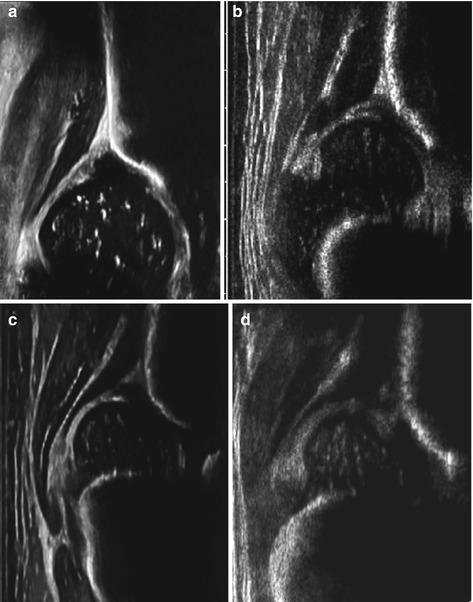
Fig. 11.6
Pathological hips (Graf classification). (a) Immature hip, slightly rounded roof (>3 months of age – type IIa). (b) Endangered hip: severely rounded bony roof, displaced cartilaginous roof, dynamic assessment mandatory (type D). (c) Dysplastic – decentered hip with flat bony roof – type III. (d) Luxated hip – by definition cartilaginous labrum compressed between femoral head and iliac bone (type IV)
US Criteria:
Femoral head has pushed cartilaginous acetabular roof cranially:
Insufficient osseous containment with flat bony rim.
Insufficient bony as well as cartilaginous coverage.
Decentering of femoral head and cartilaginous acetabulum:
Type III A – hyaline cartilage hypoechoic.
Type III B – cartilaginous acetabulum small, compressed, distorted – structural anomalies – some echoes and inhomogeneous. Only in untreated and chronically dislocated hips – sign of severe damage (remark: very uncommon in Middle Europe).
Therapy: needs repositioning and fixation.
US criteria:
Femoral head displaced from joint space:
Luxated in cranial, lateral or dorsal position.
Cartilaginous acetabulum herniated and displaced caudally:
Pressed in between femoral head and iliac bone – increased inhomogeneous echoes.
Sometimes difficult to find bony rim – reliable measurements often impossible/not required.
Dynamic assessment helps to evaluate for repositionability.
Results in Rosendahl Modification
According to morphology (using Graf angle discrimination):
Immature, mildly dysplastic, severely dysplastic.
Using stability: stable, dislocatable, dislocated.
DDH According to Harcke
Classification: normal, lax with stress, subluxed or dislocated (see Fig. 11.3b).
NOTE: Method more subjective; also includes description of hip stability. Neither accuracy nor population-based rates of pathological hips based on this technique have been published.
Hip Assessment Based on Femoral Head Coverage
All outside accepted limits = DDH – less potential for grading, used as initial screening tools to assess for normal or abnormal hips.
In abnormal hips, either Harcke or Graf method can be applied additionally for treatment decisions.
11.2 Other Conditions of Hip Joint
11.2.1 Arthritis and Inflammation of Hip Joint
As in all joints, examination of contralateral (not affected side) helpful for comparison (start there).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree