Location: Lower limb (thigh), retroperitoneum, pelvic region, upper limb, trunk, head, and neck. Deeply located.
Clinical: Slow enlarging painless mass, increased skin temperature, telangiectasia, unilateral varicose veins, pulsation, audible bruit, urinary retention, hydronephrosis, constipation, vomiting, hypoglycemia.
Imaging: On angiography: rich vascularity, encircled by tortuous vessels, arborizing from one pedicle, rapid arteriovenous flow. On CT: heterogeneous mass sharply enhanced after contrast. On MRI: homogeneous intermediate intensity with high-signal hemorrhagic zones on T1, inhomogeneous bright lesion on T2, prominent serpentine vessels with signal intensity depending on the flow within them, strong enhancement with ill-defined necrotic areas that do not become enhanced.
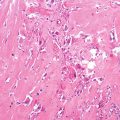
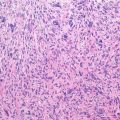
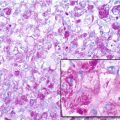
Histopathology: Soft, from pale to dull red or brownish red, heavily bleeding, thin pseudocapsule, cystic hemorrhagic necrotic areas. Thick, diffused network of capillaries, totally collapsed or wide-open sinusoids, surrounded by compact proliferation of cells with oval nuclei, distinct nuclear membrane, granular chromatin, small nucleolus, ill-defined cytoplasm, thick reticular fibers all around. Cells are organized in a so-called patternless pattern. Mature flattened endothelium. Typical “staghorn-like” shape of vessels. There is no strict correlation between morphology and behavior. However, histological aspects that could predict an aggressive and malignant behavior are high cellularity, cellular atypia, extensive necrosis, and >4/10 HPF mitotic figures. On immunohistochemistry, SFT/HPC is positive for vimentin, CD34, CD99, and Bcl2.
Course and Staging: Slow growth, benign more frequent than malignant. About 10 % behave aggressively with local and distant recurrence. Benign, stage 3; malignant, stage IIB. If malignant, recurrence and metastases are frequent.
Treatment: As the biological behavior of SFT is unpredictable, wide excision is the treatment of choice. The role of radio- and chemotherapy is unclear.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree