4 Sonographic Anatomy of the Breast and Axilla Anatomically the breast is a modified sweat gland lying within the deep and superficial layers of superficial pectoral fascia. Viewing a schematic sagittal section of the breast turned 90° to correlate with ultrasonographic positioning, we observe the following anatomic structures (from anterior to posterior), which can also be visualized with ultrasound (Tables 4.1, 4.2): skin, subcutaneous fat, Cooper ligaments, the superficial mammary fascia, the breast parenchyma (with ducts and lobules), interlobar fibrofatty tissue, the deep mammary fascia, retromammary fat, muscle fascia, the pectoralis major and minor muscles, the ribs and intercostal spaces, and finally the pleura and lung (Fig. 4.1). The breast consists of a varying mixture of tissue components, and its composition depends on age, hormonal influences, structural changes (congenital, degenerative, or pathologic), and individual characteristics (Tables 4.3, 4.4). As a general rule, the breast tissue of young women consists mostly of parenchyma and contains little fat. With aging, the glandular tissue of the breast is replaced by connective tissue and fat. But there is great individual variation, so that the breasts of young multiparous women who have nursed their infants are predominantly fatty, and even in young girls a substantial portion may consist of fat, especially if the breasts are large. Conversely, the breasts of older women who receive postmenopausal hormone replacement may respond by increasing fibro-glandular density, and many older women may have mammographically dense breasts, the density reflecting the fibrous (rather than glandular) predominance of their breast tissue. This should be considered in breast examinations as it will influence the overall interpretation of clinical, sonographic, and mammographic findings. The structural composition of the breast varies with age, functional status, and individual differences in tissue distribution and quantitative make-up. Fig. 4.1 Gross anatomy of the breast. PMa = pectoralis major muscle, PMi = pectoralis minor muscle.
Gross Anatomy
Breast
|
|
|
|
|
– Lobules |
– Lactiferous ducts |
– Interlobar connective tissue |
– Fat |
|
|
|
|
|
|
|
Anatomic structure | Echogenicity |
Skin | Hyperechoic |
Nipple | Hypoechoic |
Parenchyma | Hyperechoic |
Connective | tissue Hyperechoic |
Subcutaneous fat | Hypoechoic |
Fatty infiltration | Hypoechoic |
Retromammary fat | Hypoechoic |
Cooper ligaments | Hyperechoic |
Lactiferous ducts | Anechoic* |
|
|
– Alveoli |
– Lactiferous ducts |
– Intralobar connective tissue (hormonally responsive) |
|
|
|
– Young women |
– Good readability |
|
– Scant fatty infiltration |
– Middle-aged women |
– Good or moderate readability |
|
– Predominantly hypoechoic with connective-tissue septa |
– Older women |
– Moderate readability |
|
– Young and middle-aged women |
– Poor readability |
Parasternal Region
The internal thoracic artery descends on either side of the sternum (Fig. 4.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


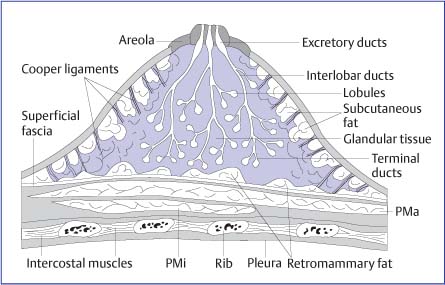
 Skin
Skin Subcutaneous fat
Subcutaneous fat Cooper ligaments
Cooper ligaments Superficial mammary fascia
Superficial mammary fascia Breast parenchyma with
Breast parenchyma with Deep mammary fascia
Deep mammary fascia Retromammary fat
Retromammary fat Muscle fascia
Muscle fascia Pectoralis major muscle
Pectoralis major muscle Pectoralis minor muscle
Pectoralis minor muscle Ribs and intercostal muscles
Ribs and intercostal muscles Pleura
Pleura Fat
Fat Parenchyma
Parenchyma Interlobar connective tissue
Interlobar connective tissue Axilla
Axilla Homogeneous hyperechoic pattern
Homogeneous hyperechoic pattern Heterogeneous hyperechoic pattern
Heterogeneous hyperechoic pattern Partially involuted or involuted pattern
Partially involuted or involuted pattern Fibrotic pattern (heterogeneously hypoechoic)
Fibrotic pattern (heterogeneously hypoechoic)