Case presentation
A 16-year-old female presents with a history of severe headaches, nausea, and vomiting for the past 3 weeks. She was seen at an urgent care facility where she was diagnosed with sinusitis and was given prescriptions for odansetron, prednisone, and amoxicillin. After several days of these medications, she did not experience any relief, so she was seen by her primary care provider. She was given an injection of ceftriaxone, her oral antibiotics were changed to cefdinir, and the steroid dose was lowered. The child’s headaches, nausea, and vomiting were persistent, so she was brought to the emergency department for evaluation.
The headaches have become daily and occur throughout the day. She does have nighttime headache, which started 1 week ago. She states that the headaches cause nausea, which leads to emesis. There has been no fever, neck pain, back pain, vision changes, incontinence, or weakness; she has noted intermittent numbness to the fingertips of both her hands. There has been no report of trauma. She has been taking nonsteroidal antiinflammatory medications, which have become less effective over the past week.
Her examination is unremarkable, other than complaint of mild headache, which is primarily left frontal in location. She is afebrile; her heart rate is 84 beats per minute, respiratory rate is 18 breaths per minute, and blood pressure is 120/80 mm Hg. She is awake, alert, and age appropriate. Her pupils are equal, round, and reactive to light. There is no evidence of papilledema and her extraocular movements are intact. She has no visual field cuts and cranial nerves II–XII are grossly intact. Deep tendon reflexes are 2+ and symmetric. She moves her extremities symmetrically with no apparent weakness, spasticity, or hypotonia. Her gait is steady and there are no cerebellar findings. Her sensation appears intact.
Imaging considerations
Imaging is often employed in patients with general neurologic complaints, such as severe headache, focal neurologic findings including ataxia, or if there are symptoms that raise suspicion for an intracranial process, such as emesis or vision changes, or concerning historical findings (such as wakening in the middle of the night with headache, first morning emesis, or persistent/worsening headache). The choice of imaging modality may be influenced by the resources available at a particular facility.
Computed tomography (CT)
This imaging modality is an excellent first-line choice when there is concern for an intracranial hemorrhage, mass, or lesion. CT is widely available, sedation is generally not required, and intravenous contrast is not generally indicated.
Magnetic resonance imaging (MRI)
This imaging modality can provide details of the intracranial structures and anatomy. Often, this test is obtained to further delineate findings initially identified on CT. Cost, availability, and the potential need for sedation are barriers to MRI use as a first-line imaging modality.
Imaging findings
The patient underwent noncontrast CT imaging of the brain. A selected image from that study is included. These images demonstrate an approximately 8 × 7 × 6-cm arachnoid cyst in the region of the left Sylvian fissure, extending from the mid-left frontal extra-axial space to the floor of the left middle cranial fossa. There is mild mass effect and bilateral extra-axial fluid collections, most consistent with hygromas ( Fig. 36.1 ).

Case conclusion
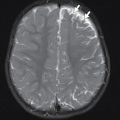
Pediatric Neurosurgery was consulted. The patient was admitted to the hospital for observation and remained stable. After discussion with the family, the decision was made to perform an arachnoid fenestration. The next day, she had an MRI study, prior to surgery to assess for any other structural anomalies. This study again demonstrated the left frontotemporal arachnoid cyst causing distortion of the left frontal and temporal lobe contours and mild effacement of the left lateral ventricle from mass effect. There are 6-mm-thick bilateral frontoparietal subdural hygromas. There is mild flattening of the lateral hemispheric parenchymal contour from mass effect ( Figs. 36.2 and 36.3 ). The child was electively taken to the operating room for arachnoid cyst fenestration, which was performed successfully. She recovered uneventfully.