Case presentation
A 7-month-old baby presents with left infraorbital swelling and erythema for the past 2 days, which has progressed rapidly. There has been a fever of 101.5 degrees Fahrenheit for the past 24 hours. He has not had cough, congestion, vomiting, or diarrhea. Four days ago, the child was playing with his older sibling, who, during the course of play, threw a small toy car at the child, striking him in the left side of the face (under the eye) and causing a small abrasion. The wound did not appear large and the mother has been keeping the area clean with soap and water. He has been eating and drinking well and is otherwise at his baseline.
Physical examination reveals a child in no distress. His temperature is 100.1 degrees Fahrenheit, his heart rate is 137 beats per minute, and his respiratory rate is 30 breaths per minute. He has obvious erythema and swelling to the left periorbital area, particularly the infraorbital area, which is warm and is painful when palpated. There is no fluctuance, but there is induration. The child is unable to open the eye (which you find very difficult to open due to the swelling) and consequently the pupil, conjunctiva, and sclera are not visible. There is no proptosis. There is moderate yellow eye discharge and eyelash mattering.
Imaging considerations
Plain radiography
Plain radiography is not a first-line imaging modality in patients with suspected periorbital infection and associated complications. While indications suggestive of sinus disease can be visualized, signs of sinus mucosal thickening may be nonspecific in pediatric patients, and neither cellulitis nor an abscess will be visualized with this imaging test.
Computed tomography (CT)
This modality is the imaging modality of choice to evaluate periorbital and orbital infections. Examination of the child with periorbital cellulitis can be difficult, since pediatric patients are often anxious and uncooperative, and there may be significant swelling and/or pain. CT has been increasingly used to determine the extent of infection and evaluate patients for possible orbital involvement. One study reported the use of CT in almost 94% of patients. In patients with a clinical examination that is consistent with an uncomplicated periorbital infection, it is reasonable to withhold CT imaging and initiate antibiotic therapy with close observation. If there is no improvement in 48 hours, worsening clinical examination, or signs of complications (neurologic symptoms or increasing pain), then obtaining imaging is reasonable. CT is appropriate when there is concern for orbital infection, abscess, or intracranial complication and when clinical examination is difficult. , , Periorbital cellulitis will appear as diffuse soft-tissue thickening and areas of enhancement anterior to the orbital septum on CT. Intravenous contrast should be utilized. As contemporary scanners are rapid, sedation is usually not required. The use of pediatric protocols to lower ionizing radiation exposure time is recommended per American College of Radiology guidelines.
Magnetic resonance imaging (MRI)
This modality is excellent at detecting infectious and inflammatory processes but is not a first-line imaging test. A study with and without contrast can be obtained to complement CT findings if further detail of an identified pathologic process is necessary. If intracranial extension is a concern, MRI is recommended, as MRI is better at soft tissue detail than CT. ,
Ultrasound (US)
Orbital US is an emerging imaging modality but currently is not used routinely in the evaluation of periorbital infection. ,
Imaging findings
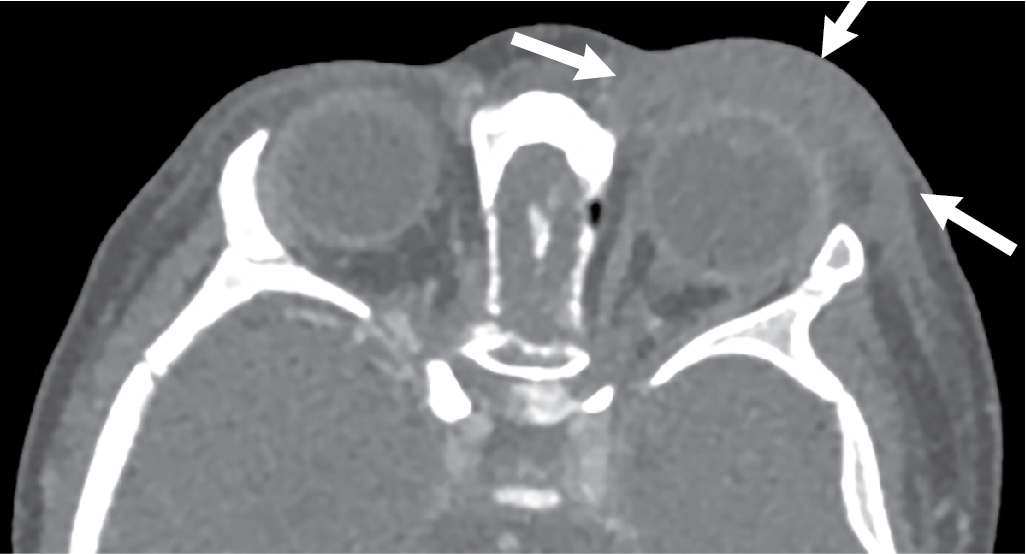
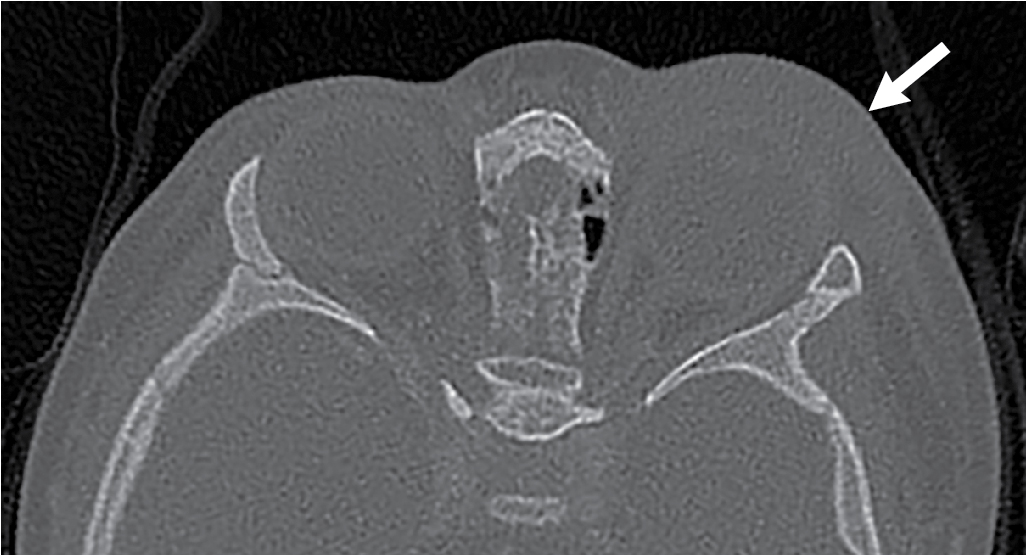
The physical examination findings were suggestive of a periorbital infection; however, the swelling was significant, hindering the ability to complete a thorough physical examination. After much discussion with the family, the decision was made to obtain an intravenous contrast–enhanced orbital CT. Selected images from this study are presented here. There is diffuse left preseptal periorbital soft tissue swelling with no sign of abscess, intraorbital, or intracranial involvement ( Figs. 35.1–35.3 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








